Medical expert of the article
New publications
Leukoplakia vulva: what is it, how to treat the disease?
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Vulvar leukoplakia is currently the number one problem, as it is a common condition in women and can be a precancerous condition. This problem should be diagnosed at the initial stages, in which case the prognosis is more favorable. Therefore, every woman should know the symptoms and manifestations.
Epidemiology
Statistics on the prevalence of leukoplakia among women indicate that the percentage of affected cases is estimated at 1-3%. Leukoplakia is more common with age, usually not occurring before the age of 30. Mortality from the pathology itself is not determined, but the degree of malignancy depends on the form and can reach 56%.
Causes vulvar leukoplakia
There are many recognized conditions that involve white lesions on the vulvar mucosa, but most of these spots have no known cause. They are called leukoplakia when other possible causes have been ruled out. There are also several recognized subtypes of leukoplakia, described according to the clinical appearance of the lesion.
Almost all such spots are usually the result of keratosis. Normal vulvar mucosa is red-pink in color due to the underlying vascular network in the lamina, which is visible through the thin epithelial layer. Almost all white spots are benign, that is, non-cancerous, but leukoplakia has a high potential for transformation into a malignant form, which must be taken into account.
Interest in vulvar disease has increased significantly in the last few years. The vulva is part of the female genital tract. Embryologically, it is the result of the union of the cloacal endoderm, urogenital ectoderm, and paramesonephric mesodermal layers. Various epithelia, from keratinized squamous epithelium to squamous mucosa, line the vulva. The vestibular epithelium is neither pigmented nor keratinized, but contains eccrine glands. This is important for understanding the development of leukoplakia pathogenesis.
Benign vulvar disorders are a serious problem for women of all ages. These disorders include vulvar atrophy, benign tumors, hamartomas and cysts, infectious disorders, and neoplastic epithelial disorders. Infectious disorders include those caused by known transmissible agents such as viruses, bacteria, fungi, and protozoa. They may be initially seen by physicians from different specialties, including dermatologists and gynecologists, and often require a multidisciplinary approach. All of these pathologies may be associated with or may trigger the development of leukoplakia.
Developmental abnormalities of the vulva are usually rare. Vulvar atrophy may be associated with old age or other disorders, but these abnormalities are often a nearly physiological finding in older people. Leukoplakia may often develop against a background of atrophy.
The exact causes of leukoplakia are not clear. However, the following factors are possible:
- Systemic factors such as diabetes, endocrine disorders, malnutrition, vitamin deficiency, dysfunction of the pituitary-ovarian system. Also an important role in the development of leukoplakia is played by a viral infection, Candida albicans, HPV infection is observed in 22% of patients. Mutation of the p53 gene is one of the causes leading to abnormal cell proliferation.
- Local factors such as: excessive thermal stimulation, chafing, age-related atrophy, mucosal damage or ulcers.
Pathogenesis
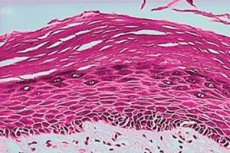
The pathogenesis of leukoplakia is the excessive growth of abnormal cells. It is a proliferative lesion of the mucous membrane or epidermal epithelium. Normal epithelium of the vulvar mucosa does not contain a stratum corneum and a granular layer. In leukoplakia, the epithelium of the mucous membrane becomes significantly keratinized. In leukoplakia, the epithelium of the mucous membrane becomes keratinized within the thickness of the granular layer in a place where there should normally be no keratin. First, due to the action of a pathological factor on the vulvar mucosa, epithelial hyperplasia of the mucosa occurs in order to restore the damaged layer (this is why leukoplakia so often occurs against the background of erosions or cracks). After this, acanthotic thickening of the epithelium and infiltration of dermal lymphocytes and plasma cells occur. This leads to thickening of the granular layer and significant hyperkeratosis with the subsequent appearance of irregularly shaped cells and mitotic figures, which may become the basis for a further neoplastic process.
