Medical expert of the article
New publications
Herpetic encephalitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The probability of infection with Herpes simplex viruses is very high. It is believed that the vast majority of the adult population of the planet are seropositive for labial herpes. The insidiousness of this intracellular parasite is that it can remain latent for a long time, and under favorable conditions for its development, it can affect the central nervous system.
Encephalitis is an inflammation of the brain parenchyma with neurologic dysfunction that may be caused by infectious, postinfectious, and noninfectious causes.[ 1 ] Infection accounts for approximately 50% of identifiable cases and is the most common etiologic category of encephalitis.[ 2 ]
Herpetic encephalitis is a rather rare and severe disease, most cases of which are caused by the virus of the first type. In the absence of timely diagnosis and a course of antiviral therapy, the disease is accompanied by high mortality and a large number of severe neurological complications associated with local involvement of the limbic system of the brain.
The word herpes translates as "creeping" or "creeping", and is a reference to herpetic skin lesions. Goodpasture [ 3 ] and others demonstrated that material from herpetic labial and genital lesions caused encephalitis when inoculated into the scarred cornea or skin of rabbits. In the 1920s, the Mathewson Commission was among the first to report that HSV caused encephalitis in humans. The first pediatric report of HSVE was published in 1941. [ 4 ] The first adult case, a 25-year-old man with headache, fever, aphasia, and left pupillary dilation, was reported in 1944. [ 5 ] Postmortem pathology revealed numerous petechiae and ecchymoses with perivascular lymphocytic cuffing in the left temporal lobe, midbrain, and lumbar spine. Intranuclear inclusions were identified and the virus was isolated from the patient's brain. Since these early reports, significant progress has been made in the pathobiology, diagnosis, and treatment of HSVE.
Epidemiology
Herpetic encephalitis affects two to four people out of a million worldwide every year. Among all encephalitis of various origins, herpetic cases account for about 15%, this figure fluctuates from year to year in a slightly higher or lower direction.
In 60-90% of cases, the herpes virus HSV-1 is detected in patients. [ 6 ] Most experts do not note a connection between the incidence of the disease and the season of the year, but some have indicated that herpes encephalitis occurs more often in the spring.
A person of any gender and age can become ill, however, approximately a third of cases occur in childhood and adolescence (up to 20 years old), and half occur in patients who have passed the half-century age limit.
Although encephalitis is rare in infected individuals, HSV-1 is consistently the single most common cause of sporadic encephalitis worldwide.[ 7 ],[ 8 ] The incidence of HSV worldwide is estimated to be 2 to 4 cases/1,000,000,[ 9 ] and incidence in the United States is similar. There is a bimodal distribution with peak incidence in children (<3 years) and again in adults >50 years of age, but most cases occur in individuals over 50 years of age, regardless of gender.[ 10 ],[ 11 ]
Causes herpetic encephalitis
Most experts are inclined to believe that the development of this disease occurs as a result of the activation of herpes viruses, which exist latently, having integrated into the DNA chains of nervous tissue cells.
Primary infection with HSV-1 or 2 may occur in the form of an inflammatory process in the cortex, subcortex, and white matter of the brain and be the only manifestation of infection. Such cases are typical for the first encounter with the herpes virus in childhood and adolescence.
Diffuse infection with the herpes simplex virus, when the visceral organs and skin are involved in the process, can often spread to the central nervous system with the development of encephalitis.
The vast majority of patients with herpetic inflammation of the brain substance are found to have the herpes simplex virus type 1 (HSV-1), the one that manifests itself as itchy blisters on the lips, much less often - the second (HSV-2), the so-called genital. In cases of chronic sluggish encephalitis, HSV-3 (herpes zoster, causing chickenpox/shingles), HSV-4 (Epstein-Barr virus, causing Filatov's disease or infectious mononucleosis), cytomegalovirus HSV-5, human herpesviruses HSV-6 and HSV-7, which are "noticed" in the development of chronic fatigue syndrome, are found. Sometimes in one patient, cells of different tissues are affected by viruses of different strains (mixed form). So, theoretically, damage by all these types can lead to herpetic encephalitis.
