Medical expert of the article
New publications
premature pregnancy
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Post-term pregnancy is one of the problems that traditionally determines great scientific and practical interest, caused, first of all, by unfavorable perinatal outcomes in this pathology.
In domestic obstetrics, it is believed that a post-term pregnancy, lasting more than 287–290 days, is accompanied by intrauterine suffering of the fetus and ends with the birth of a child with signs of biological overmaturity, which determines the high risk of developing ante/intranatal distress syndrome and difficult neonatal adaptation.
Epidemiology
The incidence of post-term pregnancy is approximately 7% of all pregnancies (Martin et al., 2007).
The American College of Obstetricians and Gynecologists defines post-term pregnancy as one that lasts more than 42 weeks (294 days). Its incidence is on average about 10%. In most European countries, post-term pregnancy is defined as one that lasts 294 days or more, with the exception of Portugal (287 days or more) and Ireland (292 days or more). The incidence of post-term pregnancy in Europe is about 3.5–5.92%.
At the same time, a child with signs of postmaturity is not always born with postmaturity and, on the contrary, signs of postmaturity can be noted in a fetus born before the expiration of 290 days of gestation, which is probably due to individual timing and features of pregnancy development. However, the functional state of a postmature fetus deserves more attention, given the high frequency of occurrence of such serious complications as meconium aspiration syndrome, hypoxic-ischemic damage to the central nervous system, myocardium, kidneys, intestines, leading to ante- and intranatal death of the fetus.
Post-term pregnancy is considered a factor that increases the frequency of complications during childbirth and leads to an increase in perinatal morbidity and mortality. The most typical perinatal complications of post-term pregnancy are stillbirth, asphyxia and birth trauma. E. Ya. Karaganova, I. A. Oreshkova (2003), having conducted a thorough analysis of perinatal outcomes in 499 patients with post-term pregnancy depending on the gestational age, found that as the gestational age increases from 41 to 43 weeks, the proportion of perinatal morbidity increases. Thus, at 43 weeks of pregnancy, the frequency of hypoxic-ischemic CNS damage increases by 2.9 times, asphyxia - by 1.5 times, aspiration syndrome - by 2.3 times compared to full-term newborns with a gestational age of no more than 41 weeks. At a pregnancy term of more than 41 weeks, signs of fetal distress before the onset of labor were detected in 67.1% of fetuses (in half of them at a pregnancy term of 42–43 weeks), admixture of meconium in the amniotic fluid - in 31.6%, oligohydramnios - in 50.9% of patients.
Causes premature pregnancy
The most common cause of post-term pregnancy is inaccurate dating (Neilson, 2000; Crowley, 2004). The use of standard clinical criteria to determine the estimated date of delivery (EDD) tends to overestimate the gestational age and therefore increases the incidence of post-term pregnancy (Gardosi et al., 1997; Taipale and Hiilermaa, 2001). Clinical criteria commonly used to confirm gestational age include last menstrual period (LMP), uterine size assessed by first trimester bimanual examination, perception of fetal movements, auscultation of fetal heart sounds, and fundal height. singleton pregnancy.
When a post-term pregnancy does occur, the cause is usually unknown.
Risk factors
When analyzing the somatic, obstetric and gynecological anamnesis, and the characteristics of the current pregnancy, risk factors are noted that indicate the possibility of developing a post-term and prolonged pregnancy.
Risk factors for post-term pregnancy:
- the pregnant woman is over 30 years old;
- history of sexually transmitted infections (STIs) and chronic inflammatory diseases of the uterine appendages;
- indication of a history of late delivery;
- "immature" or "insufficiently mature" cervix at 40 weeks or more of gestation.
Risk factors for prolonged pregnancy:
- the age of the pregnant woman is from 20 to 30 years;
- dysfunction of the ovaries with irregular or prolonged (≥ 35 days) menstrual cycle;
- discrepancy between the gestational age determined by the first day of the last menstrual period and the ultrasound scan.
