Medical expert of the article
New publications
Ischemic nerve neuropathy: types
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
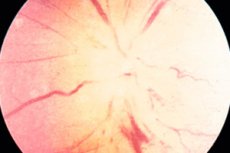
When it comes to ischemic neuropathy, everyone immediately remembers the pathology of the optic nerve, caused by a violation of blood circulation in one of the sections of the eye. More precisely, even the sections of the nerve itself, which adjoins the eyeball. The intra- and retrobulbar sections are most susceptible to ischemic lesions.
Ischemic optic neuropathy
Ischemic optic neuropathy includes 2 types of pathologies that differ in the localization of the lesion of the optic nerve. Anterior ischemic optic neuropathy is a lesion of nerve fibers in the intrabulbar region, which is limited by the sclera and is located within the eyeball. This is the shortest section of the optic nerve (only 0.5 mm), in which its disk is located.
Ischemic disorders in the optic disc (in the anterior form of the pathology, the retinal, choroidal or scleral layer is affected) can be noticed already at an early stage even with the help of conventional ophthalmoscopy.
Posterior ischemic optic neuropathy is changes in the retrobulbar (also known as intraorbital) section. The length of this section is from 2.5 to 3.5 cm, it is located between the sclera and the orbital opening of the optic canal. Unfortunately, the disruption of the blood supply to the nerves in this section at the beginning of the pathology is not noticeable during ophthalmoscopy or retinography. Only electrophysiological methods of examination and Dopplerography of the vessels (carotid, ophthalmic and supratrochlear artery) will be informative.
As in the first case, the disease mainly affects older people. At the same time, the frequency of detection of this pathology in men is significantly higher than in women.
The main specific symptom of both pathologies is considered to be a sharp decrease in the quality of vision due to vascular spasm, thrombus blockage or sclerotic changes. The influence of systemic diseases and acute blood loss is not excluded.
But ischemic processes can occur not only in the optic nerve area, but also in other structures of the nervous system. The cause of neuropathies in any case will be a violation of blood flow in the vessels that feed a specific nerve.
Ischemic neuropathy of the facial nerve
This is a lesion of one of the youngest nerves in the cranial region. This easily injured formation carries an important function of regulating facial expressions. In other words, it is responsible for the innervation of facial muscles. It is clear that a decrease in its function leads to the appearance of a strange grimace on the face, which a person cannot control. And deterioration of the nerve fibers can occur due to a circulatory disorder in one of the vessels passing near a certain branch of the facial nerve.
The facial nerve is a rather complex branched structure, the fibers of which are intertwined with the fibers of other structures responsible for the sensitivity of the tongue, salivation and lacrimation. In the immediate vicinity of the nucleus of the facial nerve in the depths of the brainstem are also located the nuclei of other nerves (auditory, abducens, trigeminal). Damage to these nerve structures is also possible, then the symptoms of damage to the facial nerve (half-closed eyes and mouth, distorted facial features, sagging cheeks, etc.) can be superimposed on such symptoms as changes in taste perception, strabismus, hearing loss, salivation, excessive lacrimation, etc.
According to statistics, the incidence of this type of pathology is about 0.025%. Treatment of the disease is quite long - 21-30 days, and the recovery period can last from 3 weeks in mild cases to six months in advanced cases. The prognosis depends on the degree of nerve damage. Complete muscle paralysis gives a half-prognosis. Complete restoration of muscle mobility is observed in half of the patients. With partial paralysis, this figure increases to 85%. In 1 out of 10 patients, the disease can relapse.
Depending on the degree of damage to the facial nerve, the facial expression disorder is replaced by a strange mask. With complete muscle atony, a strange picture is observed. Usually the process is one-sided, so one half of the face has the same usual expression, and the other turns into a grimace: all wrinkles on the forehead, around the eye, in the nasolabial triangle are missing, the eyelid and corner of the lips drop, the eye slit becomes unusually wide, while the person cannot close the eye completely. Because of the slightly open mouth, there are difficulties with eating, especially liquid food, which pours out.
Well, let's move on, from the head down to the body. In the shoulder area we see a nerve plexus consisting of the thoracic spinal and cervical nerves. Below it (along the arm) several short and long branches diverge, and any of them can be subject to ischemic damage if the blood flow of the vessel feeding the nerve is disrupted.
One of the long branches of the brachial plexus is the median nerve, which passes side by side with the brachial artery through the axillary area and then stretches along the medial edge of the humerus. At the bottom of the shoulder, it dives under the ligament of Struther, then goes into the thickness of the round muscle, called the pronator, and comes out on the forearm. At this point, the nerve has practically no branches. They appear in the area of the forearm and hand.