A complication in the form of inflammation of the brain is sometimes caused by the so-called herpetic angina. Strictly speaking, this disease has nothing to do with the herpes virus. Therefore, the encephalitis that occurs against its background is viral, but not herpetic. The causative agent is the Coxsackie virus - an enterovirus. What makes it related to herpes is their viral nature - the ability to parasitize inside cells, including the brain. The same applies to such a disease as herpetic stomatitis. In fact, the so-called herpetic angina (stomatitis) is the same disease, it is just that with angina, the mucous membrane of the pharynx is affected to a greater extent, vesicles appear on it, resembling herpes. With stomatitis, the mucous membrane of the oral cavity is affected to a greater extent. Modern medicine calls this pathology enterovirus vesicular pharyngitis or stomatitis, depending on the predominant area of the rash and the discomfort associated with it. These diseases generally end quite well, with complete recovery, however, in rare cases complications may develop in the form of viral encephalitis, the symptoms of which are identical to herpes.
Herpes viruses that affect human skin cells or mucous membranes of the orolabial zone are embedded in them, begin to multiply and migrate throughout the body by hematogenous and lymphogenous routes, reaching nerve cells. After suppression of the active stage that develops after infection, the viruses are embedded in their genetic apparatus and remain in the nerve cells in a "dormant" state, do not multiply and do not manifest themselves in most carriers. In studies with postmortem oligonucleotide probing, herpes simplex virus DNA was found in neurons of the brain tissue of most deceased people, the cause of death of whom was absolutely not associated with infection with this microorganism. It has been established that the introduction of the herpes virus into cells, in particular, nerve tissue, is not always accompanied by its reproduction and death of the host cell. Usually, it inhibits the replication of the stranger, and the microorganism goes into a state of incubation.
But under the influence of certain trigger factors, the herpes virus is activated, and the latent course of the infection turns into an acute or subacute process, while the brain tissue will not necessarily be affected.
Risk factors
Risk factors that trigger the reactivation process have not been precisely established. It is assumed that these may be local injuries to the face, stress, hypothermia or overheating, immunosuppression, hormonal fluctuations, frequent vaccinations and careless behavior after them. Age is important, infants and the elderly are most at risk of developing herpes encephalitis.
Pathogenesis
The pathogenesis of herpes encephalitis is not uniform. It is assumed that in those infected for the first time, the herpes simplex virus type 1 (childhood and adolescence) enters the cells of the brain substance from the epithelium of the mucous membrane of the nasopharynx. Having overcome the tissue barrier, the microorganism migrates neurogenically (along the neurites of the olfactory neurons) to the olfactory bulb and, under favorable conditions for its development, causes inflammation of the brain substance.
The mechanisms by which HSV gains access to the central nervous system (CNS) in humans are unclear and remain a subject of debate. The most likely routes include retrograde transport via the olfactory or trigeminal nerves [ 12 ], [ 13 ] or via hematogenous dissemination. Viral tropism of the orbitofrontal and mesotemporal lobes argues against hematogenous dissemination in most cases. Experimental data in animals support transmission to the CNS via one or both of the trigeminal and olfactory pathways and suggest that virions may disseminate to the contralateral temporal lobe via the anterior commissure. [ 14 ]
Unlike other cranial nerves with sensory functions, the olfactory nerve pathways do not pass through the thalamus but connect directly to the frontal and mesotemporal lobes (including the limbic system). There is some evidence to support extension of olfactory function to the CNS in humans, but definitive data are lacking.[ 15 ],[ 16 ] The trigeminal nerve innervates the meninges and may extend into the orbitofrontal and mesiotemporal lobes.[ 17 ] However, since the trigeminal sensory nuclei are located in the brainstem, one might expect the relatively rare HSVE-associated brainstem encephalitis to be more common if this was the primary route of entry into the CNS in most cases.[ 18 ],[ 19 ]