General risk factors include primiparity, previous post-term pregnancy (Alfirevic and Walkinshaw, 1994; Mogren et al., 1999; Olesen et al., 1999), male fetus (Divon et al., 2002), obesity (Usha Kiran et al., 2005; Stotland et al., 2007), hormonal factors, and genetic predisposition (Laursen et al., 2004).
It is not known how body mass index (BMI) affects pregnancy duration and delivery timing, but interestingly, obese women are more likely to experience post-term pregnancy (Usha Kiran et al., 2005), while women with low BMI have a higher risk of post-term pregnancy and preterm birth (delivery before 37 weeks of gestation) (Hickey et al., 1997). Since adipose tissue is hormonally active (Baranova et al., 2006) and obese women may have altered metabolic status, it is possible that endocrine factors involved in the onset of labor are altered in obese women.
Genetic factors may be associated with prolongation of pregnancy. Women who have themselves carried a post-term pregnancy have a higher risk of having a post-term pregnancy (relative risk of 1.3) (Mogren et al., 1999). Women who have had a previous post-term pregnancy have an increased risk of having a subsequent post-term pregnancy (27% with one previous post-term pregnancy and 39% with two previous prolonged pregnancies) (Kistka et al., 2007).
Pathogenesis
The pathogenesis of post-term pregnancy is not fully understood. As shown above, some risk factors associated with post-term pregnancy have been identified with some possible explanations, however, the pathogenesis of this condition is not yet clear. Despite the improvement in the understanding of labor in recent years, we still lack clarity regarding the exact mechanisms that initiate labor and promote its progression. To better understand the pathogenesis of post-term pregnancy, it is important to shed light on the pathophysiology of labor and try to understand why these mechanisms are not triggered in post-term pregnancy or, conversely, are triggered earlier in preterm labor. It seems logical that there is indeed a common basis or relationship between these three conditions. The mechanisms of labor involve the interaction between hormonal, mechanical and inflammatory processes in which the placenta, mother and fetus play a vital role.
Placental production of corticotropin-releasing peptide (CRH) is associated with the duration of pregnancy (McLean et al., 1995). Placental CRH synthesis increases exponentially as pregnancy progresses and peaks at the time of delivery. Women delivering preterm have a faster exponential growth rate than women delivering at term, whereas women delivering later have a slower growth rate (Ellis et al., 2002; Torricelli et al., 2006). These data suggest that postterm delivery is due to altered biological mechanisms regulating the duration of pregnancy. This may be due to a hereditary predisposition resulting from polymorphisms in genes in the physiological pathway linking CRH to delivery. It is also possible that the maternal phenotype may alter the response of maternal tissues to normal hormonal signals at delivery, as may occur in obese women.
CRH can directly stimulate the fetal adrenal gland to produce DHEA, a precursor of placental estriol synthesis (Smith et al., 1998). Maternal plasma CRH concentrations correlate with estriol concentrations (Smith et al., 2009). The CRH-induced increase in estriol increases more rapidly than estradiol levels in late pregnancy, resulting in an increased estriol to estradiol ratio that is thought to create an estrogenic environment in the last weeks of pregnancy. Concomitantly, the increase in maternal plasma progesterone that occurs during pregnancy slows down or even decreases in late pregnancy. This may be due to CRH inhibition of placental progesterone synthesis (Yang et al., 2006). Thus, the pregnancy-promoting (relaxation-promoting) effect of progesterone decreases as the labor-promoting (uterine contraction-promoting) effect of estriol increases. These changes in ratios have been observed in preterm, term singleton and twin pregnancies (Smith et al., 2009). The situation in postterm pregnancies is unknown.
Symptoms premature pregnancy
The symptom complex of an overripe fetus was first described by Ballantyne (1902) and Runge (1948), which is why it is called Ballantyne-Runge syndrome, including the absence of cheesy grease, dryness and maceration of the skin of the newborn ("bath" feet, palms), as well as in the groin and axillary folds, long nails, dense bones of the skull, narrow sutures and reduced sizes of fontanelles, greenish or yellowish coloration of the skin, fetal membranes, umbilical cord. Other observations indicate prolonged pregnancy.
