Medical expert of the article
New publications
Labyrinthitis (inflammation of the inner ear).
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Labyrinth (otitis media, inflammation of the inner ear) is an inflammatory disease of the inner ear that occurs as a result of the penetration of pathogenic microorganisms or their toxins and is manifested by a combined dysfunction of the peripheral receptors of the vestibular and auditory analyzers.
Epidemiology
According to summary statistics, by the end of the 1950s, otogenic labyrinthitis accounted for 1.4-5.4% of the total number of purulent otitis media. Given that the greatest number of cases of labyrinthitis is associated with inflammation of the middle ear, prevention is timely diagnosis and effective treatment of otitis media, which mainly affects children. Middle otitis in the gums is the result of the transition of the inflammatory process from the nasopharynx and pharynx through the auditory tube into the middle ear cavity. Thus, careful sanitation of the nose, nasopharynx and pharynx is a preventive measure among their otitis and otogenic complications.
Causes labyrinthitis
Labyrinthitis can be caused by various viruses, bacteria and their toxins, trauma. The source of infection is most often an inflammation center in the middle ear cavities or skull located in close proximity to the labyrinth (acute and chronic otitis media, mastoiditis, cholesteatoma, petrositis). In purulent inflammation of the middle ear, the infection penetrates the labyrinth.
The dominant role belongs to bacteria - streptococcus, staphylococcus, mycobacterium tuberculosis. The causative agent of meningogenic labyrinthitis is meningococcus, pneumococcus, mycobacterium tuberculosis, pale treponema, influenza and mumps viruses.
Pathogenesis
Various factors are important for the development of labyrinthitis: general and local reactivity of the organism, the nature and degree of virulence of the pathogen, the features of the manifestation of the inflammatory process in the middle ear and cranial cavity, the routes of infection penetration into the inner ear. The following types of infection penetration into the inner ear are distinguished: tympanogenic (from the middle ear cavity through the labyrinth windows, fistula), meningogenic (from the subarachnoid space of the brain), hematogenous (through the vessels and lymphogenous pathways in patients with general infectious diseases of viral etiology).
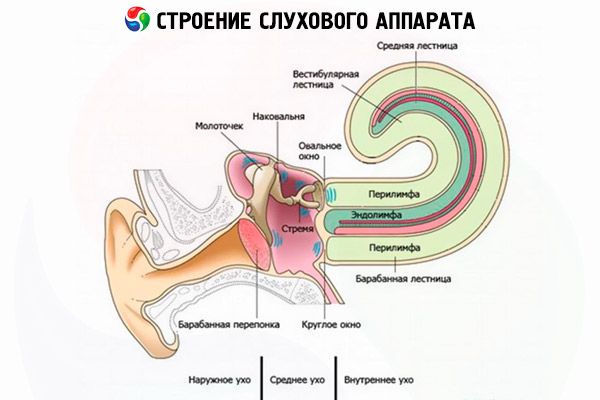
The transition of the inflammatory process from the middle ear is possible in any part of the labyrinth wall, but usually occurs through the membranous formations of the labyrinth windows and the lateral semicircular canal. In acute purulent inflammation of the middle ear and chronic purulent mesotympanitis, the inflammatory process spreads through the windows without violating their integrity or by breaking through, which leads to the development of acute diffuse serous or purulent labyrinthitis. In chronic purulent epitympanitis, the spread of inflammation occurs through the destruction of the bone labyrinth wall by the pathological process, often in combination with a breakthrough of the membranous formations of the windows; the infection can pass along the "reformed paths" (vessels, seals).
In the pathogenesis of labyrinthitis resulting from trauma, the following are important: violation of the integrity of the bone and membranous labyrinth, the degree of edema, hemorrhage into the peri- and endolymphatic space. If, in addition to labyrinthitis, there is a violation of blood circulation in one of the terminal branches of the internal auditory artery (compression, blood stasis), then necrotic labyrinthitis develops. Compression of such small-diameter arteries as the internal auditory artery is facilitated by endolymphatic edema, which is especially often expressed in serous inflammation. Limited labyrinthitis is observed only in chronic purulent epitympanitis with caries and cholesteatoma. In chronic purulent epitympanitis, the destruction of the wall of the bone labyrinth occurs under the influence of the inflammatory process or cholesteatoma, which, by pressure, contributes to the creation of a fistula of the labyrinth.
Most often, the fistula is localized in the area of the lateral semicircular canal, but it can form in the area of the base of the stapes, promontory, and other semicircular canals. During the period of exacerbation of inflammation, exudate appears in the middle ear, due to which limited labyrinthitis turns into diffuse. In syphilis, any path of transition of a specific inflammatory process into the labyrinth is possible, including hematogenous.