Whether HSVE is a reactivation of latent virus or caused by a primary infection is also a matter of debate; both can occur. Proposed pathogenic mechanisms include reactivation of latent HSV in the trigeminal ganglia with subsequent spread of infection to the temporal and frontal lobes, primary CNS infection, or possibly reactivation of latent virus in the brain parenchyma itself.[ 20 ],[ 21 ] In at least half of HSVE cases, the viral strain responsible for encephalitis is different from the strain causing herpetic skin lesions in the same patient, an observation that suggests the possibility of a primary CNS infection.[ 22 ]
HSV infection triggers a strong response from the innate immune system until the adaptive immune system can help eliminate the active infection. Early in the immune response to HSV, pattern recognition receptors called Toll-like receptors (TLRs) located on cells of the innate immune system recognize and bind to pathogen-associated molecular patterns. [ 23 ] This triggers TLR dimerization, which subsequently activates signaling pathways that initiate the production of pro-inflammatory cytokines such as interferons (IFNs), tumor necrosis factor, and various interleukins. [ 24 ] IFNs contribute to host resistance to viral proliferation through activation of the Jak-Stat signaling pathway [ 25 ] and by triggering the production of both RNase enzymes that degrade cellular RNA (both host and viral) and double-stranded RNA-dependent protein kinase, which halts cellular translation. [ 26 ] Deficiencies in the immune response to HSV (e.g., defects in the TLR-3 pathway, including TLR3 itself, UNC93B1, TIR-domain-containing adaptor-inducing IFN-β, tumor necrosis factor receptor-related factor-3, TANK-binding kinase 1, or IFN regulatory factor-3) leave the host susceptible to HSVE. [ 27 ], [ 28 ]
The inflammatory cascade triggers adaptive immunity, which can lead to necrosis and apoptosis of infected cells. Although the host immune response is critical for eventual viral control, the inflammatory response, especially the recruitment of activated leukocytes, can contribute to tissue destruction and subsequent neurological sequelae.[ 29 ],[ 30 ]
Following primary infection, the virus establishes a latent state for the life of the host and remains dormant unless reactivated.[ 31 ] To establish and maintain latency, a number of complex processes must be balanced. These include silencing of lytic-phase viral genes, abrogation of host cell defense mechanisms (e.g., apoptosis), and evasion of host immunity, including both innate and adaptive immune responses (e.g., downregulation of major histocompatibility complex expression).[ 32 ],[ 33 ] HSV-specific CD8+ T cells reside in the trigeminal ganglia and contribute to the maintenance of viral latency.[ 34 ] During reactivation, viral gene expression occurs in a transiently organized manner, as reviewed recently. [ 35 ] After reactivation, the virus can infect adjacent neurons and travel to tissues innervated by infected dorsal root ganglia, causing relapse of the disease and releasing infectious viral particles that can be transmitted to others.
In early infancy, the HSV-2 virus is most often detected. The majority of infections occur during the child's passage through the mother's birth canal if she is currently in the acute stage of the disease (there are rashes on the genitals). The likelihood of infection at the time of birth is highest, so women with acute genital herpes are usually advised to give birth by Caesarean section.
Much less frequently, herpes encephalitis in newborns can be the result of intrauterine infection, and it can also be caused by contact with a sick parent or a representative of the maternity hospital staff after birth, but such cases are much less common.
Adult patients with this neuroinfection usually had herpes rashes in the past or were seropositive for herpes simplex viruses according to test results. Encephalitis could develop with repeated infection with another strain of the virus - in this case, a strain of the herpes virus is found on the mucous membrane of the oral cavity or pharynx (nose), different from the one that affected the brain tissue. Different strains are found in about a quarter of patients with herpes encephalitis.
Three quarters of the remaining patients have orolabial strains of the virus identical to those found in the brain tissue. In this case, two scenarios are assumed. The first option considers the hypothesis that the virus is latent in the nodes of the trigeminal nerve or sympathetic chains, and when reactivated neurogenically (along the nerves innervating the middle cranial fossa) it reaches the brain tissue. The second option assumes that the virus, upon infection, has already reached the neurons of the brain and was there in a state of latency, where, under favorable conditions, it was reactivated.
The herpes virus replication occurs intracellularly, with the formation of intranuclear inclusions, affecting neurons, auxiliary cells (glia) and destroying interneuronal connections.
How is herpes encephalitis transmitted?