Many people wonder whether vulvar leukoplakia is contagious. Since it is a non-infectious disease, it is not transmitted to men and is not contagious. The only thing is that if a woman has concomitant bacterial, fungal or viral sexually transmitted infections, only they can be transmitted.
Symptoms vulvar leukoplakia
Vulvar leukoplakia is relatively uncommon and may present with nonspecific clinical signs.
The first signs of the disease are the appearance of formations on the mucous membrane in the form of white-pink or grayish-white spots that have clear contours. The sizes are often different and the distribution is different. Usually, the appearance of these pathological formations does not give the woman any sensations. Therefore, the first signs of the progression of the disease can be seen only during a doctor's examination for a completely different reason.
Symptoms may, however, occur in some women, and this can be considered a lucky chance, as the chances of early detection are high.
Early symptoms may include genital itching, unusual discharge or more discharge. Sometimes there may be a burning or heaviness sensation, vulvodynia.
Late symptoms are a local burning sensation with a significant spread of the leukoplakia area, tingling and itching, local mucous membrane of the skin with varying degrees of pigment loss, often with edema, cracked and scattered superficial ulcers. Visually, the woman herself cannot see the manifestations of the disease, she can only suspect due to the appearance of some symptoms.
On visual examination, the symptom of white thickened infiltrative epithelium with transparent borders can be seen, and small fragments of erosions and ulcers are also possible. Skin lesions occur in the vaginal mucosa, urethral mucosa, clitoris, inside and outside the labia in the form of one or more irregular white and milky-white spots or plaques, slightly raised above the entire mucous surface. Some of them may not bulge, but the surface of the keratosis is rough and, touching this spot, for example, when scraping the surface of the mucous membrane, the base bleeds easily. The area of leukoplakia can usually bleed due to scratching or friction, there may be erosion or lichenification.
Leukoplakia of the vulvar cervix is more difficult to diagnose, since the small spot may not be noticeable visually. But this location has a higher risk of malignancy. Symptomatically, leukoplakia of the cervix can bleed frequently, may cause more symptoms of discomfort than in other places.
Kraurosis, like vulvar leukoplakia, is considered one of the potentially carcinogenic conditions. Kraurosis develops in older women and is accompanied not only by thickening and hyperkeratosis of the epithelium, but also by the formation of sclerotic areas that are no longer amenable to conservative treatment. In essence, these are two different diseases that have histological differences, but leukoplakia can also potentially become sclerotic.
Vulvar leukoplakia in children is rare, occurring primarily in young prepubertal girls. It generally involves the skin of the vulva (the area surrounding the opening of the vagina), but can sometimes also involve the anus. In children, leukoplakia is dangerous and symptoms typically occur for months or years before the condition is diagnosed.
The most common symptoms that girls with leukoplakia experience are itching and soreness. These symptoms can range from mild to severe. Girls may react or express their discomfort in different ways. For example, some girls may simply complain that their “private area” is sore or itchy, while others may react by holding the genital area or rubbing and scratching it. The degree of discomfort may be out of proportion to the amount of disease present. The most important thing is that the girl feels comfortable talking about the symptoms.
Leukoplakia in children can also cause painful urination, and even constipation. Painful urination occurs when urine passes through the skin of the vulva, which may be irritated and inflamed. Constipation occurs from holding in stool due to painful cracks in the skin near the anus.
Stages
The stages of leukoplakia are difficult to track clinically, and one can only assume that the types of leukoplakia are successive stages of one process. A distinction is made between flat and hyperkeratotic leukoplakia. Flat leukoplakia of the vulva is characterized by the formation of whitish areas that do not protrude above the skin. They may be barely noticeable and are often asymptomatic. Warty leukoplakia of the vulva is the formation of dense areas that rise above the surrounding mucosa and can be of different sizes. Because of this, such areas can be injured and are often accompanied by bleeding or other symptoms.