From the cranial cavity on the side of the meninges, the infection penetrates into the inner ear through the cochlear aqueduct and the internal auditory canal.
In the pathogenesis of labyrinthitis that developed as a result of trauma, the following are important: disruption of the integrity of the membranous and bony labyrinth, concussion, and hemorrhage into the peri- and endolymphatic spaces.
Morphological changes in the inner ear in serous, purulent and necrotic labyrinthitis are different.
Serous labyrinthitis is characterized by endolymphatic edema, swelling, vacuolization, and disintegration of the neuroepithelium. Purulent labyrinthitis is characterized by an accumulation of polymorphonuclear leukocytes and bacteria in the perilymphatic space against the background of dilated blood vessels. Then these changes occur in the endolymphatic space, the edema progresses, and necrosis of the membranous and later bone walls of the labyrinth occurs. With a favorable outcome, fibrosis and the formation of new fibrous tissue are possible, which leads to the destruction of all repector and nerve elements. Necrotic labyrinthitis is characterized by alternating areas of purulent inflammation and necrosis of soft tissues and the labyrinth capsule. The inflammatory process can affect the entire labyrinth or be limited to one of its parts. The process ends with labyrinthine sclerosis.
In case of specific infection, labyrinthitis has some morphological features. Thus, changes in tuberculous labyrinthitis are manifested in two forms: proliferative and exudative-necrotic. Damage to the inner ear in syphilis is manifested as meningoneurolabyrinthitis, with ostitis of the temporal bone involving the membranous labyrinth. The morphological picture is characterized by edema, increasing dystrophy of the membranous labyrinth, areas of fibrous tissue proliferation, along with bone resorption.
 [ 5 ]
[ 5 ]
Symptoms labyrinthitis
In typical cases, acute labyrinthitis manifests itself as a labyrinthine attack of sudden severe dizziness in combination with nausea and vomiting, disturbance of optical and dynamic balance, noise in the ear and hearing loss. Dizziness is systemic, very pronounced; the patient cannot raise his head or turn it to the side; the slightest movement increases nausea and causes vomiting, profuse sweating, and changes in the color of the skin of the face. With serous labyrinthitis, the symptoms persist for 2-3 weeks, and gradually lose their severity and disappear. With purulent labyrinthitis, after the acute inflammation subsides, the disease can become protracted.
Sometimes labyrinthitis develops as a primary chronic and is characterized by periodic obvious or less pronounced symptoms of labyrinthine disorders, which complicates timely accurate diagnosis. Currently, in such cases, it is helpful to conduct a study of the temporal bone using high-resolution neuroimaging methods.
Cochlear symptoms - noise and hearing loss up to deafness - are observed both in diffuse serous and purulent labyrinthitis. Persistent deafness more often indicates purulent inflammation in the labyrinth.
Meningococcal infection usually affects both labyrinths, which is accompanied by mild peripheral vestibular disorders; balance disorder is more common. Simultaneous bilateral complete loss of vestibular excitability is often accompanied by a sharp decrease in auditory function,
Tuberculous labyrinthitis is characterized by a chronic latent course and progressive dysfunction of the labyrinth.
The clinical picture of syphilitic labyrinthitis is varied. Typical cases are characterized by fluctuating episodes of hearing loss and dizziness. In acquired syphilis, three forms of labyrinthitis are distinguished:
- apoplectiform - sudden and irreversible combined or isolated loss of labyrinth functions in one or both ears. Often there is simultaneous damage to the facial nerve (a process in the pontine-cerebellar angle). Occurs in all stages of syphilis, but more often in the second.
- acute form (in syphilis) - intermittent noise in the ears and dizziness - sharply increase by the end of the 2nd-3rd week, sharp suppression of the labyrinth functions quickly occurs. Observed in the second and third stages of syphilis.
- chronic form - tinnitus, gradual loss of hearing and vestibular excitability that is imperceptible to the patient, which can only be diagnosed with additional examination of the patient. Observed in the second stage of the disease.
Where does it hurt?
Forms
Labyrinthitis is distinguished.
- According to the etiological factor - specific and non-specific.
- According to pathogenesis - tympanogenic, meningogenic, hematogenous and traumatic.
- Tympanogenic labyrinthitis is caused by the penetration of the infectious agent into the inner ear from the middle ear cavity through the labyrinth windows.
- Meningogenic labyrinthitis develops with meningitis due to the penetration of infectious agents from the subarachnoid space through the cochlear aqueduct or internal auditory canal.