Prolonged pregnancy, lasting more than 287 days, is not accompanied by fetal suffering and ends with the birth of a healthy child without signs of overmaturity. Thus, prolonged pregnancy is considered a physiological condition aimed at the final maturation of the fetus.
Complications and consequences
Post-term pregnancy is associated with increased fetal and neonatal mobility and morbidity, as well as maternal morbidity. These risks are greater than originally thought. In the past, the risks were underestimated for two reasons. First, earlier studies of post-term pregnancy were published before ultrasound became a routine method of defining pregnancy. As a result, many of the pregnancies included in the studies were not actually post-term. The second reason is related to the definition of stillbirth itself. Stillbirth rates have traditionally been calculated using pregnancies delivered at a given gestational age, rather than ongoing (unborn) pregnancies. This will reduce the stillbirth rate in post-term pregnancies, since once the fetus is delivered, it is no longer at risk of intrauterine fetal death (IUFD). Thus, the appropriate denominator is not all births at a given gestational age, but ongoing (unborn) pregnancies (Rand et al., 2000; Smith, 2001; Caughey et al., 2003).
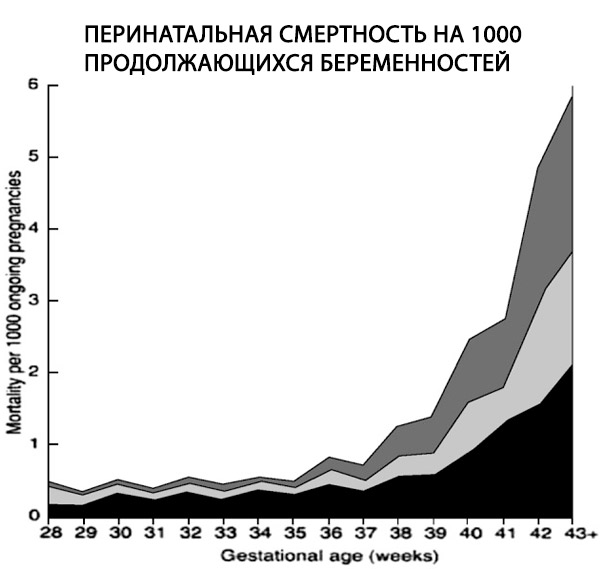
One retrospective study of over 170,000 singleton births using an appropriate denominator demonstrated a 6-fold increase in the stillbirth rate in postterm pregnancies from 0.35 to 2.12 per 1000 ongoing pregnancies (Hilder et al., 1998).
Complications in the fetus and newborn
Perinatal mortality, defined as stillbirths plus early neonatal deaths, is twice as high at 42 weeks of gestation as at term (4–7 versus 2–3 per 1,000 births, respectively). It increases fourfold at 43 weeks and five to sevenfold at 44 weeks (Bakketeig and Bergsjo, 1989; Feldman, 1992; Hilder et al., 1998; Cotzias et al., 1999). These data also show that, when calculated per 1,000 ongoing pregnancies, the fetal and neonatal mortality rates increase sharply after 40 weeks (Hilder et al., 1998) (Hilder et al., 1998).
Uteroplacental insufficiency, meconium aspiration and intrauterine infection are considered to be the main reasons for the increased perinatal mortality in these cases (Hannah, 1993).
Fetal morbidity is also increased in postterm pregnancies and pregnancies progressing beyond 41 weeks of gestation. This includes meconium passage, meconium aspiration syndrome, macrosomia, and dysmaturity. Postterm pregnancies are also an independent risk factor for low cord pH (neonatal acidemia), low 5-minute Apgar scores (Kitlinski et al., 2003), neonatal encephalopathy (Badawi et al., 1998), and infant mortality in the first year of life (Hilder et al., 1998; Cotzias et al., 1999; Rand et al., 2000). Although some of these infant deaths are clearly the result of perinatal complications such as meconium aspiration syndrome, most have an unknown cause.