 [ 18 ]
[ 18 ]
Complications and consequences
The consequences that may be experienced by all women are very different. The most common complication is sclerosis. The sclerosis virus is a common complication of vulvar and perianal leukoplakia. There is atrophy of the mucous membrane at the site of leukoplakia, and the mucous membrane gradually becomes thinner, which is mainly due to long-term vulvar leukoplakia caused by the body's own immune dysfunction.
Some cases of vulvar leukoplakia may be complicated by diabetes and the effects of these factors are mutual. Vulvar leukoplakia gradually increases the condition, which can lead to endocrine disorders, induced diabetes and an increase in the degree of vulvar damage.
Irregular menstruation may be a consequence of leukoplakia, both with endocrine disorders, clinically diagnosed and requiring treatment.
 [ 19 ]
[ 19 ]
Diagnostics vulvar leukoplakia
The main diagnosis is based on histopathological examination and clinical manifestations. If there are epithelial or epidermal changes in the mucous membrane, it is easier to diagnose the problem. However, the diagnosis of leukoplakia is often diagnosed at a late stage.
The diagnosis of leukoplakia is also based on the results of a gynecological examination, the presence of complaints in patients. The tests used for this pathology are a clinical blood test, an immunogram, and a cytological examination of smears from the affected area.
Instrumental diagnostics of leukoplakia includes colposcopy (taking smears from pathological foci for further examination using a microscope), biopsy, ultrasound, and Schiller test.
When a doctor finds a white spot on the mucosa, he can only assume that it is an area of leukoplakia. A biopsy and histological examination are needed for confirmation. Microscopic examination of keratinocytes taken from an area of the vulva, cleared of the mucosa, is used as a diagnostic. Usually, a tissue biopsy is performed to exclude other causes of white spots, as well as to allow for a detailed histological examination and to assess the presence of any epithelial dysplasia. This is an indicator of malignant potential and usually determines the management and return interval. The areas of leukoplakia lesions that are preferentially biopsied are areas that show induration (hardening) and erythroplasia (redness), as well as erosive or ulcerated areas. These areas are more likely to show dysplasia than homogeneous white areas.
Histologic examination is mandatory after microscopy to exclude cellular atypia (cancer). Leukoplakia has a wide range of possible histologic appearances. The degree of hyperkeratosis, epithelial thickness (acanthosis/atrophy), dysplasia, and underlying lamina propria inflammatory cell infiltration may vary. In mucous membranes, hyperkeratosis can be defined as an increase in the thickness of the keratin layer of the epithelium or the presence of such a layer in a location where it is not normally expected. In leukoplakia, hyperkeratosis varies in thickness and may be either ortho- or para-keratosis (depending on whether cell nuclei are lost or preserved) or a mixture of both in different areas of the lesion. The epithelium may show hypertrophy (eg, acanthosis) or atrophy. The red areas in leukoplakia represent atrophic or immature epithelium that has lost the ability to keratinize. The transition between the lesion and the normal surrounding mucosa may be well demarcated or poorly defined. Hyperkeratosis and altered epithelial thickness may be the only histologic features of a leukoplakia lesion, but some exhibit dysplasia. The word dysplasia generally means "abnormal growth" and, specifically in the context of vulvar lesions, refers to microscopic changes ("cellular atypia") in the mucosa that indicate a risk of malignant transformation. Inflammatory cell infiltration in lamina samples is usually seen in the presence of dysplasia. Severe dysplasia is synonymous with the term carcinoma in situ, indicating the presence of neoplastic cells that have not yet penetrated the basement membrane or invaded other tissues. This is why it is so important to not only perform a histologic examination of leukoplakia but also to make the diagnosis in a timely manner, as it may sometimes already be an early stage of cancer.
 [ 20 ]
[ 20 ]
Differential diagnosis
The differential diagnosis of leukoplakia can be considered in accordance with the appearance of similar spots on the vulvar mucosa, which in appearance may resemble leukoplakia.
