Medical expert of the article
New publications
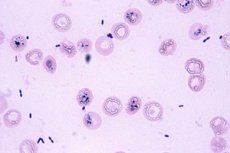
Gonococcus in the smear
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Normally, there should be no gonorrhea pathogen (Neisseria gonorrhoeae) in a smear of secretions from the genital tract. This infectious agent causes serious diseases of the genitourinary system, which are fraught with chronicity and impaired fertility, as well as the development of gonococcal sepsis. Gonococci are not uncommon in a smear. This is the second most common sexually transmitted infection after chlamydia. Of particular danger is the asymptomatic course of gonorrhea in the young part of the female population of fertile age. In this category of patients, the infection quickly becomes complicated by inflammatory diseases of the pelvic organs, which, if left untreated, can lead to persistent infertility.
Therefore, if gonococci are found in the smear, this means that urgent measures must be taken to neutralize the infection and protect your genitourinary system. Simply put, you need to get treatment. You can retake the smear if there are no obvious signs of illness, however, ignoring such unpleasant news is more expensive for yourself. Having received a negative result during the retake, you also do not need to relax. The result can be affected by treatment with antibacterial drugs for a completely different reason, washing with an antiseptic and visiting the toilet before the procedure. A competent medical consultation is mandatory in any case.
How can you get infected?
The most likely route of transmission of the infection is unprotected sex in any form: genital, anal, oral, petting (it is enough to touch the mucous membrane with secretions from infected genitals; to become infected from hands with fresh infected secretions touching the genitals). The vertical route of transmission - from a sick mother to her child during childbirth also carries a high risk of infection.
Gonorrhea is rarely transmitted through everyday life, since the pathogen is very unstable and quickly dies in the external environment. But it is still impossible to completely exclude this transmission route, although it is necessary to completely neglect generally accepted sanitary standards, for example, to use one bath towel or washcloth, and without waiting for this object to dry. Women are at a greater risk of getting the pathogen in this way. Women generally become infected during unprotected sexual contact with an infected partner in 85% of cases, while for men this probability is 30-40%. This is facilitated by anatomical differences in the structure of the genitals.
Gonococci and trichomonads in a smear, as well as other pathogenic microbes - combined infection is common, even more common than monoinfection. At the same time, some researchers believe that the danger of infection with trichomonads lies in their mobility and ability to transport other pathogens, in particular, gonococci, spreading them to deeper organs. Symptoms in these cases may be blurred, but laboratory diagnostics - a classic smear of vaginal (urethral) discharge, bacterial culture for microflora, as well as more modern methods - polymerase chain reaction, determination of antibodies will help to dot the dots in diagnostics.
As practice shows, inflammation in the vast majority of cases develops at the site of the primary introduction of the infectious agent. Infection during genital contact in women is localized mainly in the urethra and paraurethral passages, Bartholin's glands, at the entrance to the vagina, cervix, anus. The introduction of gonococcus directly into the vaginal wall (colpitis) occurs more often in pregnant women, since during this period the multilayered squamous epithelium, practically inaccessible to damage by these infectious agents, undergoes structural transformations due to hormonal changes - it becomes loose, saturated with blood vessels, which facilitates its penetration. With ascending gonorrhea, the fallopian tubes, uterus, ovaries are infected. In representatives of the stronger sex, everything is simpler - the primary inflammation is localized in the urethra.
Extragenital forms of gonococcal infection are localized on the mucous membrane of the oral cavity and conjunctiva of the eyes.
An extremely rare, but possible localization is in other organs due to the migration of the pathogen through the blood or lymphatic vessels (metastatic form).
How does the disease manifest itself?
Gonococci in a smear in women may well become an unpleasant surprise as a result of a preventive examination by a gynecologist. In women, biomaterial for research is taken from the mucous membrane of the vagina, cervical canal and urethra. If necessary, the microflora of the rectum, back wall of the pharynx, tonsils and oral cavity can be examined.
In most patients (about 70%), gonorrhea is asymptomatic or has mild symptoms. On average, symptoms appear within the first three to five days after infection, although sometimes the latent period can last for two weeks. These are mainly various disturbances in the process of emptying the bladder (dysuria) and yellowish-white vaginal discharge.
The condition may be complicated by nagging pains in the lower abdomen above the pubis or on the side. In cases of ascending infection to the uterus, appendages and pelvic area of the peritoneum, mucopurulent discharge may have bloody streaks, the menstrual cycle is disrupted. The uterus becomes painful, its enlargement and softening are detected upon palpation. The appendages may become clogged with pus, these accumulations may be mistaken for a neoplasm by the doctor upon palpation. The peritoneum becomes inflamed, which threatens the development of peritonitis.
The appearance of such symptoms does not directly indicate the presence of gonococcal infection, but should be a reason for examination.
In about a third of infected women, the disease is acute with abundant purulent discharge, itching and swelling of the external genitalia, pain in the lower abdomen, frequent urination, accompanied by severe discomfort, sometimes accompanied by a high temperature (from 38.5 to 40℃). If a woman decides to "treat" herself and takes a course of antibiotics, temporary relief may occur, acute symptoms will go away, however, there is a high probability that the infection will remain, become chronic and someday manifest itself with unexpected and severe complications.