About 20% of postterm fetuses have dysmaturity syndrome, which refers to neonates with features resembling chronic intrauterine growth retardation due to uteroplacental insufficiency (Vorherr, 1975; Mannino, 1988). These include thin, wrinkled, flaky skin (excessive scaling), thin frame (undernutrition), long hair and nails, oligohydramnios, and frequent passage of meconium. These pregnant women have an increased risk of umbilical cord compression due to oligohydramnios, meconium aspiration, and short-term neonatal complications such as hypoglycemia, seizures, and respiratory failure.
Maternal risks
Post-term pregnancy is associated with significant risks for the mother. The risk is increased:
- labor dystocia (9-12% versus 2-7% at full term);
- severe perineal lacerations (3rd and 4th degree lacerations) associated with macrosomia (3.3% versus 2.6% at full term);
- operative vaginal delivery; and
- doubling of the caesarean section (CS) rate (14% versus 7% at term) (Rand et al., 2000; Campbell et al., 1997; Alexander et al., 2000; Treger et al., 2002).
Caesarean section is associated with a higher incidence of endometritis, bleeding, and thromboembolic disease (Alexander et al., 2001; Eden et al., 1987).
Similar to neonatal outcomes, maternal morbidity also increases with term pregnancy up to 42 weeks of gestation. Complications such as chorioamnionitis, severe perineal lacerations, cesarean section, postpartum hemorrhage, and endomyometritis increase after 39 weeks of gestation (Yoder et al., 2002; Caughey and Bishop, 2006; Heimstad et al., 2006; Caughey et al., 2007; Bruckner et al., 2008;).
Diagnostics premature pregnancy
Traditional diagnostics of post-term pregnancy consists of adequate calculation of the gestational age. At the same time, the most accurate methods at the present stage include calculations based on the first day of the last menstruation and on ultrasound scanning data from 7 to 20 weeks of pregnancy. A number of authors consider these two methods equivalent. However, some researchers suggest relying solely on ultrasound biometry data when determining the gestational age in post-term pregnancy. Among the risk factors for post-term pregnancy, a number of features of the somatic, obstetric and gynecological anamnesis and the course of the current pregnancy are distinguished.
From the somatic anamnesis, many authors highlight the age of the parents over 30 years, the presence of extragenital pathology in the mother. Among the features of the obstetric and gynecological anamnesis, attention should be paid to menstrual dysfunction, the presence of abortions and spontaneous miscarriages, inflammatory diseases of the uterine appendages, a history of late births, and 3 or more upcoming births.
Laboratory diagnostics of post-term pregnancy
As the term of post-term pregnancy increases, progressive depletion of the kallekrein-kinin system occurs, manifested in extremely low kininogen content (0.25–0.2 μg/ml, with N=0.5 μg/ml), low activity of kallekrein, its inhibitors, and spontaneous esterase activity of blood plasma after 41 weeks of pregnancy.
In post-term pregnancy, intensification of lipid peroxidation processes is observed both in the pregnant woman's body and in the fetus's body, which contributes to the inhibition of membrane-binding enzymes of subcellular structures. As a result, detoxification and energy-producing functions are significantly impaired and, as a consequence, exogenous and endogenous toxic metabolites accumulate, endotoxemia develops, progressing as the pregnancy term increases. The intensity of endotoxemia can be assessed by the sorption capacity of erythrocytes and by the concentration of medium molecular proteins. An increase in peroxidation and endogenous intoxication correlates with the severity of fetal hypoxia.
Post-term pregnancy is characterized by a low content of prostaglandin F2α, which is synthesized in the decidua and myometrium and is the main modulator of the development of labor.
At a pregnancy term of more than 41 weeks, an increase in plasma viscosity, uric acid concentration, and a decrease in the concentration of fibrinogen, antithrombin III, and platelet count are noted. The concentration of fetal fibronectin > 5 ng/ml in the cervicovaginal secretion in women with a pregnancy term of more than 41 weeks indicates a high biological readiness of the body for labor and its spontaneous onset within the next 3 days. The sensitivity and specificity of this method are 71 and 64%, respectively.
