Medical expert of the article
New publications
Upper jaw fracture
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
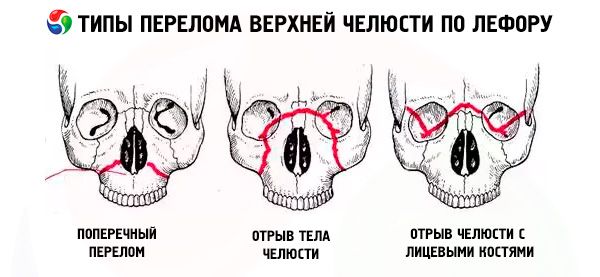
A fracture of the maxilla usually follows one of the three typical lines of least resistance described by Le Fort: upper, middle and lower. They are commonly called Le Fort's lines (Le Fort, 1901).
- Le Fort I - the lower line, has a direction from the base of the pyriform aperture horizontally and back to the pterygoid process of the sphenoid bone. This type of fracture was first described by Guerin, and Le Fort also mentions it in his work, so the fracture along the lower line should be called the Guerin-Le Fort fracture.
- Le Fort II - the midline, passes transversely through the nasal bones, the floor of the orbit, the infraorbital margin, and then down along the zygomaticomaxillary suture and the pterygoid process of the sphenoid bone.
- Le Fort III is the upper line of least strength, passing transversely through the base of the nasal bones, the floor of the orbit, its outer edge, the zygomatic arch and the pterygoid process of the sphenoid bone.
In the case of a Le Fort I fracture, only the dental arch of the upper jaw together with the palatine process is mobile; in the case of a Le Fort II fracture, the entire upper jaw and nose are mobile, and in the case of a Le Fort III fracture, the entire upper jaw together with the nose and zygomatic bones. The mobility indicated may be unilateral or bilateral. In the case of unilateral fractures of the upper jaw, the mobility of the fragment is less pronounced than in the case of bilateral fractures.
Fractures of the upper jaw, especially along the Le Fort III line, are often accompanied by damage to the base of the skull, concussions, bruises or compression of the brain. Simultaneous damage to the jaw and brain is often the result of severe and severe trauma: a blow to the face with a heavy object, compression, a fall from a great height. The condition of patients with a fracture of the upper jaw is significantly aggravated by damage to the walls of the paranasal sinuses, the nasal part of the pharynx, the middle ear, the meninges, the anterior cranial fossa with the nasal bones driven into it, and the walls of the frontal sinus. As a result of a fracture of the walls of this sinus or the ethmoid labyrinth, emphysema of the subcutaneous tissue in the eye socket, forehead, and cheek may occur, which is manifested by the characteristic symptom of crepitus. Crushing or rupture of the soft tissues of the face is often observed.
 [ 1 ]
[ 1 ]
Symptoms of a fractured upper jaw
Fractures of the base of the skull are accompanied by the symptom of "bloody glasses", subconjunctival suffusion (blood soaking), retroauricular hematoma (in case of a fracture of the middle cranial fossa), bleeding and especially liquorrhea from the ear and nose, dysfunction of the cranial nerves and general neurological disorders. Most often, the branches of the trigeminal, facial and oculomotor nerves are damaged (loss of sensitivity, disturbance of facial expressions, pain when moving the eyeballs upward or to the sides, etc.).
The rate of development of hematomas is of great diagnostic importance: fast - indicates its local origin, and slow - over 1-2 days - is typical for indirect, deep bleeding, i.e. a fracture of the base of the skull.
Diagnosis of fractures of the upper jaw, compared to injuries of the lower jaw, is a more complex task, since they are often accompanied by rapidly increasing swelling of soft tissues (eyelids, cheeks) and intra-tissue hemorrhages.
The most typical symptoms of a fracture of the upper jaw:
- lengthening or flattening of the middle part of the face due to the displacement of the torn jaw downward or inward (backward);
- pain when trying to close the teeth;
- malocclusion;
- bleeding from the nose and mouth.
The latter is especially pronounced in fractures along the Le Fort III line. In addition, fractures of the upper jaw are often impacted, which makes it difficult to detect the main symptom of a fracture of any bone - displacement of fragments and their pathological mobility. In such cases, diagnosis can be aided by flattening of the middle third of the face, malocclusion and the step symptom, revealed by palpation of the edges of the orbits, zygomatic arches and zygomatic-alveolar ridges (the area where the zygomatic process of the upper jaw and the maxillary process of the zygomatic bone join) and caused by a violation of the integrity of these bone formations.
To increase the accuracy of diagnosis of fractures of the upper jaw, one should take into account the pain during palpation of the following points, corresponding to areas of increased extensibility and compression of the bones:
- superior nasal - at the base of the root of the nose;
- lower nasal - at the base of the nasal septum;
- supraorbital - along the upper edge of the eye socket;
- extraorbital - at the outer edge of the eye socket;
- infraorbital - along the lower edge of the eye socket;
- zygomatic;
- arched - on the zygomatic arch;
- tuberal - on the tubercle of the upper jaw;
- zygomatic-alveolar - above the area of the 7th upper tooth;
- canine;
- palatine (points are palpated from the side of the oral cavity).