In the forearm, the nerve passes under the muscles responsible for flexion movements of the fingers. Here, the entire anterior muscle group is under its control.
The median nerve enters the hand area through the wrist canal, which is also called the carpal tunnel. Here, the nerve is responsible for the innervation of the muscles responsible for the movement of the thumb and the sensitivity of the skin on the palm side of the 3.5 fingers, including the thumb, the lumbrical muscles, and the wrist joint.
Due to the special anatomical structure of the median nerve, its most vulnerable places are considered to be tunnels, where the nerve passes between muscles, ligaments, joints, where it can be pinched together with the nearby artery that supplies the nerve with nutrition. Tunnel syndromes include: carpal tunnel syndrome, round pronator syndrome, Struther's band syndrome, etc.
Ischemic neuropathy of the median nerve
It becomes clear that in this case we are not talking about ischemic neuropathy, but about compression-ischemic neuropathy of the median nerves, where ischemia occurs due to compression of the nerve and vessels. The cause of such compression can be injuries, tumors, inflammatory and degenerative processes in muscles and joints. Sometimes tunnel syndrome is associated with professional activities and regular performance of tasks in which nerves and vessels are compressed.
The most indicative symptoms of the pathology are considered to be: severe pain, which can affect areas of the medial surface of the forearm, hand and first 3 fingers, swelling of the affected area, the appearance of heat in this area (with ischemia, a reverse reaction with cyanosis and hypothermia is often observed), sometimes numbness and tingling in the hand and palm are noted. A person cannot clench his fingers into a fist, bend or bend the thumb, the second finger usually does not bend either, and with bending the third, certain difficulties are eliminated.
Ischemic neuropathy of the ulnar nerve
The ulnar nerve is another long branch of the brachial plexus that can be compressed along with the vessels that feed it, resulting in compression-ischemic neuropathy of the ulnar nerve. This nerve also gives branches, only starting from the forearm, but it is responsible for the innervation of the flexor ulnaris, the hand, some part of the deep flexor of the fingers, the muscle responsible for adduction of the thumb, the interosseous and lumbrical muscles, the muscles of the last finger, the skin of the palms and fingers.
Together with the ulnar artery, the nerve passes through the cubital canal (aka the ulnar canal) and Guyon's canal in the wrist area, where their compression is most often observed, which is accompanied by weakness of the hand, due to which a person cannot perform habitual movements (take something in the hand, type on text, play the keyboard, etc.). Numbness is also a characteristic syndrome of the pathology, it is felt in the area of the little finger and part of the ring finger, as well as on the outside of the palm.
A person may feel discomfort and pain in the elbow, which often radiates to the wrist and hand. The middle and outer phalanges of the fingers are constantly bent, which creates the impression of a predator's paw with claws.
The causes of the pathology are identical to the previous type of neuropathy. These are injuries, inflammations, rheumatic changes, as well as performing certain work and bad habits that lead to compression of the nerve in the elbow or wrist area.
Another long branch that comes out of the brachial plexus is called the radial nerve. It runs along the back of the armpit and rests at the intersection of the latissimus dorsi muscle and the tendon of the triceps brachii. This is where the radial nerve can be compressed.
The nerve then passes along the humeral groove, spiraling around the bone itself, where it can also be subject to compression. Compression of this nerve is also possible in the elbow area, where it passes along the inner part of the elbow bend, then descending to the hand in the form of two branches: superficial and deep.
Ischemic radial neuropathy
The radial nerve is responsible for the innervation of the muscles that extend the forearm and hand, abduct the thumb, extend the proximal phalanges of the fingers and turn the palm upward, provides sensitivity to the elbow, the back of the shoulder, the back of the forearm, some part of the hand and the first 3 fingers with the exception of the extreme (distal) phalanges.
Ischemic neuropathy of the radial nerve can be caused by its compression due to trauma, tumors, untimely removal of the tourniquet, frequent regular bending of the arm at the elbow or wrist, compression during sleep. Compression in the armpit area occurs due to the use of crutches or when leaning on a leg bent at the knee while sitting. Compression of the radial nerve in the wrist area is possible when wearing handcuffs.
The cause of ischemic neuropathy may be inflammatory and degenerative changes in the tissues in the area of the radial nerve and the vessels that feed it. Ischemia may also be a consequence of infectious systemic diseases and severe intoxications.
If we are talking about a nerve lesion in the armpit, the symptoms will be difficulty in extending the arm in the area of the forearm, hand and phalanges of the fingers closest to the palm. There is a strong weakening of the hand. Even if the arms are raised, the hand will still remain hanging. The person cannot move the thumb to the side, feels numbness and tingling on the back of the first 3 fingers, although the sensitivity of the distal phalanges remains.