It is extremely important to study the features of the functional state of the fetoplacental complex and the fetus in post-term pregnancy (ultrasound, Doppler and cardiotocographic studies). During the echographic study, fetometry is performed to determine the estimated weight of the fetus and assess its anatomical development. In 12.2% of cases, IUGR of I–II degrees is detected, which does not significantly differ from the frequency of detection of the syndrome in prolonged pregnancy. At the same time, in 80% of cases, we detected an asymmetric form of IUGR and in 20% - a symmetric form. Post-term pregnancy is characterized by the detection of echographic signs of pronounced involutional-dystrophic changes (GIII with petrifications). The average value of the amniotic fluid volume index in the post-term pregnancy group was 7.25±1.48, typical for post-term pregnancy is the detection of a reduced amount of amniotic fluid.
Doppler study
The most important factor for predicting perinatal outcomes is the determination of the stages of fetal hemodynamic disturbances during post-term pregnancy.
- Stage I - disturbance of intraplacental and fetoplacental blood flow. At this stage, there are no disturbances of arterial and venous fetal hemodynamics. An increase in vascular resistance is noted in the umbilical artery and its terminal branches, as well as in the spiral arteries. The indicators of the gas composition and acid-base balance of the umbilical cord blood are within normal limits.
- Stage II - centralization of fetal blood circulation. Hypoxemia is noted in the blood of the newborn at birth. At this stage, two successive stages are distinguished.
- IIa - initial signs of centralization of fetal arterial circulation with unchanged venous and intracardiac blood flow, characterized by:
- a decrease in resistance in the MCA (by no more than 50%) or an increase in vascular resistance in the aorta;
- reduction of the CPC (to 0.9);
- an increase in resistance in the renal arteries of the fetus by no more than 25% of the norm.
- IIb - moderately expressed centralization of blood circulation with impaired blood flow in the venous duct and increased blood flow rates on the aortic valve. At this stage, the following are detected:
- simultaneous increase in vascular resistance in the aorta and decrease in the middle cerebral artery;
- decrease in CPC;
- increase in the average blood flow velocity (Tamx) in the venous duct;
- increase in the average linear and volumetric blood flow velocity at the aortic valve.
- IIa - initial signs of centralization of fetal arterial circulation with unchanged venous and intracardiac blood flow, characterized by:
- Stage III - pronounced centralization of fetal circulation with impaired venous outflow and decompensation of central and intracardiac hemodynamics. Hypoxemia combined with acidosis and hypercapnia is noted in the umbilical cord blood of the newborn at birth. Dopplerometric indicators at this stage are characterized by:
- a decrease in vascular resistance in the SMA by more than 50% of the norm, a decrease in the CPC below 0.8;
- progressive increase in vascular resistance in the aorta and renal arteries by more than 80%;
- in the venous duct - an increase in the S/A ratio, PIV (more than 0.78) and a decrease in Tamx;
- in the inferior vena cava - an increase in PIV, IPI and %R (more than 36.8%);
- in the jugular veins - an increase in the S/A ratio, PIV (above 1.1) and a decrease in Tamx;
- a decrease in the average linear and volumetric velocity at the valves of the aorta and pulmonary trunk;
- increased heart rate, decreased stroke volume, left ventricular end-systolic and end-diastolic volumes, and cardiac output.
The identified stages of fetal hemodynamic changes reflect the consistent progression of its functional state disorders under conditions of chronic intrauterine hypoxia during post-term pregnancy. When hypoxemia combined with hyperacidemia and hypercapnia is detected in the umbilical cord blood of a newborn, the frequency of adverse perinatal outcomes is 4.8 times higher compared to the group with isolated hypoxemia. Consequently, hyperacidemia and hypercapnia reflect pronounced fetal metabolic disorders and progressive deterioration of its condition under conditions of chronic hypoxia during post-term pregnancy.