The presence of accidentally detected gonococci in a woman's smear indicates that she was infected and is a carrier of gonorrhea pathogens. The absence of symptoms does not indicate well-being; pathological changes occur in the microflora of the vagina and cervical canal, which over time affect various organs of the genitourinary system. Chronic infection leads to irreversible consequences - tubal obstruction, leading to persistent fertility problems, the development of ectopic pregnancy, any other organs and systems can be affected. A fairly rare but severe complication - gonorrheal sepsis can end in death.
Gonorrhea in men usually manifests itself with pronounced symptoms of gonorrheal urethritis. Purulent discharge from the urethra, which becomes more and more abundant, hyperemic and edematous outlet of the urethra, discomfort during the process of urination - burning, later, when the process spreads to the back urethra, frequent urges join, a feeling of incomplete emptying of the bladder and other unpleasant symptoms usually force a man to see a doctor. Biological material for research is taken from the urethra by inserting a special sterile probe into it. Before the procedure, the patient's prostate gland and urethra are massaged.
Accidentally detected gonococci in a smear in men with a torpid (asymptomatic) course are extremely rare, however, such patients are a source of multiple infections. In addition, this category of patients, as well as those who try to cure themselves or simply ignore the disease, are a reserve for replenishing patients with epidemitis, prostatitis, infertility and impotence. Untreated chronic gonorrhea can lead to scarring and strictures of the urethra, threatening complete impossibility of emptying the bladder.
Therefore, if a man has stains on his underwear from minor and undisturbing discharge, in the mornings the lips at the exit of the urethra slightly stick together, the urine has become cloudy, there is slight discomfort when emptying the bladder, it is necessary to undergo an examination immediately. Unpleasant sensations during the examination are not comparable to the consequences of an advanced disease.
Gonococci in a smear in pregnant women are subject to mandatory eradication. The patient could have been infected both before and during pregnancy. If the infection was latent, pregnancy could have provoked an exacerbation. The vast majority of infected expectant mothers have chronic forms of damage to the lower parts of the genitourinary system. During pregnancy, a smear for gonococci is examined twice - upon application and before maternity leave. Women themselves seek help for suspected gonorrhea extremely rarely - either during an acute illness with pronounced symptoms, or during an exacerbation of severe complications. The inflammatory process in an acute form during infection of a pregnant woman is accompanied by more noticeable symptoms than in the presence of chronic gonorrhea.
This disease in a pregnant woman can cause serious health problems for herself and the newborn. The child often becomes infected when passing through the infected birth canal of the mother - in this case, the newborn of either sex develops glenoblenorrhea, leading to blindness. In girls, the genitals can become infected, which will lead to gonorrheal vulvovaginitis of the newborn. Sepsis in newborns can also be caused by the presence of a gonococcal infection in the mother.
For a woman, this disease is fraught with complications during pregnancy, premature birth, and fetal death. With chronic ascending gonorrhea, a woman often develops a habitual miscarriage.
Childbirth is a provoking factor for the spread of infection beyond the internal os of the uterus.
So, if gonococci are detected in a smear, then a patient of any gender is diagnosed with gonorrhea. This disease requires immediate treatment by a venereologist. Otherwise, the consequences can be very sad. In addition to the genitourinary system, gonococci can affect not only the genitourinary organs, but also joints, musculoskeletal tissue, as well as the liver, heart, and brain through the lymphogenous and hematogenous pathways.
Treatment
Acute gonorrhea is the easiest to treat; if the disease has become chronic, treatment may be longer and multi-stage, however, provided that the patient follows all medical instructions and does not stop treatment when the first signs of improvement appear, it is quite possible to destroy the infection.
Gonococci are sensitive to antibiotics. Previously, penicillins were used for their eradication. Modern pathogens have acquired resistance to this group of drugs, so antibiotics belonging to the fluoroquinolone and cephalosporin series are more often prescribed. The main principles observed in the treatment of gonorrheal infection are the choice of a drug to which the detected gonococcus is sensitive, and the selection of a single and course dose sufficient for its eradication.
Nowadays, combined infection, for example, with trichomoniasis, is increasingly common. These parasites are indifferent to antibiotics, which do not penetrate the membranes of the cytoplasm of trichomonads. In case of combined infection with these parasites, the gonococci phagocytosed by them, preserved in trichomonads after treatment, can be a source of recurrent gonorrhea. Therefore, in this case, complex treatment is necessary.
Premature interruption of the course of therapy is not allowed, since even in the absence of symptoms, gonococci can remain in the body, acquire resistance to previously used drugs and in the event of a subsequent relapse, it will be almost impossible to eradicate them. After the therapeutic course, a thorough examination is mandatory. The criteria for successful treatment are the absence of: symptoms of infection and gonococci in a smear from the urethra, cervical canal and anus.
All sexual partners of the sick individual must undergo examination. Female children are subject to examination if gonococci are detected in a smear of one of the parents.
The patient and his relatives must observe the rules of personal hygiene.
Patients are advised to drink plenty of fluids, avoid spicy foods and alcoholic beverages during treatment, limit physical activity, avoid going to the pool, sauna, or swimming in open water.
Immunity does not develop after an infection, and you can become infected as many times as you like. The most reliable way to prevent infection is barrier contraception (a condom).
The following actions can help reduce the risk of infection after unprotected sexual contact - immediately emptying the bladder and washing the external genitals using laundry soap, an antiseptic, such as miramistin or chlorhexidine. They can be used within two hours after sex, however, these methods do not guarantee avoiding infection, their effectiveness decreases exponentially with the time that has passed since unprotected contact. Due to differences in the anatomy of the genitals, such measures are more effective for males.


 [
[