Close contact with a patient does not pose a danger in terms of direct infection with herpes encephalitis. Only the virus itself is transmitted. Most often, this occurs during direct contact with an infected person in the acute stage, when he has orolabial, genital, skin rashes. It is not for nothing that herpes is also called the "kissing disease". Liquid secretion from the accumulation of vesicles on the lips of the patient is simply oversaturated with viruses, his saliva and nasal discharge are also seeded with pathogens. The infection affects damaged skin (with microcracks, scratches) when droplets of saliva seeded with microorganisms or rhinobronchial secretion get into the skin when the patient coughs and sneezes, during an emotional conversation, or during direct contact, for example, when kissing. In small children, the virus can penetrate even through intact skin. It is possible to become infected by alternately using the same towel, dishes, lipstick, and other similar actions.
You can get the first and second type of cellular parasite during oral-genital sex with an infected partner. And if the vesicles on the lips are clearly visible, then it is often problematic to determine the active phase of HSV-2 (sexual), since most infected people may have exacerbations in a latent form, and the patient himself simply may not suspect it.
It is also possible to become infected in the latent stage. This usually occurs with frequent direct contact of mucous membranes or with injuries and microdamages on the contact surfaces of the body of a healthy person.
Genital herpes is transmitted from a mother infected during pregnancy to her child vertically (in utero) and by contact during childbirth.
Symptoms herpetic encephalitis
The first signs of the disease are non-specific and resemble the manifestation of many acute infectious diseases. In the early stage, high temperature (39℃ and above), increasing headache in the forehead and temples, weakness, drowsiness, and loss of appetite are noted. Nausea and vomiting, in about half of those affected, join the symptoms of general intoxication in the first hours of the disease. Quite quickly in the early stage, on the second or third day, neurological symptoms begin to appear, indicating the possibility of herpes encephalitis.
The patient begins to behave inappropriately, and behavioral disorders progress. Confusion of consciousness appears, the patient loses spatial-temporal orientation, sometimes ceases to recognize close people, forgets words, events. Hallucinations are observed - auditory, visual, olfactory, tactile, focal and even generalized epileptiform seizures, indicating damage to the limbic part of the brain. Behavioral disorders can be pronounced, some patients experience a state of delirium - they are hyperexcitable, aggressive, uncontrollable. In some cases (with damage to the medial basal areas of the temporal lobes by the virus), opercular seizures are observed - the patient makes automatic chewing, sucking, swallowing movements.
Herpes encephalitis in young children is often accompanied by myoclonic seizures.
Contact with a patient already at an early stage presents certain difficulties associated with a slowdown in mental reactions, memory lapses, confusion and dullness of consciousness.
The early stage of herpetic encephalitis usually lasts for several days, sometimes up to a week, but can progress rapidly and in a few hours progress to the stage of the peak of the disease, which is characterized by disturbances of consciousness up to the development of sopor and coma. In a state of sopor, the patient's consciousness is absent, he does not respond to being addressed, but motor reactions to pain, light, and auditory stimuli are preserved. [ 36 ], [ 37 ]
In a series of 106 cases of HSVE, the main reasons for hospital presentation were seizures (32%), abnormal behavior (23%), loss of consciousness (13%), and confusion or disorientation (13%).[ 38 ]
Symptoms indicating the development of a coma in a patient include disturbances in the respiratory rhythm, with periodic pauses (apnea), motor disturbances on both sides, symptoms of decortication (disconnection of the functions of the cerebral cortex) and decerebration (disconnection of the anterior part of the brain). These postural reactions are extremely unfavorable signs.
The pose indicating the onset of decorticate rigidity is the upper limbs are bent and the lower limbs are extended. The pose of decerebration is the patient's body is drawn up into a string, all limbs are extended, the extensor muscles are tense, the limbs are straightened. The level of damage to the brainstem is determined by the degree of impaired consciousness and dysfunction of the facial and bulbar nerves.
In the absence of adequate treatment, cerebral edema develops, shifting the location of its trunk in relation to other structures. Typically, the temporal areas of the brain are wedged into the tentorial opening, which is accompanied by a triad of symptoms: loss of consciousness, different sizes of pupils of the eyes (anisocoria); weakening of one half of the body. Other focal lesions of the brain and cranial nerves are also observed.