If the nerve is affected in the spiral canal, the elbow reflex and extension of the arm at the elbow are not impaired, as is the sensitivity of the back of the shoulder.
When the nerve near the elbow joint is affected, a person experiences pain and numbness on the back of the hand every time the arm is bent at the elbow. In this case, the sensitivity of the forearm may remain normal or slightly reduced.
Nerve damage in the wrist area is characterized by two syndromes: Turner's (with fractures) and radial tunnel (with compression of the superficial branch). In both cases, the back of the hand and fingers go numb, and a burning sensation and pain are felt on the back of the thumb, which can spread up the entire arm.
In the area of the upper limbs there are several more short nerves (long thoracic, subclavian, axillary, supra- and subscapular nerves, etc.), as well as long branches: musculocutaneous and medial nerve of the forearm. All of them can also be subject to ischemia, but this happens much less frequently than with the nerves described above.
Ischemic neuropathies of the upper extremities are no longer pathologies of old age. They are more typical for young people and middle-aged people, i.e. the working-age population.
And what will the nerves of the lower extremities tell us, for which ischemic neuropathy is also not something unimaginable, especially considering the frequent cases of varicose veins and leg injuries?
The work of the muscles of our legs is controlled by two types of nerve plexuses. One of them is called lumbar, the second - sacral. Several branches come out of the lumbar plexus, passing in the iliac-sternal and inguinal region, in the area of the genitals, thigh. The lumbar plexus also includes the lateral and obturator nerves.
All these branches are engaged in the innervation of the muscles and skin of the pelvis and thigh, and can be subject to ischemia to a greater or lesser degree, but not as often as the nerves of the sacral plexus.
The sacral plexus has 3 sections: coccygeal, genital and sciatic. But of all the nerve fibers of the sacral plexus, the largest of the nerves, called sciatic because it runs in the buttocks, and its branches - the peroneal and tibial nerves, are most often damaged. The sciatic nerve branches into two unequal branches in the second half of the length of the thigh near the popliteal fossa.
The sciatic nerve passes inside the pelvis and through a special opening comes out on its back surface, dives under the piriformis muscle, runs along the thigh along its back part and divides not far from the popliteal fossa. Thanks to this nerve, we can bend the leg at the knee.
Damage to the sciatic nerve is possible along its entire route as a result of trauma, tumor processes, hematomas, aneurysms, and prolonged compression. But most often it is compressed by the piriformis muscle, altered as a result of various pathologies of the spinal column or an incorrectly administered intramuscular injection.
Damage to the sciatic nerve, as well as other nerve structures, is also possible with systemic infectious and inflammatory pathologies and toxic effects on the body.
Symptoms of sciatic nerve damage include piercing pain along the nerve, limiting movement of the limb, numbness and tingling in the back of the leg and foot, and difficulty bending the leg at the knee.
Neuropathy of the sciatic nerve is second in frequency only to pathology of one of its branches – the peroneal nerve. This nerve, passing under the knee, bifurcates at the beginning of the fibula. Thus, the deep and superficial branches become the continuation of the nerve. The first goes along the outer surface of the shin and the upper side of the foot, the second – along the anterolateral part of the shin with a transition to the medial part, where the nerve penetrates under the skin and branches into two parts. These parts are called the intermediate and medial cutaneous nerves.
The deep part of the peroneal nerve is responsible for the innervation of the muscles that extend the foot and toes, and also lift the outer edge of the foot. The superficial branch controls the muscles that provide rotation and plantar flexion of the foot, its sensitivity, innervates the skin between the toes and on the lower part of the shin.
Most often, the fibular nerve is affected in the area of the fibular head and the place where the nerve exits the foot. Compression of the nerve and nearby vessels in these areas is called upper and lower tunnel syndrome. In addition to compression, including wearing tight shoes and prolonged immobilization of the limb, injuries, systemic infections and intoxications, the cause of the disease can be changes in muscle and joint tissue caused by diseases of the spine. Less often, the disease is caused by tumors, connective tissue pathologies, metabolic disorders.
Peroneal Nerve Neuropathy
However, vascular disorders (for example, varicose veins or vascular thrombosis) and compression are considered the most common causes of the development of ischemic or compression-ischemic neuropathy of the peroneal nerve.