Symptoms of mobility of the upper jaw fragments and a "floating palate" can be identified as follows: the doctor grasps the anterior group of teeth and the palate with the fingers of his right hand, and places his left hand on the cheeks from the outside; then makes light rocking movements forward-down and back. In case of impacted fractures, the mobility of the fragment cannot be determined in this way. In these cases, it is necessary to palpate the pterygoid processes of the sphenoid bones; in this case, the patient usually feels pain, especially in case of fractures along the Le Fort II and III lines, sometimes accompanied by a number of the above-mentioned symptoms of a fracture of the base of the skull, ethmoid labyrinth, nasal bones, lower walls of the orbits and zygomatic bones.
In patients with injuries to the upper jaw and frontal bone, fractures of the walls of the maxillary sinuses, lower jaw and zygomatic bones, ethmoid labyrinth and nasal septum are possible. Therefore, with combined fractures of the base of the skull, upper jaw, zygomatic bones, nasal septum and lacrimal bones, intense lacrimation and liquorrhea from the nose and ears may occur.
The combination of fractures of the upper jaws with traumatic damage to other parts of the body in most cases is clinically manifested by a particularly severe syndrome of mutual aggravation and overlap. Patients with such a combination should be classified as victims with an increased risk of developing general septic complications not only in the maxillofacial region, but also in other foci of damage of distant localization (as a result of metastasis of infection), including closed ones that do not have a direct anatomical connection with the jaws, oral cavity, face.
Many patients with fractures of the upper jaws experience some degree of traumatic neuritis of the infraorbital branches of the trigeminal nerve; some victims experience prolonged decreased electrical excitability of the teeth on the side of the injury.
Of certain diagnostic significance is the detection by palpation of irregularities in the edges of the orbit (step-like protrusions), zygomatic-alveolar ridges, nasolabial sutures, as well as changes in the edges of the upper jaw during radiography in axial and frontal projections.
Outcomes of jaw fractures
The outcome of jaw fractures depends on many factors: the age and general condition of the victim prior to the injury, the presence of mutual aggravation syndrome, the environmental situation in the area of the victim's permanent residence; in particular, on the presence of an imbalance of mineral elements in water and food (G. P. Ruzin, 1995). Thus, according to G. P. Ruzin, in residents of different areas of the Ivano-Frankivsk region, the course of fractures and the nature of the studied metabolic processes are almost identical and can be considered optimal, while in the Amur region, the process of bone tissue regeneration and metabolic reactions are slower. The frequency and nature of complications depend on the period of adaptation of the individual in this area. The indicators he used: the inflammatory response index (IRI), the metabolic index (MI), the regeneration index (RI) - allow analyzing the totality of changes in the studied indicators even in cases where changes in each of them do not go beyond the physiological norms. Therefore, the use of the IVR, MI and RI indices makes it possible to predict the course of a fracture, the development of an inflammatory-infectious complication, to draw up a treatment plan for a patient in order to optimize metabolic processes, prevent complications and monitor the quality of treatment taking into account the patient's characteristics and external conditions. For example, for the Ivano-Frankivsk region, the critical values of the indices are: IVR - 0.650, MI - 0.400, RI - 0.400. If lower figures are obtained, corrective therapy is necessary. Metabolic optimization is not required if IVR> 0.6755, MI> 0.528, RI> 0.550. The author has established that in different regions the index values may vary depending on the medical-geographical and biogeochemical conditions that must be taken into account when analyzing them. Thus, in the Amur region these values are lower than in the Ivano-Frankivsk region. That is why it is advisable to conduct an assessment of the IVR, MI and RI in conjunction with a clinical and radiological examination of the patient in the first 2-4 days after the injury - to identify the initial level of regenerative potential and prescribe the necessary corrective therapy, on the 10th-12th day - to clarify the treatment being carried out, on the 20th-22nd day - to analyze the results of treatment and predict the characteristics of rehabilitation.
According to G. P. Ruzin, in regions with hypo- and discomfort conditions, the presence of an imbalance of mineral components and amino acid composition of proteins during the adaptation period, it is necessary to include anabolics and adaptogens in the treatment complex. Among all the physical factors used by him, laser radiation had the most pronounced positive effect.
Based on his research, the author summarizes practical recommendations as follows:
- It is advisable to use tests that characterize the conditions of metabolism and the reparative process: inflammatory response index (IRI), metabolic index (MI), regeneration index (RI).
- If the IVR is below 0.675, it is necessary to use osteotropic antibiotics; if the IVR is above 0.675, with timely and adequate immobilization, antibiotic therapy is not indicated.
- If MI and RI values are less than 0.400, therapy is required that includes a complex of drugs and agents that stimulate protein and mineral metabolism.