The stage of regression of herpetic encephalitis occurs by the end of the month from the onset of the disease and its duration can be calculated in months. About a fifth of patients recover completely, the rest have lifelong neurological deficit of varying severity. These may be local psychomotor disorders, or there may be a vegetative state.
Herpetic encephalitis in newborns is most severely tolerated by premature and weakened children. They often have the disease in a fulminant necrotic form or rapidly develop respiratory failure, leading to coma. There are usually no rashes, but there are almost always convulsions, paresis, as a result of which the swallowing reflex is impaired, and the child cannot eat.
Full-term infants usually have a milder course. The condition worsens gradually - hyperthermia, the child is weak and capricious, there is no appetite. Later, neurological symptoms may join - convulsions, myoclonus, paresis.
Chronic progressive herpetic encephalitis in newborns manifests itself with symptoms in the first or second week of life. The baby's temperature rises, he becomes lethargic and whiny, characteristic vesicles appear on the head and body, and epileptiform symptoms join in later. Without treatment, the baby can fall into a coma and die.
Herpetic encephalitis in adults and older children also occurs with varying degrees of severity. The classic acute course of the disease caused by the virus of the first and second types is described above. Subacute is distinguished by relatively less pronounced symptoms of intoxication and neurological deficit. It does not reach a comatose state, but hyperthermia, headache, photophobia, nausea, febrile seizures, drowsiness, cognitive disorders, forgetfulness, confusion are always present.
In addition, there are also "milder" variants of the disease. Chronic sluggish herpetic encephalitis is a progressive viral lesion of the brain, which most often affects people over 50 years of age. The symptoms differ from the acute course by a gradual increase. A person notices constant increased fatigue, progressive weakness. His temperature may periodically, for example, in the evening, rise to subfebrile values, or there may be a constant subfebrile temperature. Against the background of increased nervous and physical stress, stress, after colds and flu, as a rule, an exacerbation of the sluggish process is observed. Asthenia of the body increases and eventually leads to a decrease in intellectual potential, loss of working capacity and dementia.
One of the forms of sluggish herpetic encephalitis is chronic fatigue syndrome, the trigger for the development of which is usually a previous illness with flu-like symptoms. After this, the patient cannot recover for a long period of time (more than six months). He feels constant weakness, he is tired of ordinary daily loads, which he did not notice before the illness. All the time he wants to lie down, his performance is at zero, attention is scattered, memory fails, and so on. The cause of this condition is currently considered to be a neuroviral infection, and the most likely etiological factors are called herpes viruses and not only simple herpes, but also HSV-3 - HSV-7.
Types of herpetic encephalitis are classified according to different criteria. According to the severity of symptoms (form of the course), the disease is divided into acute, subacute and chronic recurrent.
Depending on the degree of damage to the brain tissue, a focal and diffuse inflammatory process is distinguished.
The localization of lesions is reflected in the following classification:
- inflammation of mainly the gray matter of the brain - polioencephalitis;
- predominantly white - leukoencephalitis;
A generalized process that affects all tissues is panencephalitis.
Complications and consequences
Herpetic encephalitis is a potentially curable disease, but timely treatment is of great importance. In its absence or late onset, the disease often causes the death of the patient or severe neuropsychiatric complications. The most severe consequence of herpetic encephalitis is akinetic mutism or progressive vegetative state. The patient completely loses the ability to intellectual activity, does not speak or move, only the sleep-wake cycle is fully restored. In addition, the function of breathing and blood circulation is preserved. All other life processes proceed abnormally: the patient is unable to eat, drink, monitor personal hygiene, does not control bowel and bladder emptying. This condition is irreversible and is a consequence of large-scale damage to brain tissue. It develops in patients after coming out of a long coma.
Many patients who have survived a severe course of herpes encephalitis suffer from lifelong persistent neuropsychiatric disorders of varying severity: hemiparesis, hemiplegia, visual and hearing impairment (often on one side), epileptiform seizures. [ 39 ]
Diagnostics herpetic encephalitis
The idea of such a diagnosis is suggested primarily by the presence of neurological disorders - inappropriate behavior, seizures, confusion, which occur with symptoms such as high temperature and severe headache.