With ischemic and compression nature of the pathology, the symptoms of the disease appear gradually, their intensity increases with time. The defeat of the peroneal nerve to the place of branching under the knee is characterized by problems with the extension of the foot and toes. The foot remains curved downwards, which presents certain difficulties when walking. A person has to lift his legs strongly so as not to touch the floor with his toes (cock or horse gait). The patient may also experience pain in the outer part of the shin or foot.
If the deep branch of the peroneal nerve is affected by ischemic damage, the foot drop is not as pronounced, but difficulties in its extension and movement of the toes remain. A decrease in the sensitivity of the dorsum of the foot and the space between the first two toes is noted. If the disease lasts for a long time, it is possible to notice a sinking of the interosseous spaces on the dorsum of the foot.
In neuropathy of the superficial branch of the peroneal nerve, there is a decrease in sensitivity of the lateral surfaces of the lower leg and the medial region of the dorsum of the foot. The patient may experience pain in these same places. Flexion of the fingers is not impaired, but the rotation of the foot is somewhat weakened.
Ischemic neuropathy of the tibial nerve
The tibial nerve runs through the center of the popliteal fossa, between the medial and lateral heads of the fleshy gastrocnemius muscle, then between the flexors of the fingers and dives into the lumen of the ankle fork. From there, the nerve enters the tarsal canal, where it is securely fixed together with one of the tibial arteries by the flexor retainer. It is in this canal that compression of the nerve most often occurs.
The tibial nerve controls the movement and sensitivity of the skin and muscles responsible for flexion of the foot and lower leg, inward bending of the foot, various movements of the toes, and extension of the distal phalanges.
In addition to compression in the tarsal region, ischemic neuropathy of the tibial nerve can be caused by injuries (often such injuries are suffered by athletes), foot deformities, prolonged stay in an uncomfortable position, diseases of the knee joint and ankle, tumor processes, metabolic disorders, vascular pathologies (for example, vasculitis, in which inflammation and destruction of the vascular walls occurs).
If the tibial nerve is affected in the area below the knee, the clinical picture of the pathology implies a violation of the downward flexion of the foot (with peroneal pathology, the situation is the opposite, although in both cases there is an inability to stand on tiptoe). During movement, a person puts emphasis on the heel, trying not to lean on the toes. The posterior group of muscles of the lower leg and foot gradually atrophies and the foot begins to resemble a clawed paw of an animal (an identical situation is observed with neuropathy of the ulnar nerve).
Sensitivity impairment is observed on the back of the shin and on the lower third of its front part, in the area of the sole. Sensitivity is reduced over the entire surface of the first 3 fingers and on the back of the 5th finger. The fourth finger is partially affected, since it is innervated by different nerves.
If the neuropathy is traumatic in nature, then, on the contrary, sensitivity may become excessively high and the skin swollen.
Compression of the nerve and the vessels that feed it in the tarsal canal will manifest itself as burning and piercing pain in the sole area, which radiates to the calf muscle. The pain intensifies during running and walking, and also if the patient stands for a long time. Pathologically increased sensitivity is observed on both edges of the foot. Over time, the foot becomes flatter, and the toes bend slightly inward. If you tap with a hammer in the area of the Achilles tendon, the patient will complain of pain in this place.
Damage to the medial nerve on the sole manifests itself as pain on the inner edge of the foot and in the dorsal area of the first 3 toes. If you tap (percussion) in the area of the navicular bone, then sharp piercing pains will be felt in the big toe.
Compression of the nerve in the tarsal canal and damage to the medial branch of the tibial nerve are typical for people with high physical activity, athletes, tourists. Most often, they are provoked by prolonged walking or running.
The defeat of the branches of the tibial nerve in the area of the fingers is typical for people with excess weight who love heels. Thus, this pathology is more typical for women. It is characterized by a pain syndrome that begins at the arch of the foot. The pain is felt at the base of the foot, and also penetrates through the first 2-4 fingers, intensifying during standing or walking.
Damage to the branches of the tibial nerve in the heel area, caused by prolonged walking without shoes or on thin soles, as well as landing on the heel during a jump from a height, is manifested by pain and a strong decrease in sensitivity in this area. But sometimes patients complain of unpleasant sensations in the heel (tingling, tickling, etc.) or increased sensitivity to touch (touching the tissues is painful). Due to fear of such symptoms, a person tries to walk without stepping on the heel.
It should be said that our body is wrapped in a huge network of intersecting nerves and vessels. Disruption of blood flow in any part of the body can easily lead to nerve damage, i.e. to the development of ischemic neuropathy. And although the causes of such disorders can be completely different, the consequences of nerve damage always affect the patient's quality of life, limit movement, ability to work, and sometimes communication, affecting the psycho-emotional state of a person.