- Hematogenous labyrinthitis is caused by the penetration of infectious agents into the inner ear with the bloodstream: it occurs more often in viral infectious diseases.
- Traumatic labyrinthitis is caused by trauma (for example, a fracture of the base of the skull, a gunshot wound).
- By the nature of the inflammatory process - serous, purulent and necrotic.
- Serous labyrinthitis is characterized by an increase in the amount of perilymph, swelling of the endosteum of the labyrinth, the appearance of fibrin and formed elements of the blood in the endo- and perilymph.
- Purulent labyrinthitis is caused by pathogens of purulent infection and is characterized by leukocyte infiltration of the peri- and endolymph, and the formation of granulations.
- Necrotic labyrinthitis is characterized by the presence of areas of necrosis of soft tissues and the bone labyrinth, usually alternating with foci of purulent inflammation.
- According to the clinical course - acute and chronic (manifest and latent).
- Labyrinthitis is an acute serous or purulent labyrinthitis, manifested by suddenly developing symptoms of dysfunction of the inner ear (dizziness with nausea and vomiting, disturbance of static and dynamic balance of the body, noise in the ear, hearing loss); with serous labyrinthitis, the symptoms gradually disappear after 2-2 weeks, with purulent labyrinthitis, the disease can become chronic.
- Chronic labyrinthitis, characterized by the gradual development of dysfunction of the inner ear (dizziness with nausea and vomiting, tinnitus, disturbance of static and dynamic balance of the body, hearing loss), the presence of a fistula symptom, spontaneous vestibulovegetative, vestibulosensory and vestibulosomatic reflexes.
- By prevalence - limited and diffuse (generalized).
- Limited labyrinthitis is a lesion of a limited area of the wall of the bony labyrinth; it is observed in chronic otitis media and is caused by granulating osteitis or pressure of cholesteatoma.
- Diffuse labyrinthitis is a purulent or serous labyrinthitis that has spread to all parts of the bony and membranous labyrinth.
- Viral labyrinthitis most often develops against the background of herpes zoster oticus, beginning with pain in the ear and behind the ear, vesicular rashes in the external auditory canal. The combination of auditory and vestibular disorders is often accompanied by facial nerve paresis. The viral infection spreads to the vestibular nerve, posterior semicircular canal and sacculus.
Diagnostics labyrinthitis
The basis for timely diagnosis of labyrinthitis is a reliable and carefully collected anamnesis.
Tympanogenic labyrinthitis is the most common. To diagnose it, it is necessary to conduct otoscopy, vestibulometry and audiometry, radiography or CT of the temporal bones. If acute or chronic otitis media is detected in a patient, the fistula symptom is examined.
The pathognomonic sign of limited labyrinthitis with fistula, but against the background of preserved function of the neuroepithelium of the inner ear, is the fistula symptom, that is, the appearance of dizziness and nystagmus towards the diseased ear when air is compressed in the external auditory canal.
The essential diagnostic signs of labyrinthitis are spontaneous vestibular reactions occurring according to the peripheral type. The correct assessment of spontaneous nystagmus in combination with a harmoniously occurring vestibulospinal reflex is of decisive diagnostic importance. The direction and intensity of nystagmus change according to the severity of the inflammatory process and the stage of the disease.
In the initial stages of both serous and purulent labyrinthitis, spontaneous nystagmus is directed toward the affected labyrinth and has I, II, III degrees of expression. This nystagmus is combined with a deviation of the arms and body toward the slow component, is observed for several hours, sometimes days, gradually changing its direction to the opposite (toward the healthy labyrinth). The appearance of spontaneous nystagmus in the opposite direction is the result of the development of compensatory mechanisms in the central sections of the vestibular analyzer, aimed at equalizing the functional state of the two labyrinths. This type of nystagmus is rarely observed and detected, since it persists for a short time.
Often, spontaneous nystagmus, which is absent during visual assessment, is recorded using electronystagmography. After 2-3 weeks, spontaneous nystagmus disappears. Experimental vestibular reactions during this period of labyrinthitis are contraindicated and inappropriate, as they can cause increased dizziness and do not help in making a diagnosis. However, subsequent experimental vestibular tests allow us to identify nystagmus asymmetry along the labyrinth, the phase of suppression, and to assess the development of central vestibular compensatory reactions. Initially, a decrease in vestibular excitability on the side of the affected labyrinth is accompanied by hyperreflexia on the side of the healthy labyrinth, and in the recurrent period of the disease, vestibulometry reveals symmetrical hyporeflexia and the absence of spontaneous nystagmus. In addition to spontaneous nystagmus, other labyrinthine symptoms are also revealed - gait disturbance and deviation of the head and body to the healthy side. It is important to know that turning the head to the sides in a patient with labyrinthitis is accompanied by a change in the direction of spontaneous nystagmus, which leads to a change in the direction of the patient's torso deviation. In cerebral pathology, the patient always deviates toward the lesion.