If herpes encephalitis is suspected, tests (microscopic examination of cerebrospinal fluid and its polymerase chain reaction to detect fragments of the herpes virus genotype) are urgently prescribed, as well as instrumental studies, the most informative of which is nuclear magnetic resonance imaging. If this is not possible, computed tomography and electroencephalography are performed, [ 40 ] which can be useful for assessing the effectiveness of anticonvulsants. However, the insidiousness of the disease is that in the early stages of development, diagnostic criteria may not go beyond the norm. Then the studies are repeated during the first week.
Polymerase chain reaction of cerebrospinal fluid gives results with high accuracy and allows to replace such traumatic examination as biopsy of brain substance. The detected fragments of DNA of the herpes virus indicate the herpetic etiology of encephalitis, and the positive result of the study is maintained for a week after the start of antiviral therapy.
Microscopy of the spinal cord substance reveals lymphocytosis, the presence of erythrocytes (in the hemorrhagic form), elevated protein levels, and reduced or normal glucose levels.
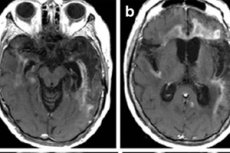
The main imaging method is nuclear MRI. It is used for emergency indications. In addition, it allows to clarify whether the patient can undergo a lumbar puncture for analysis. Herpes encephalitis on MRI shows increased signals in the temporal lobes or insular region of the cerebral cortex, on the surface of the orbital frontal gyri, which are characterized by unilaterality or bilateral damage with no symmetry. These results lack specificity, but together with clinical symptoms and laboratory data, in most cases they allow an accurate diagnosis. [ 41 ]
Early diagnostics do not always confirm the diagnosis: in 10% of patients, CSF microscopy and MRI data, and in 5%, PCR results are false negative. [ 42 ] However, in most patients, at least some examination confirms the diagnosis, and subsequent visualizations reveal obvious and progressive changes - the presence of edema and hemorrhage, diffuse spread of lesions.
Differential diagnosis
First of all, it is necessary to identify the origin of the pathogen, since the main treatment is aimed at neutralizing it: viral encephalitis requires massive antiviral therapy, bacterial encephalitis requires antibiotics, parasitic encephalitis requires appropriate antiparasitic drugs, etc. In this sense, the results of tests, especially PCR, play a decisive role. [ 43 ], [ 44 ]
Herpetic encephalitis must be distinguished from multiple sclerosis, neoplasms, abscesses, cerebral circulatory disorders, for example, in the case of a stroke in the middle cerebral artery basin, the basal ganglia are usually damaged (which is visible on MRI), while in the case of herpetic encephalitis they are not affected, myelitis - inflammation of the spinal cord, especially since disseminated neuroinfection often spreads to areas of the spinal cord (herpetic encephalomyelitis).
The HSV-2 virus causes inflammation in the soft membranes of the brain (herpetic meningitis) more often than HSV-1, although it is rarely localized. The inflammation quickly spreads to the brain matter - neurons and glial cells, and herpetic meningoencephalitis develops. If the origin of the pathogen is established, the treatment principle is similar (antiviral therapy). But the affected area is larger, and complications and consequences can be more serious. It is differentiated based on the results of instrumental studies.
Who to contact?
Treatment herpetic encephalitis
Patients with suspected acute brain damage from the herpes simplex virus are necessarily hospitalized, and in the intensive care unit. [ 45 ] This is due to the high probability of developing a coma, respiratory failure, swallowing disorder, and other vital function disorders that cannot be maintained at home.
At the initial stage, it is recommended to administer the antithrombotic drug Curantil three times a day in a single dose of 25-50 mg. This is done to prevent ischemic cerebral circulation disorders.
The main treatment is etiotropic, aimed at reducing the activity of the herpes virus (it is currently not possible to completely destroy it). The drug of choice is Acyclovir and its synonyms, which are especially effective against the herpes viruses HSV-1 and HSV-2. Timely antiviral therapy can increase the patient's chances of a favorable outcome of the disease and minimal complications.