- At low IVR values, the use of local thermal procedures (UHF) is contraindicated until the inflammatory focus is resolved or drained.
- When treating patients with fractures of the lower jaw in unfavorable medical and geographical conditions, especially during the adaptation period, adaptogens, anabolics and antioxidants should be prescribed.
- In order to quickly resolve the infiltrate and reduce the duration of pain, it is advisable to use laser irradiation in the first 5-7 days after the injury.
- To optimize the treatment of patients with a fracture of the lower jaw and reduce the duration of hospitalization, it is necessary to organize rehabilitation rooms and ensure continuity at all stages of treatment.
With timely pre-hospital, medical and specialized care, the outcomes of jaw fractures in adults are favorable. For example, V. F. Chistyakova (1980), using a complex of antioxidants for the treatment of uncomplicated fractures of the lower jaw, was able to reduce the length of stay of patients in hospital by 7.3 bed-days, and V. V. Lysenko (1993), when treating open fractures, i.e., obviously infected with oral microflora, using intraoral nitazole foam aerosol, reduced the percentage of traumatic osteomyelitis by 3.87 times, also reducing the period of antibiotic use. According to K. S. Malikov (1983), when comparing the radiographic picture of the process of reparative regeneration of the lower jaw with autoradiographic indices, a specific pattern in bone mineral metabolism was established: an increase in the intensity of the inclusion of the radioactive isotope 32 P and 45 Ca in the bone regenerate of the damaged lower jaw is accompanied by the appearance of radiographic areas of calcification in the terminal sections of the fragments; the dynamics of the absorption of radiopharmaceuticals occurs in the form of two phases of the maximum concentration of labeled compounds 32 P and 45 Ca in the injury zone. As the bone fragments heal in fractures of the lower jaw, the degree of intensity of the inclusion of isotopes 32 P, 45 Ca in the injury zone increases. The maximum concentration of osteotropic radioactive compounds in the terminal sections of the fragments is observed on the 25th day after the jaw injury. The accumulation of macro- and microelements in the terminal sections of the fragments of the lower jaw has a phasic character. The first increase in the concentration of minerals is observed on days 10-25, the second on days 40-60. At later stages of reparative regeneration (120 days), mineral metabolism in the fracture zone begins to gradually approach normal parameters, and by the 360th day it is completely normalized, which corresponds to the process of final reorganization of the bone callus that connected the fragments of the lower jaw. The author found that timely and correct anatomical alignment of fragments and their reliable surgical fixation (for example, with a bone suture) leads to early (25 days) bone fusion of the lower jaw fragments and restoration (after 4 months) of the normal structure of newly formed bone tissue, and its study by biochemical and spectral research methods in comparison with morphological and autoradiographic data showed that the degree of saturation of the callus microstructures with minerals gradually increases with increasing maturity of the bone tissue.
In case of untimely use of complex treatment, the above-mentioned and other inflammatory complications (sinusitis, arthritis, migrating granuloma, etc.) may occur, false joints may form, cosmetic disfigurement of the face may occur, chewing and speech disorders may occur, and other non-inflammatory diseases may develop that require complex and long-term treatment.
In cases of multiple jaw fractures in elderly and senile individuals, delayed fusion, pseudoarthrosis, osteomyelitis, etc. are often observed.
In some cases, the treatment of post-traumatic complications requires the use of complex orthopedic structures in accordance with the nature of the functional and anatomical-cosmetic disorders, as well as reconstructive surgeries (osteoplasty, refracture and osteosynthesis, arthroplasty, etc.).
Diagnosis of fracture of the upper jaw
X-ray diagnostics of maxillary fractures is often very difficult, since the X-rays in the lateral projection show a superposition of two maxillary bones. Therefore, X-rays of the maxilla are usually taken in only one (sagittal) projection (survey X-ray), and attention should be paid to the contours of the zygomatic alveolar ridge, infraorbital margin and the borders of the maxillary sinuses. Their violation (kinks and zigzags) indicates a fracture of the maxilla.
In case of craniofacial disjunction (fracture along the Le Fort III line), radiography of the facial skeleton in the axial projection is of great help in establishing the diagnosis. In recent years, tomography and panoramic radiography have also been successfully used.
In recent years, diagnostic technologies (computer tomography, magnetic resonance imaging) have appeared that allow for the simultaneous diagnosis of damage to both the facial and cranial skull. Thus, Y. Raveh et al. (1992), T. Vellemin, I. Mario (1994) divided fractures of the frontal, maxillary, ethmoid bones, and orbit into two types and one subtype - (1a). Type I includes fronto-nasal-ethmoid and medial-orbital fractures without damage to the bones of the skull base. In subtype 1a, damage to the medial wall of the optic canal and compression of the optic nerve are also added to this.