Cardiotocography
When conducting this method at stage I, initial signs of chronic intrauterine hypoxia (20.93%) and moderate fetal hypoxia (6.97%) are detected. At stage IIa, the frequency of initial signs of fetal hypoxia increased by 2 times, with moderate hypoxia - by 4.13 times. At stage IIb, the frequency of moderate and severe fetal hypoxia increases significantly. At stage III, only severe (65.1%) and moderate (30.2%) fetal hypoxia were detected.
The program of screening examination of pregnant women includes:
- identification of pregnant women at risk of post-term pregnancy;
- ultrasound fetometry with assessment of signs of maturity of the newborn;
- assessment of the quantity and quality of amniotic fluid;
- assessment of the degree of maturity of the placenta;
- cardiotocography;
- assessment of fetal hemodynamics (middle cerebral artery, aorta, venous duct, inferior vena cava);
- assessment of the biophysical profile of the fetus;
- assessment of cervical maturity;
- amnioscopy.
How to examine?
Differential diagnosis
During a comprehensive examination of women with prolonged pregnancy, the following is revealed:
- in 26.5% of observations - grade II, in 51.8% - grade III placental maturity;
- in 72.3% of observations - normal amount of amniotic fluid;
- in 89.2% of observations - normal indicators of fetal-placental blood flow and in 91.6% - normal cerebroplacental ratio;
- in 100% of observations - normal indicators of central hemodynamics of the fetus, its transvalvular and venous blood flow;
- a decrease in the CPC with normal indicators of fetoplacental and fetal blood flow indicates the presence of deviations in the functional state of the fetus and is characteristic of IUGR, intrauterine infection, and chronic fetal hypoxia.
Who to contact?
Treatment premature pregnancy
Accurate dating of pregnancy is critical for the diagnosis and management of post-term pregnancy (Mandruzzato et al., 2010). The last menstrual period has traditionally been used to calculate the expected date of delivery (EDD). However, many inaccuracies can exist due to cycle irregularity, recent use of hormonal contraception, or bleeding in early pregnancy.
Routine ultrasound screening for pregnancy has been shown to reduce the rate of false positive diagnoses and hence the overall rate of post-term pregnancy from 10-15% to approximately 2-5%, thereby minimising unnecessary interventions (Bennett et al., 2004; Caughey et al., 2008a; 2009).
The goals of treatment of post-term pregnancy are: correction of fetal hemodynamic disorders, prevention of fetal progression during labor, preparation of the birth canal for labor, induction of labor.
Indications for hospitalization
Exceeding the gestational age of 40 weeks 3 days with a precisely calculated date of birth, the presence of risk factors for post-term pregnancy, and insufficiently prepared birth canal.
Drug treatment of post-term pregnancy
To correct the condition of the fetus during post-term pregnancy, the drug hesobendin + etamivan + etofillin (instenon) is used - a combination drug with a neuroprotective effect based on the mutual potentiation of the effects of its components.
Indications for the administration of the drug hesobendin + etamivan + etofillin:
- impaired blood flow in the umbilical artery of the fetus (SDO > 2.7, IR > 0.65);
- decrease in cerebroplacental coefficient (CPC < 1.10);
- initial signs of centralization of fetal circulation;
- initial signs of fetal hypoxia according to CTG data. The listed factors indicating initial signs of fetal distress do not require emergency delivery, but indicate the need to correct its condition by increasing the adaptive capabilities of the fetal brain during labor.
Preparing for childbirth in post-term pregnancy
Mechanical methods of cervical irritation:
- Detachment of the lower pole of the fetal bladder. Detachment of the lower pole of the fetal bladder can also lead to increased synthesis of prostaglandins and "ripening" of the cervix. Detachment of the lower pole of the fetal bladder, performed daily or 2-3 times a week, helps prepare the cervix for labor and induce labor. This method is highly effective, easy to perform, has a low frequency of side effects, and is inexpensive. Its disadvantages include discomfort felt by the pregnant woman during the examination, rare bleeding, and the possibility of rupture of the fetal membranes.