Acyclovir is a drug that targets so-called molecular targets, a purine analogue of guanine, a component of nucleic acids. A similar structure allows acyclovir to penetrate the virus cell and, interacting with its enzymes, turn into acyclovir triphosphate, which, when integrated into the viral DNA chain, interrupts the process of reproduction of the pathogenic microorganism. And most importantly, Acyclovir does not have a significant effect on the genetic apparatus of human cells and promotes the mobilization of immunity.
Patients with severe forms of herpes encephalopathy with the development of coma are prescribed acyclovir in a single dose of 10-15 mg per kilogram of the patient's weight three times a day intravenously. It is usually given by drip, since the drug must be administered into the vein very slowly. The course of treatment is from one to two weeks. The advantage of acyclovir in HSVE was established by two landmark clinical trials conducted in the mid-1980s. Whitley et al. [ 46 ]. Current guidelines recommend using acyclovir intravenously for 14-21 days in cases of HSV. [ 47 ]
In milder cases of the disease, if the patient can swallow medications on his own, a tablet form of the drug may be prescribed.
Acyclovir is also available in tablets. The dose is prescribed by a doctor depending on the patient's condition and age, since encephalitis is treated with high doses of the drug. For patients with severe forms of renal failure, the dose is adjusted. Tablets are taken for therapeutic purposes up to five times a day.
If possible, Valaciclovir is sometimes preferred. This is a more modern drug, the advantage of which is that it acts prolonged and can be taken less often than its predecessor. In the body, the active substance is broken down into acyclovir, which has the main, antiherpetic effect, and valine, an aliphatic acid, a natural ingredient of proteins. In herpes encephalitis, the ability of this substance to protect and regenerate the myelin sheath of nerve fibers is valuable. Valine increases the energy potential of the body's muscle cells, improves coordination of movements, stimulates cellular synthesis and promotes tissue renewal.
These antiviral drugs are contraindicated for people with hypersensitivity to acyclovir. For vital indications, they are prescribed to pregnant women, since the drug's teratogenicity has not been identified, however, complete safety has not yet been proven. Valaciclovir is not prescribed to children. Side effects from taking it are headache, nausea, hematopoiesis disorders and renal excretory function.
Recent studies have shown that the anti-flu drug Arbidol is also active against the herpes simplex virus type 2. In addition to its viral static ability, it also stimulates interferon synthesis, humoral and cellular immunity.
Other immunomodulators may be prescribed, such as Laferobion, which is human interferon, or Levamisole. The dosage and duration of taking drugs to stimulate the immune system is prescribed by a doctor. They are usually used for a short period of time, from three to five days. They can also cause allergic reactions and are not recommended for people with chronic diseases of the heart, blood vessels, liver, and kidneys.
To reduce inflammation and prevent cerebral edema, glucocorticosteroids (Prednisolone, Medrol, Dexamethasone) are prescribed. [ 48 ] Their usefulness in encephalitis is not recognized by all specialists, since corticosteroids have both a strong anti-inflammatory and immunosuppressive effect, which can theoretically promote viral replication. It is not surprising that there are different opinions regarding their use in HSVE [ 49 ], [ 50 ] and the number of side effects is frightening, so pulse therapy is carried out in a short course. When taking them, the dosage and regimen should not be violated under any circumstances. A non-randomized retrospective study of 45 patients with HSV showed that the addition of corticosteroids to acyclovir may be associated with improved results, [ 51 ], which encourages larger-scale clinical trials.
B vitamins are prescribed to improve the functioning of the central nervous system, maintain normal metabolism in the brain, and restore the myelin sheaths of nerve fibers. The most important for the functioning of the nervous system are thiamine, pyridoxine, and cyanocobalamin (B1, B6, B12). Thiamine normalizes the conduction of nerve impulses, pyridoxine strengthens the myelin sheath of nerve fibers and the production of neurotransmitters. Cyanocobalamin complements all of the above effects, and also stimulates the conduction of nerve impulses to the distal parts of the nervous system. This group of vitamins helps to normalize hematopoiesis, which is important for such a serious disease and serious drug therapy.
They can be taken in tablets (Neurorubin, Neurobion) or injected - each separately, alternating with each other. This option is considered preferable.
Ascorbic acid is also administered, the daily dose of which should be no less than 1.5 g.