Type II includes frontal-nasal-ethmoid and medial-orbital fractures involving the skull base; in this case, the internal and external parts of the facial and cranial skull are damaged with intracranial displacement of the posterior wall of the frontal sinus, the anterior part of the skull base, the upper wall of the orbit, the temporal and sphenoid bones, and the sella turcica region; there are ruptures of the dura mater. This type of injury is characterized by cerebrospinal fluid leakage, hernial protrusion of brain tissue from the fracture gap, the formation of bilateral telecanthus with spreading of the interorbital region, and compression and damage of the optic nerve.
Such detailed diagnostics of complex craniofacial trauma allows, 10-20 days after the injury, to compare bone fragments of the base of the skull and face simultaneously, which makes it possible to reduce the length of hospital stay for victims and the number of complications.
What do need to examine?
How to examine?
Who to contact?
Providing assistance to victims with maxillofacial trauma
Treatment of patients with jaw fractures involves restoring the lost form and function as quickly as possible. The solution to this problem includes the following main stages:
- alignment of displaced fragments,
- securing them in the correct position;
- stimulation of bone tissue regeneration in the fracture area;
- prevention of various types of complications (osteomyelitis, pseudoarthrosis, traumatic sinusitis, perimaxillary phlegmon or abscess, etc.).
Specialized care for jaw fractures should be provided as early as possible (in the first hours after the injury), since timely repositioning and fixation of fragments provide more favorable conditions for bone regeneration and healing of damaged soft tissues of the oral cavity, and also help stop primary bleeding and prevent the development of inflammatory complications.
The organization of assistance to victims with maxillofacial trauma must provide for the continuity of medical measures along the entire route of the victim from the scene of the incident to the medical institution with mandatory evacuation to the destination. The scope and nature of the assistance provided may vary depending on the situation at the scene of the incident, the location of medical centers and institutions.
A distinction is made between:
- first aid, which is provided directly at the scene of an incident, at medical posts and is carried out by victims (in the order of self- or mutual assistance), an orderly, or a medical instructor;
- pre-medical care provided by a paramedic or nurse and aimed at supplementing first aid measures;
- first medical aid, which should be provided, if possible, within 4 hours from the moment of injury; it is carried out by non-specialist doctors (in rural district hospitals, at medical centers, and ambulance stations);
- qualified surgical care, which must be provided in medical institutions no later than 12-18 hours after the injury;
- specialized care that must be provided in a specialized institution within one day after the injury. The given timeframes for providing various types of care are optimal.
 [ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
[ 4 ], [ 5 ], [ 6 ], [ 7 ], [ 8 ]
First aid at the scene
Favorable outcomes of treatment of maxillofacial injuries largely depend on the quality and timeliness of first aid. Not only the health, but sometimes the life of the victim, especially in the event of bleeding or asphyxia, depend on its proper organization. Often, one of the main features of maxillofacial injuries is the discrepancy between the type of the victim and the severity of the injury. It is necessary to draw the attention of the population to this feature by conducting health education work (in the Red Cross system, during civil defense classes).
The medical service should pay great attention to training in first aid techniques, especially for workers in those industries where the incidence of injuries is quite high (mining, agriculture, etc.).
When providing first aid to a victim with a facial injury at the scene of the incident, first of all it is necessary to put the victim in a position that prevents asphyxia, i.e. lay him on his side, turning his head towards the injury or face down. Then an aseptic bandage should be applied to the wound. In case of chemical burns of the face (acids or alkalis), it is necessary to immediately wash the burned surface with cold water to remove the remains of the substances that caused the burn.
After first aid has been provided at the scene of the incident (medical post), the victim is evacuated to a medical aid station, where first aid is provided by mid-level medical personnel.
Many patients with maxillofacial injuries can independently reach medical centers located near the scene of the incident (health centers of factories, plants). Those victims who cannot move independently are transported to medical institutions in compliance with the rules for preventing asphyxia and bleeding.
First aid for injuries to the maxillofacial region can be provided by mid-level medical workers called to the scene of the incident.
 [ 9 ]
[ 9 ]
First aid
Like emergency aid, life-saving aid is provided at the scene of an incident, at medical posts, in health centers, paramedic and paramedic-obstetric stations. In this case, efforts should be aimed primarily at stopping bleeding, preventing asphyxia and shock.
Mid-level medical workers (dental technician, paramedic, midwife, nurse) must know the basics of diagnosing facial injuries, elements of first aid and the specifics of transporting patients.
The amount of pre-hospital care depends on the nature of the injury, the patient's condition, the environment in which this care is provided, and the qualifications of the medical workers.
Medical personnel must determine the time, place and circumstances of the injury; after examining the victim, make a preliminary diagnosis and carry out a number of therapeutic and preventive measures.
Fighting bleeding
The rich network of blood vessels in the maxillofacial region creates favorable conditions for bleeding to occur in facial injuries. Bleeding can occur not only outward or into the oral cavity, but also into the depths of the tissues (latent).
In case of bleeding from small vessels, the wound can be tamponed and a pressure bandage applied (if this does not cause a threat of asphyxia or displacement of jaw fragments). A pressure bandage can be used to stop bleeding in most injuries of the maxillofacial region. In cases of injury to large branches of the external carotid artery (lingual, facial, maxillary, superficial temporal), temporary bleeding can be stopped in emergency care using finger pressure.