- Balloon dilation of the cervix. For balloon dilation of the cervix, a Foley balloon catheter is used. It is inserted and inflated in the cervical canal. This method mechanically expands the cervical canal and enhances the synthesis of prostaglandins. Through the catheter, it is possible to introduce a saline solution into the extra-amniotic space, expanding the lower uterine segment and also facilitating the onset of labor.
- Mechanical dilators of natural and synthetic origin. To prepare the cervix for labor, cervical dilators of natural origin - laminaria and synthetic - dilapan, gipan, lamicel, are used, which are probes with a diameter of 2 to 4 mm and a length of 60-65 mm. Laminaria is made of natural material of the algae Laminaria japonicum. Synthetic dilators are created from chemically and biologically inert polymers with good hygroscopicity. The probes-dilators are inserted into the cervical canal in the required amount. Due to their hygroscopicity, they absorb the fluid contained in the cervical canal, significantly expand and exert radial pressure on the cervical canal. They mechanically open the cervix and facilitate the onset of labor. Synthetic dilators of the cervical canal do not cause discomfort and are well tolerated by patients. The limited use of synthetic dilators is associated with caution due to their long stay in the cervical canal, increasing the risk of ascending infection. The described mechanical methods of action on the cervix cause a response reaction of synthesis of endogenous prostaglandins E2 in the cervix, which contribute to a decrease in the amount and destabilization of collagen in its structure, having a relaxing effect on smooth muscles. In addition, prostaglandins E2 are considered dominant at the beginning of labor.
Medicines
Preparations of the prostaglandin E2 group are used. The most common, tested in practical obstetrics, medicinal means of preparing the cervix for labor and inducing labor include preparations of prostaglandins E2. Prostaglandins E2 are available in various dosage forms: in the form of gels for intracervical use, vaginal tablets and pessaries. The effectiveness of prostaglandins E2 in ripening the cervix and initiating labor reaches 80–83%. However, their use may result in the development of uncoordinated, violent labor and premature detachment of a normally located placenta. Consequently, prostaglandins E2 should be administered only in obstetric hospitals with mandatory cardiotocographic monitoring of fetal cardiac activity and uterine contractility.
Patient education
Necessarily:
- teaching women to keep a menstrual calendar to ensure the ability to accurately calculate the gestational age and the due date; counting fetal movements to promptly determine the risk of fetal hypoxia when its motor activity decreases or increases;
- informing the patient about the need for a thorough assessment of the condition of the fetus at a gestation period of more than 40 weeks 3 days and possible hospitalization in the presence of unfavorable prognostic factors.
Further management
Standard for examination and management of women with a pregnancy term exceeding 40 weeks:
- Conducting differential diagnostics of post-term and prolonged pregnancy.
Post-term pregnancy should be considered in the following cases: the first upcoming birth in a pregnant woman over 30 years old, a regular menstrual cycle, a history of STIs and chronic inflammatory diseases of the uterine appendages, indication of a late birth, compliance of the gestational age calculated based on the first day of the last menstruation and the ultrasound scan data performed between 7 and 20 weeks of gestation, in the presence of an “immature” or “insufficiently mature” cervix, detection of a placenta of stage GIII maturity or oligohydramnios during ultrasound.
Prolonged pregnancy is indicated by: the age of the pregnant woman from 20 to 30 years; dysfunction of the ovaries with an irregular or prolonged (> 35 days) menstrual cycle; discrepancy between the gestational age determined by the first day of the last menstruation and ultrasound scanning; detection of a “mature” cervix; placenta of GI and GIII maturity without petrifications and a normal amount of amniotic fluid during ultrasound.
- To correctly assess the condition of the fetus and prevent adverse perinatal outcomes, all pregnant women with a gestation period of more than 40 weeks must undergo Doppler ultrasound examination of the arterial hemodynamics of the fetus.