Leukoplakia cannot be wiped off the mucosa, which distinguishes it from white patches such as pseudoseminal candidiasis, where the white layer can be removed to reveal an erythematous, sometimes bleeding surface. The white color associated with leukemia disappears when the mucosa is stretched. Other causes of white patches usually require pathological examination of a biopsy specimen to differentiate them from leukoplakia.
Atrophic areas of the vulva may superficially resemble leukoplakia. Common mucosal leukoplakia is a hypertrophic dystrophy of the vulva, usually not accompanied by vulvar atrophy, histopathology of thickening of the epidermal layer, heterogeneity of cells and atrophy of hardening. In contrast, atrophic dystrophy of the vulva appears as a skin lesion in the form of atrophic blue and white flat spots that have complete degeneration of dermal collagen fibers, the bottom of the inflammatory cell infiltration, which can be identified.
Leukoplakia also needs to be differentiated from vulvar dermatitis. Vulvar dermatitis is white spots distributed on both sides of the labia, itchy, often accompanied by lesions of other parts of the skin, skin pigmentation lesions, histopathological changes of chronic dermatitis, thickening of the skin layers.
Treatment vulvar leukoplakia
A systematic review found that none of the treatments commonly used for leukoplakia were effective in preventing malignant transformation. Some treatments may result in healing of leukoplakia, but do not prevent recurrence of the lesion or malignant change. Regardless of the treatment used, a diagnosis of leukoplakia almost always results in a recommendation that possible causative factors should be eliminated, as well as long-term follow-up of the lesion to detect any malignant changes early. However, medications are used on a case-by-case basis.
Many different topical and systemic agents have been studied, including anti-inflammatory agents, antifungals, carotenoids (precursors to vitamin A, such as beta-carotene), retinoids (vitamin A-like agents), and cytotoxic agents. Vitamins C and E have also been studied in relation to the treatment of leukoplakia. Some of these studies are based on the hypothesis that antioxidant nutrients, vitamins, and cell growth suppressor proteins (such as p53) are antagonists of tumorigenesis. High doses of retinoids may cause toxic effects.
Local treatment is one of the priorities and also includes some care recommendations.
- Keep the vulva clean and dry, avoid excessive cleaning with soap, etc. Itching can be significantly reduced when using topical corticosteroids such as hydrocortisone ointment, hydrocortisone oil cream. Hydrocortisone suppositories are recommended for local use. The method of application is intravaginal, the dosage is one suppository per night in the vagina, no more than seven days. Side effects may include the development of candidiasis, since suppositories slightly suppress local immunity.
- Terzhinan is used for vulvar leukoplakia when a woman has a concomitant bacterial or fungal infection, or candidiasis, which could cause this problem. This is a complex drug that includes an antibacterial agent (ternidazole and neomycin), an antifungal agent (nystatin) and a hormonal agent (prednisolone). The method of application is intravaginal in the form of suppositories, the dosage is one suppository once a night for six days in a row. Side effects are not common, there may be a burning sensation after the introduction of the drug, itching.
- Ointments and creams for vulvar leukoplakia are used as a local therapy. Iranian saffron cream is one of the effective, according to user reviews, products. The product contains several types of Chinese herbs without adding hormonal drugs and synthetic drugs. The product consists of a set of gel and cream. How to use - first wash with gel, then dry with a towel and apply cream. Side effects are not determined.
- Ointment 999 is a complex preparation that contains camphor, menthol, biologically active herbs, and the antimicrobial hormonal agent hexamethasone. The preparation has an anti-inflammatory and antibacterial effect. Method of application of the preparation - in the form of a cream, it should be applied to the area of leukoplakia. Dosage - a small amount once a day. There may be difficulties with the use of the preparation due to the inconvenience of self-use. Precautions - if there are areas with erosions or damage, then it is not recommended to use the ointment.
Fenistil is not particularly effective for treating vulvar leukoplakia, but as an antihistamine, it can relieve or reduce itching.
Vitamins are used in complex therapy, since leukoplakia is considered one of the pathologies of hypovitaminosis. You can give preference to any multivitamin complexes - Kvadevit, Supervit, Vitrum.