Prevention of asphyxia and methods of combating it
First of all, it is necessary to correctly assess the patient's condition, paying attention to the nature of his breathing and position. In this case, asphyxia may be detected, the mechanism of which may be different:
- displacement of the tongue backwards (dislocation);
- closure of the lumen of the trachea by blood clots (obstructive);
- compression of the trachea by hematoma or edematous tissue (stenotic);
- closure of the entrance to the larynx with a hanging flap of soft tissue from the palate or tongue (valvular);
- aspiration of blood, vomit, soil, water, etc. (aspiration).
To prevent asphyxia, the patient should be seated, slightly bent forward and head down; in case of severe multiple injuries and loss of consciousness, lay on the back, turning the head towards the injury or to the side. If the injury allows, the patient can be laid face down.
The most common cause of asphyxia is tongue retraction, which occurs when the body of the lower jaw, especially the chin, is crushed in double mental fractures. One of the effective methods of combating this (dislocation) asphyxia is fixing the tongue with a silk ligature or piercing it with a safety pin or hairpin. To prevent obstructive asphyxia, it is necessary to carefully examine the oral cavity and remove blood clots, foreign bodies, mucus, food debris or vomit.
Anti-shock measures
The above measures should primarily include timely stopping of bleeding, elimination of asphyxia and implementation of transport immobilization.
The fight against shock in injuries to the maxillofacial region includes a whole range of measures carried out in cases of shock arising from injuries to other areas of the body.
To prevent further infection of the wound, it is necessary to apply an aseptic (protective) gauze bandage (for example, an individual package). It should be remembered that in case of facial bone fractures, the bandage should not be tightened too tightly to avoid displacement of the fragments, especially in case of fractures of the lower jaw.
Mid-level medical workers are prohibited from suturing soft tissue wounds in case of any facial injuries. In case of open wounds of the maxillofacial region, including all jaw fractures within the dental arch, it is mandatory at this stage of providing assistance to administer 3000 AE of Bezredko antitetanus serum.
For transport immobilization, fixing bandages are applied - a regular gauze bandage, a sling-like bandage, a circular bandage, a rigid chin bandage, or a standard transport bandage consisting of a chin bandage and a soft head cap.
If the doctor does not have these standard means, he can use a regular gauze (bandage) Hippocratic cap in combination with a sling-type gauze bandage; however, in cases where the patient is transported over a long distance to a specialized institution, it is more appropriate to apply a plaster sling-type bandage.
It is necessary to clearly fill out the referral to the medical institution, indicating everything that has been done to the patient, and to ensure the correct method of transportation.
If the patient's medical history indicates loss of consciousness, examination, assistance and transportation should be carried out only in the lying position.
The equipment of the first aid station must include everything necessary to provide first aid in case of facial injury, including feeding and quenching the thirst of the patient (a drinking cup, etc.).
In the case of a mass influx of victims (as a result of accidents, disasters, etc.), their correct evacuation and transport sorting (by a paramedic or nurse) is very important, i.e. establishing the order of evacuation and determining the position of the victims during transportation.
 [ 10 ]
[ 10 ]
First aid
First medical aid is provided by doctors of regional, district, rural district hospitals, central, district and city medical health centers, etc.
The main task in this case is to provide life-saving assistance: combat bleeding, asphyxia and shock, check and, if necessary, correct or replace previously applied bandages.
The fight against bleeding is carried out by ligating the vessels in the wound or by tightly tamponading it. In case of massive bleeding from the "oral cavity", which cannot be stopped by conventional means, the doctor must perform an urgent tracheotomy and tightly tamponade the oral cavity and pharynx.
If signs of suffocation appear, treatment measures are determined by the cause that caused it. In case of dislocation asphyxia, the tongue is sutured. A thorough examination of the oral cavity and removal of blood clots and foreign bodies eliminate the threat of obstructive asphyxia. If, despite the indicated measures, asphyxia still develops, an urgent tracheotomy is indicated.
Anti-shock measures are carried out according to the general rules of emergency surgery.
Then, in case of jaw fractures, it is necessary to apply a fixing bandage to perform transport (temporary) immobilization and give the patient something to drink in the usual way or using a drinking cup with a rubber tube attached to the spout.
Methods of temporary fixation of jaw fragments
Currently, the following methods of temporary (transport) immobilization of jaw fragments exist:
- chin slings;
- sling-like plaster or adhesive plaster bandage;
- intermaxillary ligation with wire or plastic thread;
- standard set and others. for example, continuous figure-eight ligature, lingual-labial ligature, Y. Galmosh ligature, continuous wire ligature according to Stout, Ridson, Obwegeser, Elenk, described quite well by Y. Galmosh (1975).
The choice of the method of temporary immobilization of fragments is determined by the location of the fractures, their number, the general condition of the victim and the presence of sufficiently stable teeth to fix the splint or bandage.