- If fetal hemodynamics are unchanged, the body is prepared for childbirth using estrogens, intracervical administration of prostaglandin E2 gel with dynamic CTG control (daily) and monitoring of the state of fetal blood flow (every 3 days).
- When centralization of blood circulation is detected, a study of venous blood flow and intracardiac hemodynamics is indicated to clarify the compensatory capabilities of the fetus and select the method and timing of delivery.
- During post-term pregnancy, fetal hemodynamics change in stages:
Stage I - disturbances of intraplacental and fetoplacental blood flow. At this stage, there are no disturbances of arterial and venous fetal hemodynamics. An increase in vascular resistance is noted in the umbilical artery and its terminal branches, as well as in the spiral arteries. The indicators of the gas composition and acid-base state of the umbilical cord blood are within normal limits.
Stage II - centralization of fetal circulation. Hypoxemia is noted in the newborn's blood at birth. At this stage, two successive stages should be distinguished:
- IIa - initial signs of centralization of fetal arterial circulation with unchanged venous and intracardiac blood flow;
- IIb - moderately pronounced centralization of blood circulation with impaired blood flow in the venous duct and increased blood flow velocity in the aortic valve.
Stage III - pronounced centralization of fetal circulation with impaired venous outflow and decompensation of central and intracardiac hemodynamics. In the umbilical cord blood of the newborn at birth - hypoxemia combined with acidosis and hypercapnia.
- If a decreased CPC (< 1.1), centralization of fetal hemodynamics (initial centralization: SDO in the MCA < 2.80; in the Ao > 8.00) with an increase in the average blood flow velocity in the venous duct (moderate centralization: SDO in the MCA < 2.80; in the Ao > 8.00; Tamx in the VP > 32 cm/s), initial signs of fetal hypoxia according to CTG data are detected, intravenous administration of hesobendin + etamivan + etofillin is indicated in terms of prenatal preparation to increase the adaptive capacity of the fetal brain.
- In case of initial centralization (SDO in the MCA < 2.80; or in the fetal aorta > 8.00) in the presence of good biological readiness of the body for childbirth, uncomplicated obstetric and gynecological history, average fetal size, programmed delivery through the natural birth canal after amniotomy under careful cardiac monitoring of the fetal cardiovascular system is possible. Lack of biological readiness of the body for childbirth, aggravated obstetric and gynecological history, large fetal size dictate the need for delivery by planned cesarean section.
- In case of moderately expressed centralization of fetal hemodynamics (SDO in the MCA < 2.80 and in the aorta > 8.00; Tamx in the VP > 32 cm/s) due to the tension of all compensatory mechanisms of the fetus and the absence of reserve capabilities for labor, delivery by cesarean section is indicated on a planned basis.
- Detection of disturbances in both the arterial and venous channels of fetal blood flow (marked centralization: SDO in the MCA < 2.80 and in the aorta > 8.00; in the VPr S/A > 2.25, PIV > 1.00; in the IVC %R > 16%, PIV > 1.2) in combination with moderate or severe fetal hypoxia according to CTG data indicates decompensation of fetal hemodynamics and requires delivery by emergency cesarean section.
Prevention
- Identification of a risk group for post-term pregnancy among women seeking antenatal care.
- Prevention of placental insufficiency and large fetus.
- Careful calculation of the pregnancy period and date of birth, taking into account the date of the last menstrual period (with a regular menstrual cycle) and an ultrasound scan performed before 20 weeks of pregnancy.
- Timely hospitalization of a pregnant woman to prepare the birth canal for childbirth and assess the condition of the fetus.
Forecast
With timely and thorough assessment of the fetus's condition and adequate obstetric tactics, the prognosis is favorable. The indicators of physical and neuropsychic development of children do not differ from those in uncomplicated timely births. However, with the development of complications, especially severe fetal hypoxia, birth trauma, meconium aspiration, the prognosis is less favorable. Perinatal losses are up to 7%, hypoxic-ischemic damage to the central nervous system - up to 72.1%.


 [
[