When examining hearing in patients with labyrinthitis, mixed-type hearing loss is noted, most often with a predominance of sensorineural hearing loss.
In congenital syphilis, the course and symptoms depend on the severity of the infection and specific changes in the body. The disease begins in childhood and manifests itself with symptoms of dysfunction of the inner ear. In late congenital syphilis, an atypical fistula symptom is often detected in the presence of an intact eardrum and the absence of a fistula in the lateral semicircular canal. Unlike the typical fistula symptom, nystagmus with compression in the external auditory canal is directed toward the healthy side, and with decompression - toward the irritated ear.
The peculiarity of the course of traumatic labyrinthitis is the nature and severity of the injury itself.
Screening
Not carried out.
 [ 8 ]
[ 8 ]
Indications for consultation with other specialists
Depending on the etiology of the disease, in some cases a consultation with a neurologist, neurosurgeon, or dermatovenerologist is required.
What do need to examine?
Differential diagnosis
In tympanogenic and traumatic labyrinthitis, purulent infection can penetrate into the cranial cavity, causing intracranial complications - meningitis and abscess. Diagnosis of intracranial complications can be difficult. Deterioration of the general condition, fever, headache, increased dizziness, and cerebellar symptoms are typical. To identify complications, CT of the brain and consultation with a neurologist and neuro-ophthalmologist are necessary.
Thus, to recognize labyrinthitis it is necessary:
- establish the fact of inner ear disease (anamnesis);
- to ensure that the disease is infectious in nature;
- clarify the ethnological factor;
- determine the prevalence of the process in the labyrinth.
Diagnosis is not difficult if there are characteristic vetibulo-auditory disorders caused by the infection. Anamnestic data, otoscopy results, hearing and vestibulometry tests, and positive fistula test results are taken into account. Of significant importance at present is not radiography of the temporal bones, as was previously the case, but CT and MRI of the brain and inner ear. High-resolution MRI and CT with visualization of the inner ear structures have become the most important diagnostic methods for examining inner ear pathologies, including labyrinthitis of inflammatory genesis.
Audiometry and vestibulometry help to identify the peripheral nature of auditory and vestibular disorders. It is characteristic that in case of non-purulent inner ear pathology, deafness is rare (infarction of the inner ear). A comprehensive assessment of the results of all patient examination methods contributes to successful diagnostics of labyrinthitis. Differential diagnostics should also be carried out with limited otogenic pachymeningitis (arachnoiditis) of the posterior cranial fossa and cerebellopontine angle, acute thrombosis of the auditory artery. Otogenic arachnoiditis is characterized by otoneurological symptoms revealing a combined lesion of the root of the VIII, V and VII cranial nerves. Acute thrombosis of the internal auditory artery is characterized by acute symptoms of loss of function of auditory and vestibular receptors against the background of vascular pathology (arterial hypertension, atherosclerosis).
Who to contact?
Treatment labyrinthitis
Treatment is carried out in a hospital, taking into account the etiology and pathogenesis of the disease,
Drug treatment of labyrinthitis
Conservative treatment includes the use of antibiotics taking into account the sensitivity to the pathogen and their penetration through the hematolabyrinthine barrier. Patients with labyrinthitis are prescribed drugs that have an anti-inflammatory, hyposensitizing effect, normalizing metabolic processes in the inner ear and brain. During a labyrinthine attack - vestibulolytics. drugs that improve blood supply to the inner ear.
Surgical treatment of labyrinthitis
Surgical treatment of otogenic labyrinthitis involves mandatory removal of the purulent focus from the middle ear cavities and careful revision of the promontory wall. Sanitary ear surgery is performed for any form of labyrinthitis. Surgical interventions on the labyrinth are indicated for purulent labyrinthitis and labyrinth sequestration. Labyrinthotomy is limited to drainage of the purulent focus in the inner ear by opening it and removing the pathological contents. Mastoidectomy for acute uncomplicated labyrinthitis is performed only in cases where the mastoid process is involved in the process. Labyrinthogenoic intracranial complications require labyrinthectomy: the entire labyrinth is removed, the dura mater of the posterior cranial fossa is exposed, and good drainage of the cranial cavity is created.
Prevention
Sanitation of foci of infection in the middle ear cavity.
Forecast
Approximate periods of incapacity for work range from 3 weeks to 3 months. The periods are determined by the slow restoration of vestibular function.