In case of a fracture of the alveolar process of the upper or lower jaw, after alignment of the fragments, an external gauze sling-like bandage is usually used, pressing the lower jaw to the upper.
For all fractures of the body of the upper jaw, after the fragments have been reduced, a metal splint-spoon of A. A. Limberg is placed on the upper jaw or a sling-like bandage is applied to the lower jaw.
If there are no teeth in the upper jaw, a lining of stens or wax is placed on the gums.
If the patient has dentures in his mouth, they are used as spacers between the dental arches and a sling-like bandage is additionally applied. In the anterior section of the plastic dental rows, a hole must be made with a cutter for the spout of a drinking cup, drainage tube or teaspoon to ensure the patient can eat.
If there are teeth on both jaws, then in case of fractures of the body of the lower jaw, the fragments are strengthened with an intermaxillary ligature bandage, a rigid standard sling or a plaster splint, which is placed on the lower jaw and attached to the cranial vault.
In case of fractures in the area of the condylar processes of the lower jaw, an intraoral ligature or rigid bandage with elastic traction to the victim's head cap is used. In cases of fractures of the condylar processes with malocclusion (open), the lower jaw is fixed with a spacer between the last antagonizing large molars. If there are no teeth on the damaged lower jaw, dentures can be used in combination with a rigid sling; if there are no dentures, a rigid sling or circular gauze bandage is used.
In case of combined fractures of the upper and lower jaws, the above-described methods of separate fixation of fragments are used, for example, the Rauer-Urbanskaya spoon splint in combination with ligature binding of the teeth at the ends of the lower jaw fragments. The ligature should cover two teeth on each fragment in the form of a figure eight. If there is no threat of intraoral bleeding, tongue retraction, vomiting, etc., a rigid sling can be used.
At the stage of providing first medical aid, it is necessary to correctly decide on the timing and method of transporting the victim, and, if possible, determine the evacuation purpose. In the presence of complicated and multiple fractures of the facial bones, it is advisable to reduce the number of "evacuation stages" to a minimum, sending such patients directly to inpatient maxillofacial departments of republican, regional and provincial (city) hospitals, hospitals.
In case of combined trauma (especially cranial trauma), the question of transporting the patient should be decided carefully, thoughtfully and together with the relevant specialists. In these cases, it is more appropriate to call specialists from regional or city institutions for consultation at the rural district hospital than to transport patients with concussion or brain contusion there.
If there is a dentist in the local hospital, first aid for conditions such as non-penetrating damage to the soft tissues of the face that do not require primary plastic surgery, tooth fractures, fractures of the alveolar processes of the upper and lower jaws, uncomplicated single fractures of the lower jaw without displacement, fractures of the nasal bones that do not require reduction, dislocations of the lower jaw that were successfully reduced, first- and second-degree facial burns, can be supplemented with elements of specialized care.
Patients with combined facial trauma, especially if there is a concussion, should be hospitalized in district hospitals. When deciding on their transportation in the first hours after the injury to specialized departments, the general condition of the patient, the type of transport, the road condition, and the distance to the medical facility should be taken into account. The most suitable type of transport for these patients can be considered a helicopter and, if the roads are in good condition, specialized ambulances.
After providing first aid in the district hospital, patients with fractures of the upper and lower jaws, multiple trauma to the facial bones complicated by trauma of any localization, penetrating and extensive damage to soft tissues requiring primary plastic surgery are sent to specialized departments of the district, city or regional hospital. The question of where the patient should be sent - to the district hospital (if there are dentists there) or to the maxillofacial department of the nearest hospital - is decided depending on local conditions.
Qualified surgical care
Qualified surgical care is provided by surgeons and traumatologists in outpatient clinics, trauma centers, surgical or trauma departments of city or district hospitals. It should be provided first of all to those victims who need it for vital indications. These include patients with signs of shock, bleeding, acute blood loss and asphyxia. For example, if, in the case of unstopped bleeding from large vessels of the maxillofacial region or bleeding that has occurred at previous stages, it is not possible to reliably ligate the bleeding vessel, then the external carotid artery on the corresponding side is ligated. At this stage of care, all victims with injuries to the maxillofacial region are divided into three groups.
The first group - those who require only surgical assistance (soft tissue injuries without true defects, first- and second-degree burns, facial frostbite); for them, this stage of treatment is the final one.
The second group - those requiring specialized treatment (soft tissue injuries requiring plastic surgery; damage to facial bones; third- and fourth-degree burns and frostbite of the face requiring surgical treatment); after emergency surgical care, they are transported to maxillofacial hospitals.
The third group includes non-transportable victims, as well as individuals with combined injuries to other areas of the body (especially traumatic brain injury), which are leading in terms of severity.
One of the reasons for repeated surgical treatment of a wound is intervention without preliminary X-ray examination. If there is a suspicion of facial bone fractures, it is mandatory. The increased regenerative capacity of facial tissues allows for surgical intervention to be performed with maximum tissue sparing.