If the patient is in a state of psychomotor agitation, he may be prescribed antipsychotics, in case of epileptiform seizures - anticonvulsants, nootropics and antihypertensive drugs are also used.
Treatment is symptomatic, aimed at stabilizing the work of all organs and systems - dehydration therapy (diuretics) is carried out, in severe cases - detoxification. Vital functions of the body are supported - respiratory, if necessary, artificial ventilation of the lungs is carried out; water-electrolyte balance, rheological properties and composition of blood, etc. are normalized.
Deoxyribonuclease may be prescribed, and in case of secondary bacterial infection, a course of antibacterial therapy. [ 52 ]
Almost any drug can cause an allergic reaction in a patient, so desensitizing drugs (Diphenhydramine, Suprastin, Claritin) are necessarily included in the treatment regimen.
During the recovery period, the patient may also need medication support and physical therapy.
Herpetic encephalitis is too serious a disease, and it is not advisable to rely on folk treatment in this case. The outcome of the disease directly depends on the speed of the start of antiviral therapy. In the past, before the discovery of antiherpetic drugs, the mortality rate was from 70 to 100%. So, hoping for herbal treatment, you can only miss time and a chance for recovery. However, folk medicine recipes can be useful in the recovery period. Medicinal herbs can relieve headaches, reduce anxiety, and reduce restlessness. Motherwort, valerian, mint, and peony are suitable for this. St. John's wort is known as a natural antidepressant, and echinacea is an immunomodulator. However, it is better to use herbal treatment under the supervision of a qualified herbalist.
Homeopathy can also be useful during the recovery period; it has many means for detoxification, normalization of the nervous system, and strengthening the immune system, but during acute herpes encephalitis it is better to contact an infectious disease specialist as soon as possible.
Surgical treatment of herpetic encephalitis is not used, but if complications such as focal drug-resistant epilepsy develop, brain surgery may be recommended to eliminate the source of the pathology. Such operations are performed according to individual strict indications.
Prevention
The main goal of preventive tactics is to avoid herpes infection. This can be compared to attempts to protect against respiratory viral infections. First of all, good immunity can help, for which you need to lead a healthy lifestyle: eat well and varied, combine feasible physical activity with rest, increase your stress resistance, since no one can completely avoid stress in the modern world, give up habits that are harmful to health. Practice shows that the herpes virus is very common, however, some people are resistant to infection, and they should thank only their own immune system for this.
However, if you see a person with obvious symptoms of labial herpes, you should not hug or kiss them tightly. If this is your relative, they should have separate dishes and hygiene items, however, they should always be individual.
It is worth remembering that the disease in the acute stage can also be transmitted by airborne droplets. Therefore, if possible, it is worth disinfecting exposed parts of the body that could have been contaminated with microparticles of secretion (face, neck), and rinsing the mouth.
Barrier contraceptives and treating the genitals with an antiseptic after contact partially protect against genital herpes. But the best protection is to avoid casual sex.
If infection could not be avoided, consult a doctor and regularly undergo a course of recommended antiviral therapy. You can resort to traditional medicine methods, consult a homeopath. Such measures will help keep the herpes virus under control and will be a good prevention of its reactivation and the development of serious complications.
Forecast
Timely initiation of antiviral therapy significantly increases the chances of a favorable prognosis even in severe forms of herpes encephalitis. Without treatment, herpes encephalitis leads to death or severe disability in the vast majority of cases. Currently, a fourth to fifth of inflammations of the brain tissue caused by the herpes virus end in an unfavorable outcome. The fulminant form of the disease is especially dangerous, and the spread of the inflammatory process to the soft membranes of the brain (meningoencephalitis) leaves more severe consequences.
The mortality rate from untreated HSV encephalitis is approximately 70%, and 97% of survivors will not return to their previous level of function.[ 53 ],[ 54 ]
Among the most significant negative prognostic factors are older age, coma/lower level of consciousness at presentation, restricted diffusion on DWI, and delay in taking acyclovir.
The sluggish process is dangerous due to the length of the latent period, as a result of which, by the time the patient seeks help, there are already extensive and irreversible lesions of the cerebral structures.

