Medical expert of the article
New publications
HPV type 52: what is it, how to treat?
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The abbreviation HPV is probably known to everyone nowadays. It stands for human papillomavirus. Many different strains of this virus have already been discovered, about two hundred. HPV type 52 is one of 19 papillomaviruses recognized as oncogenic. This means that its carrier has a risk of developing certain types of cancer, in particular, cervical and rectal cancer. In addition, in rarer cases, it can provoke the development of carcinoma of the vaginal walls, penile skin, oral cavity, conjunctiva and pharynx. Localizations are listed in descending order of frequency of occurrence. [ 1 ], [ 2 ]
HPV type 52 belongs to the α-papillomavirus-9 species, as does their most oncogenic representative, HPV type 16, which is found in tumor cells in more than half of patients with cervical carcinoma and is considered the culprit of their malignant transformation.
Structure HPV type 52
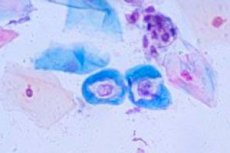
In the resting stage, the papillomavirus cell (virion) is a microscopic sphere 30 nm in diameter, consisting of a DNA molecule compactly packed with cellular proteins (histones). The virion does not even have a cellular membrane. For example, the flu virus is much more solid - four times larger, enclosed in a membrane formed from a similar structural component of the affected cell.
Genotype 52 HPV is similar to the genotype of the most highly oncogenic virus 16. Previously (before 2010) they were even considered the same virus, but then some differences were “discovered” and they were classified as one species.
HPV 52 DNA is a circular double-stranded molecule packed in the nucleus of the virus cell by two types of proteins E (early) and L (late). E proteins are responsible for the regulatory role, ensure the replication of the virus and are blamed for the initiation of the process of malignancy of keratinocytes in which they have settled. L proteins are a purely structural component, they form the outer protein shell of the virion (capsid).
Life cycle HPV type 52
Any virus is a cellular parasite. The papillomavirus parasitizes keratinocytes – cells of the upper layers of the skin and mucous membranes of living organisms. Outside these cells, the virion remains viable for a short time, up to three hours, and then on damp towels, linen.
HPV type 52 is transmitted mainly through genital-anal-oral contacts of any kind, penetration occurs through microdamage to the skin or mucous membranes. Household transmission is not excluded, but is unlikely.
The virus infects keratinocytes near the site of introduction. It does not spread throughout the body, but self-infection is possible. This can happen during depilation or shaving, if the skin surface is damaged during the procedure and the wound is touched with an infected surface.
The life cycle of HPV 52 corresponds to the stages of keratinocyte maturation and cytodifferentiation. Viruses, getting on damaged epithelium, affect young, not yet differentiated cells of the basement membrane, which is located under the upper layers of more mature cells. As keratinocytes mature, they rise to the surface of the skin, while the viruses "settle" in the cells. E-proteins perform their functions to ensure the necessary content of HPV DNA in the affected skin cells, activate the expression of viral genes, and bind tumor suppressors. The immunity of an infected person is also not asleep and in the overwhelming majority of cases of infection (80-90%) the body destroys the viruses on its own within a year. However, in about a fifth of those infected, the virus is integrated into the cell genome and a long chronic course of the disease begins with periodic relapses and the possible development of a neoplastic process. New viruses ready for infection appear at the last stage of keratinocyte differentiation and are detected depending on the localization in physiological substances: saliva, sperm, vaginal secretions, superficial layers of the skin and mucous membranes.
Symptoms
These tiny cellular parasites may not show their presence in the human body for a very long time, measured in decades. Moreover, in the infected cell, the virus can be in different forms: extrachromosomal (episomal) and integrated into the cell DNA (intrasomal). The first option is considered more favorable.
HPV type 52 belongs to a group of viruses that prefer the skin and mucous membranes of the genital organs. The first clinical signs of its presence are pointed condylomas (small sharp growths on the epithelium). They usually appear on the mucous membranes or skin of the genitals, less often in the anus, and very rarely in the oral cavity. At first, these are single small formations, later without treatment they merge. In appearance, such growths resemble cauliflower inflorescences.
HPV 52 is most often detected in women under the age of 35. Moreover, in 80% of cases it is detected in the absence of any symptoms.
Condylomas, if present, are detected during examination on the labia, clitoris, vaginal walls and cervix. Cervical erosion is also a reason for HPV testing.
Sometimes a woman herself can detect condylomas visually or by touch in accessible places when performing hygiene procedures.