When providing qualified surgical care to victims of group II who will be sent to specialized medical institutions (in the absence of contraindications for transportation), the surgeon must:
- to perform prolonged anesthesia of the fracture site; or even better - prolonged anesthesia of the entire half of the face, either using the method of P. Yu. Stolyarenko (1987): through a needle injection under the bone ledge on the lower edge of the zygomatic arch at the junction of the temporal process of the zygomatic bone with the zygomatic process of the temporal bone;
- inject the wound with antibiotics, administer antibiotics internally;
- perform the simplest transport immobilization, for example, apply a standard transport bandage;
- make sure that there is no bleeding from the wound, asphyxia or threat of asphyxia during transportation;
- monitor the administration of antitetanus serum;
- ensure proper transportation to a specialized medical facility accompanied by medical personnel (determine the type of transport, the patient’s position);
- clearly indicate in the accompanying documents everything that was done to the patient.
In cases where there are contraindications to sending the victim to another medical institution (Group III), he is provided with qualified assistance in the surgical department with the involvement of dentists from hospitals or clinics, who are obliged
General surgeons and traumatologists, in turn, must be familiar with the basics of providing assistance in case of trauma to the maxillofacial region, adhere to the principles of surgical treatment of facial wounds, and know the basic methods of transport immobilization of fractures.
Treatment of victims with combined wounds to the face and other areas in a surgical (traumatology) hospital should take place with the participation of a maxillofacial surgeon.
If a district hospital has a maxillofacial department or a dental office, the head of the department (dentist) must be responsible for the state and organization of traumatological dental care in the district. For the correct recording of maxillofacial trauma, the dentist must establish contact with the feldsher stations and district hospitals. In addition, an analysis of the treatment results of patients with facial trauma who were in district and regional institutions should be conducted.
Patients with complex and complicated facial injuries are referred to the maxillofacial department if primary soft tissue plastic surgery is required and the latest methods of treating facial bone fractures, including primary bone grafting, are used.
Specialized emergency care and follow-up treatment for maxillary fracture
This type of care is provided in inpatient maxillofacial departments of republican, regional, provincial, city hospitals, in surgical dentistry clinics of medical universities, research institutes of dentistry, in maxillofacial departments of research institutes of traumatology and orthopedics.
When victims are admitted to the hospital admission department, it is advisable to identify three sorting groups (according to V.I. Lukyanenko):
The first group - those requiring urgent measures, qualified or specialized care in the dressing room or operating room: those wounded in the face with ongoing bleeding from under bandages or the oral cavity; those in a state of asphyxia or with unstable external respiration, after tracheotomy with tight tamponade of the oral cavity and pharynx, those in an unconscious state. They are sent to the operating room or dressing room on a stretcher first.
The second group - those requiring clarification of the diagnosis and determination of the leading severity of the injury. These include wounded with combined injuries to the jaws and face, ENT organs, skull, organs of vision, etc.
The third group - those subject to referral to the department in the second priority. This group includes all victims who were not included in the first two groups.
Before the start of surgical treatment, the victim must be examined clinically and radiologically. Based on the data obtained, the scope of the intervention is determined.
Surgical treatment, regardless of whether it is early, delayed or late, should be immediate and, if possible, complete, including local plastic surgery on soft tissues and even bone grafting of the lower jaw.
As A. A. Skager and T. M. Lurye (1982) point out, the nature of the regenerative blastema (osteogenic, chondrogenic, fibrous, mixed) is determined by the oxybiotic activity of the tissues in the fracture zone, in connection with which all traumatic and therapeutic factors affect the speed and quality of reparative osteogenesis mainly through local blood supply. As a result of injury, there are always circulatory disorders of a local (wound and fracture area), regional (maxillofacial area) or general (traumatic shock) nature. Local and regional circulatory disorders are usually more prolonged, especially in the absence of immobilization of fragments and the occurrence of inflammatory complications. As a result, the reparative reaction of tissues is distorted.
With adequate blood supply to the damaged area, under conditions of fragment stability, primary, so-called angiogenic bone tissue formation occurs. Under less favorable vascular-regenerative conditions, which are created mainly in the absence of stability in the area of fragment junction, connective tissue, or cartilaginous, regenerate is formed, i.e. "reparative osteosynthesis" occurs, especially in the absence of timely and correct alignment of fragments. This course of reparative regeneration requires more tissue resources and time. It can end with secondary bone fusion of the fracture, but in this case, cicatricial connective tissue with foci of chronic inflammation sometimes persists for a long time or remains forever in the fracture area, which can clinically manifest itself in the form of exacerbation of traumatic osteomyelitis.
From the point of view of optimizing the vascular-regenerative complex, closed reposition and fixation of facial bone fragments have an advantage over open osteosynthesis with wide exposure of the ends of the fragments.
