Medical expert of the article
New publications
Leishmanias
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
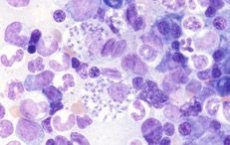
Leishmania is a causative agent of a protozoan infection that causes damage to the outer skin or internal organs (disease - leishmaniasis ).
Leishmania is a family of trypanosomids (from the order of protomonadids), class of flagellates, type of protozoa. It is an intracellular parasitic microorganism that develops in the body of certain insects, and through them is transmitted to humans or animals.
Leishmania are recognized as the causative agents of internal and cutaneous leishmaniasis, a severe infectious disease that occurs with ulcerative damage to the skin and/or internal organs.
Structure of Leishmania
Leishmania can be represented by two forms – intracellular amastigote and promastigote (flagellate form).
The amastigote has a rounded outline, from 2.5 to 5 µm in diameter, and is located in the middle of the parasitophorous vacuole of the macrophage. A clearly defined nucleus and kinetonucleus are observed, and it is distinguished by vacuolated cytoplasm and the presence of lysosomes. The outer membrane contains a polysaccharide component, but without a glycocalyx layer.
The promastigote is the presence of a clearly defined flagellum. The outer membrane contains binding molecules like glycoproteins and special cells of the immune system - mannose receptors. All this plays a major role in penetrating the macrophage. This process is facilitated by the binding of plasma antibodies to the promastigote.
Leishmania is located in the cellular protoplasm of internal organs - this can be the liver, kidneys, lungs, spleen, as well as skin and mucous membranes, capillaries, etc. An affected cell can contain from one to two hundred leishmania.
Life cycle of Leishmania
Leishmania are representatives of trypanosomatids, which means that they belong to obligate parasites. The life cycle of Leishmania is determined by the presence of two successive hosts: an insect and a vertebrate.
Insects become infected with leishmania when they suck the blood of the host animal. The parasites enter the insect's digestive organ with the blood: in the midgut, around the perimeter of the swallowed blood, the so-called peritrophic matrix is formed.
The promastigote form of the parasite reproduces in the digestive organ of female insects. After about 7 days, the infection reaches the upper part of the digestive system. In this case, leishmania completely block the female's digestive organ. When the insect bites a mammal, its saliva, together with clusters of parasites, penetrates the bite site into the skin of the new host.
As a rule, neutrophils, immune blood cells, rush to the site of damage and capture the parasites. The parasites exist inside the cells until the time comes for the natural death of the neutrophils. After this, the leishmania are released and freely enter the mammal's blood.
Leishmania life cycle
When settling inside the human body or in the body of other mammals, leishmania can be localized in the bloodstream and in the outer coverings. Mosquitoes or gnats, having sucked out particles of blood from a sick animal or person, are affected by leishmania.
Already on the first day, the swallowed flagellate parasite transforms into a mobile flagellate form. It enters the reproduction stage and after about a week, in the form of clusters, it ends up in the upper sections of the insect's digestive tract.
With the bite of an infected insect, active leishmania penetrates into a microscopic wound, and from there into the cellular structures of the skin, or through the bloodstream to the internal organs: this depends on the type of leishmania (cutaneous or visceral leishmania).
Cutaneous leishmania - at the site of the insect bite, leishmania begins to multiply and nodules (leishmaniomas) form, which are infiltrates containing macrophages, endothelial cells and lymphoid tissue, as well as fibroblasts. Subsequently, the nodes die off, and an ulcerative process with signs of edema and keratinization forms in their place: after healing, the ulcer is replaced by scar tissue.
Visceral leishmaniasis - at the site of the insect bite, a node is formed, from which the parasites are distributed through the bloodstream to all internal organs (spleen, lymph nodes, liver, etc.). There, secondary foci of infection spread are formed, which leads to proliferative changes in organ tissues, hyperplasia with further development of the dystrophic and necrotic process.
Symptoms of Leishmania
Symptoms of leishmania may vary in different geographical areas, but some clinical manifestations are characteristic of all regions. Among the local population, children under 5 years of age are most vulnerable. Visitors can get sick regardless of age category.
The disease begins gradually or acutely. The most characteristic symptom is prolonged intermittent fever, accompanied by chills, heat, frequent rises and falls in temperature. The spleen and liver enlarge and harden. Damage to the large intestine manifests itself in the form of diarrhea, malabsorption syndrome. Anemia and thrombocytopenia are observed, indicating damage to the bone marrow. A characteristic rash - leishmanoids - may appear on the skin. In the future, purulent infection may develop, sepsis, increased bleeding syndrome or thrombus formation, and ulcers in the oral cavity may appear.
Visceral leishmania usually manifests itself 3-10 months after infection. The disease begins with weakness, fatigue, headaches and muscle pain. Then there is increased sweating (at night), dyspeptic disorders, signs of anemia. In childhood, the disease is more severe and can lead to death after a few months. In adult patients, the disease can last for several years.
Cutaneous leishmaniasis can develop 1-6 months after infection. At first, a progressive node (1-1.5 cm) appears on the skin, which subsequently turns into an ulcerative process. The nodes can spread and also gradually turn into an ulcer. Ulcers heal extremely slowly (up to several months), after healing, scar tissue remains. In addition to nodes, papules can form like acne.
Types of Leishmania
Three species of Leishmania are identified that tend to parasitize the human body:
- Leishmania tropica – causes the development of cutaneous leishmaniasis. This type of parasite was identified in the 19th century by the physician and scientist P. Borovsky;
- Leishmania brasiliensis – was first discovered in the regions of South America and causes the development of mucocutaneous (American leishmaniasis);
- Leishmania donovani - affects internal organs, causing the development of the visceral form of the disease. In turn, Leishmania donovani can be divided into Mediterranean and Indian kala-azar, depending on the geographical location of the infection site.
Leishmania prevention measures
In regions with a high risk of the disease, measures are taken to prevent leishmania. Preventive measures include:
- early detection, isolation and therapy of patients with suspected leishmania;
- isolation and destruction (or treatment) of sick dogs, control of jackals, foxes, and gerbils within a one and a half kilometer zone from residential buildings;
- mosquito control (disinsection);
- use of methods of protection against mosquito attacks (nets, hats, clothing);
- Carrying out vaccinations (vaccines with live cultures of Leishmania), especially for visiting people.
Leishmania is a pressing problem for residents of Asian, African, Mediterranean and South American countries, especially in rural areas of these geographic zones.


 [
[