The most common and dangerous consequence of infection with this type of papillomavirus is cervical cancer. [ 3 ]
HPV 52 during pregnancy has the same symptoms as in non-pregnant women. It is most often detected during examination. Asymptomatic presence of the virus in the body is subject to observation, but not treatment. A pregnant woman may also have pointed condylomas; if they are small, no treatment is carried out during pregnancy. Large condylomas in the birth canal are usually an indication for delivery by Caesarean section. [ 4 ]
HPV 52 in men can manifest itself as the growth of pointed condylomas on the penis. The most serious consequences of the virus parasitism are malignant neoplasms of the skin of the penis and, possibly, the prostate gland. Infection of males occurs with the same frequency as females. However, due to the anatomical features of the structure, the male urethra does not have an area of abnormal epithelial change, therefore, in the vast majority of men, the infection does not manifest itself in any way, and self-elimination of the virus often occurs. [ 5 ]
In both sexes, condylomas can be located in the area of the anus, urethra, rectum, and oral cavity. Condylomas on the mucous membrane of the urethra can manifest themselves by urination disorders, in the rectum - difficulty emptying the bowels, the appearance of traces of blood during defecation. [ 6 ]
The presence of HPV type 52 probably increases the risk of developing rectal cancer [ 7 ] and laryngeal cancer. [ 8 ], [ 9 ]
Diagnostics
The presence of any type of human papillomavirus in the body in the absence of symptoms can be detected by analyzing a urogenital scraping (if necessary, a scraping is taken from other places), carried out by the polymerase chain reaction method or the Digene test (rapid highly specific screening). [ 10 ]
Qualitative analysis gives an answer about whether any DNA fragment of any human papillomavirus is detected in the biomaterial or not. Accordingly, the result will be positive or negative.
Analysis for HPV 52 or any other specific strain is called genotyping and is performed if the first stage result is positive. Often, one patient is found to be infected with several viral genotypes.
To clarify the carcinogenic load on the body, a quantitative analysis is carried out.
The norm for HPV 52 is either a negative qualitative analysis or a level of viral invasion below the detectable level, although it is possible that some DNA fragments were detected.
If the HPV 52 result is positive, then it is also quantitatively ambiguous:
- if the number of copies of DNA fragments does not exceed 10³ per 10⁵ keratinocytes, a low probability of developing neoplastic changes is diagnosed;
- if the number of copies of DNA fragments exceeds 10³ per 10⁵ keratinocytes, a chronic infectious process with a high probability of developing neoplastic changes is diagnosed;
- If the number of copies of DNA fragments exceeds 10⁵ per 10⁵ keratinocytes, a high carcinogenic load and an increased probability of cervical cancer are diagnosed.
A dynamic PCR analysis for HPV may be prescribed, usually it is done no earlier than six months later. If the next time a decrease in the carcinogenic load is observed, this is a favorable prognostic criterion. Growth indicates the possibility of further development of the process. Genotyping of the human papillomavirus using a linear array is also used. [ 11 ]
However, the definitive test for suspected neoplasia is the test for abnormal cells. For cervical cancer, this is a smear for oncocytology (Pap test). If such cells are found, then a biopsy is performed to determine the extent of the intervention. [ 12 ], [ 13 ], [ 14 ]
Treatment
There are no conservative methods of destroying the human papilloma virus. If the immune system fails to cope with the invasion, and parasitism leads to uncontrolled cell proliferation, modern medicine can only offer radical elimination of growths, warts, areas of altered tissue, treatment of combined infections and immunostimulation.
Such measures usually give a temporary effect, and any change in the immune status can provoke a relapse. The indication for surgical intervention is the result of oncocytological tests (the presence of abnormal cells), and not the fact of a positive PCR test result.
What to do if HPV 52 is detected? Nothing. Take this into account, see a gynecologist, repeat the test in about six months to see the quantitative indicator in dynamics. You are a potential source of infection, you should take this into account and protect your partners as much as possible. This is what you need to do if there are no other symptoms and no mixed infection is detected.
If condylomas, warts, erosions, combined bacterial infections transmitted sexually are detected, they must be treated.
After that, follow the recommendations of your gynecologist and do not neglect dispensary registration.
Prevention HPV type 52
Monogamous relationships and, to some extent, barrier contraception will help to avoid infection. In combination with a healthy lifestyle that provides good immunity, such measures are the best prevention of unpleasant consequences of infection with HPV of any type.
Vaccination before the onset of sexual activity is expected to provide protection against HPV infection. The vaccine is designed to protect against the most cancer-causing strains, 16 and 18. Given that HPV 52 is a member of the same species as HPV 16, it may also help protect against HPV. The CDC now recommends that children aged 11 to 12 years receive two doses of the HPV vaccine, up from three previously, to protect against HPV-related cancers. The second dose should be given six to 12 months after the first. The WHO recommends vaccinating adolescents of either sex. [ 17 ]
Infected people who have altered cells at the site of virus entry or skin growths are advised to have them removed and undergo annual examinations by a gynecologist and/or urologist to prevent relapses.
Forecast
In almost 90% of cases, the body copes with the human papilloma virus itself. If this does not happen, then the prognosis largely depends on the age of the infected person, his immune status, and the type of virus. HPV type 52 is classified as a carcinogenic virus, however, in the vast majority of cases, people with malignant cell degeneration are found to have other types of pathogens - 16 and 18. [ 23 ]
Remember that HPV infection does not mean disease. Infection leads to the development of dysplastic processes (precancer) in 0.5% of women, and timely diagnostics, which is provided by medical examination, allows you to take radical measures in the initial stages of the disease and prevent its development. So a lot depends on your attitude to yourself.


 [
[