Physiotherapy treatment is not widely used because additional external irritation or stimulation may cause complications.
Folk remedies
Traditional methods of treatment have not been proven effective, and it has not been proven that such methods may not cause the onset of malignancy. Therefore, it is better to use such methods only after consulting a doctor.
- To prepare the medicine, take 30 g of Sophora, 12 g of Nepeta, 6 g of red peony, 6 grams of safflower, 20 g of astragalus. Everything needs to be steamed with hot water and made into a bath. You can take such baths 2 times a day, each dose of steamed grass can be used 2-4 times.
- You can make the ointment at home. For this you need 20% fish oil ointment 20 g, 10 g dexamethasone, 5-fluorouracil and if indicated, you can add hydrocortisone ointment. After mixing, you need to apply it to a cotton swab and make such suppositories once a night for seven days.
- For the following infusion you need 30 grams of deer grass, 30 grams of alcohol spleen, 15 grams of cicada. Mix everything and make a bath, straining the contents. Take such a hot bath twice a day to treat vulvar leukoplakia.
Hirudotherapy for vulvar leukoplakia is widely discussed as one of the methods of alternative treatment of the disease. The effect of such a procedure is not clear, but some women notice a reduction in symptoms after several procedures. For such treatment, a special center is needed that deals with pathology and uses proven methods with ecological types of leeches.
Homeopathy can be used, but you should not attach great importance to this type of therapy, since complications can be missed. It is not recommended to use homeopathic methods on your own.
Surgical treatment of leukoplakia is the first choice of treatment for many clinicians. However, the effectiveness of this treatment cannot be assessed due to insufficient evidence available. It can be performed by traditional surgical excision with a scalpel or by laser or cryotherapy. Often, if a biopsy shows moderate to severe dysplasia, then the decision to use a surgical approach is more readily made. Sometimes the white spots are too large to be completely removed and are instead carefully monitored. Even if the lesion is completely removed, regular check-ups are essential as leukoplakia may recur, especially if predisposing factors such as infection persist.
Laser treatment of vulvar leukoplakia is considered the least invasive method. It is used if the lesion is small. When women do not want to take risks and think that leukoplakia may become malignant, laser treatment may be the solution.
Extirpation of the vulva is not performed in the case of leukoplakia itself. Such radical treatment can be chosen when there are serious complications with the development of cancer.
Nutrition and diet are of great importance for vulvar leukoplakia. A woman's diet should be as full of vitamins, minerals, and fiber as possible. Normal functioning of the immune system is impossible without sufficient protein, and therefore nutrition should be complete without harmful fats. Women with such a diet have a lower risk of developing leukoplakia, and if it already exists, the risk of complications is also lower.
Prevention
Prevention of this pathology is based on the correct regime of the woman, the regime of not only nutrition, but also sexual life and hormonal background. It is always necessary to undergo preventive examinations on time to exclude risk factors for the development of leukoplakia.
Vaccination against vulvar leukoplakia as a disease has not been developed. But there is a vaccine against the papilloma virus, which can cause cancer in women, especially if there is leukoplakia. A woman should get this vaccine before starting sexual activity.
Outpatient observation of vulvar leukoplakia is mandatory until it is cured or surgical intervention is performed. Even after surgical treatment, the woman is actively observed for this pathology for another year.
Forecast
The prognosis of leukoplakia depends on many factors - age, hormonal background, infections, type of pathology. For example, mixed red and white lesions (erythroleukoplakia / "spotted leukoplakia") have a higher risk of malignant changes than homogeneous leukoplakia. Older women with leukoplakia are also at higher risk. In general, spontaneous regression of spots occurs, and their disappearance occurs against the background of complex therapy. The most favorable prognosis for recovery is the use of invasive diagnostic methods.
Vulvar leukoplakia should not be a common problem for a woman, because it is one of the conditions that needs to be controlled. And although leukoplakia is often asymptomatic, it is important to undergo preventive examinations with a gynecologist regularly to detect this pathology.