Therefore, the following principles form the basis of modern treatment of bone fractures:
- perfectly accurate comparison of fragments;
- bringing the fragments along the entire fracture surface into a position of tight contact (knocked together);
- strong fixation of the repositioned fragments and their contact surfaces, eliminating or almost eliminating any visible mobility between them during the entire period necessary for complete healing of the fracture;
- maintaining the mobility of the temporomandibular joints if the surgeon has a device for extraoral repositioning and fixation of fragments of the lower jaw.
This ensures faster fusion of bone fragments. Compliance with these principles ensures primary fusion of the fracture and allows for shorter treatment periods for patients.
Additional general and local treatment measures for fresh fractures complicated by inflammation
Specialized care for maxillofacial injuries involves a range of measures aimed at preventing complications and accelerating bone tissue regeneration (physiotherapeutic treatments, exercise therapy, vitamin therapy, etc.). All patients should also be provided with the necessary nutrition and proper oral care. In large departments, it is recommended to allocate special wards for trauma patients.
In all types of assistance, it is necessary to fill out medical documentation clearly and correctly.
Measures to prevent complications include the administration of antitetanus serum, local administration of antibiotics in the preoperative period, oral cavity sanitation, temporary immobilization of fragments (to the extent possible). It is important to remember that infection in fractures within the dental arch can occur not only with a rupture of the mucous membrane or damage to the skin, but also in the presence of periapical inflammatory foci of teeth located in the fracture area or in close proximity to it.
If necessary, in addition to applying a standard transport bandage, intermaxillary fixation is performed using ligature tying of the teeth.
The method of anesthesia is selected depending on the situation and the number of patients admitted. In addition to the general condition of the patient, it is necessary to consider the location and nature of the fracture, as well as the time expected to be spent on orthopedic fixation or osteosynthesis. In most cases of fractures of the body and branch of the jaw (except for high fractures of the condylar process, accompanied by dislocation of the head of the lower jaw), local conduction and infiltration anesthesia can be used. Conduction anesthesia is best performed in the area of the oval opening (if necessary on both sides) to turn off not only the sensory but also the motor branches of the mandibular nerve. Potentiated local anesthesia is more effective. Extended conduction block and its combination with the use of calypsol in subnarcotic doses are also used.
To decide what to do with a tooth located directly in the fracture gap, it is necessary to determine the relationship of its roots to the fracture plane. Three positions are possible:
- the fracture gap runs along the entire lateral surface of the tooth root - from its neck to the opening of the apex;
- the apex of the tooth is located in the fracture gap;
- The fracture gap passes obliquely in relation to the vertical axis of the tooth, but outside its alveolus, without damaging the periodontium and the walls of the tooth alveolus.
The third position of the tooth is the most favorable in terms of consolidation prognosis (without the development of a clinically noticeable inflammatory complication), and the first position is the least favorable, since in this case there is a rupture of the mucous membrane of the gum at the neck of the tooth and a gaping fracture gap, causing inevitable infection of the jaw fragments with pathogenic microflora of the oral cavity. Therefore, even before immobilization, it is necessary to remove teeth in the first position, as well as broken, dislocated, crushed, destroyed by caries, complicated by pulpitis or chronic periodontitis. After tooth extraction, it is recommended to isolate the fracture zone by tamponing the socket with iodoform gauze. N. M. Gordiyuk et al. (1990) recommend tamponing the sockets with preserved (in a 2% chloramine solution) amnion.
It is very important to determine the nature of the microflora in the fracture area and examine its sensitivity to antibiotics. Intact teeth in the second and third positions can be conditionally left in the fracture gap, but in this case, complex treatment should include antibiotic and physiotherapy. If, during such treatment, the first clinical signs of inflammation in the fracture area appear, the remaining tooth is treated conservatively, its root canals are filled, and if they are obstructed, they are removed.
Tooth rudiments, teeth with unformed roots and not yet erupted teeth (in particular, third molars) in the absence of inflammation around them can also be conditionally left in the fracture area, because, as our experience and observations of other authors show, the well-being in the area of teeth left in the fracture gap, clinically determined on the day of the patient's discharge from the hospital, is often deceptive, unstable, especially in the first 3-9 months after the injury. This is explained by the fact that sometimes the pulp of two-rooted teeth located in the fracture area, accompanied by damage to the mandibular vascular-nerve bundle, undergoes deep inflammatory-dystrophic changes ending in necrosis. When the vascular-nerve bundle of a single-rooted tooth is damaged, necrotic changes in the pulp are observed in most cases.
According to data from various authors, preservation of teeth in the fracture gap is possible only in 46.3% of patients, since the rest develop periodontitis, bone resorption, osteomyelitis. At the same time, tooth rudiments and teeth with incompletely formed roots, preserved provided there are no signs of inflammation, have high viability: after reliable immobilization of fragments, teeth continue to develop normally (in 97%) and erupt in a timely manner, and the electrical excitability of their pulp is normalized in the long term. Teeth replanted in the fracture gap die on average in half of patients.
If, in addition to damage to the maxillofacial area, there is a concussion or brain injury, dysfunction of the circulatory system, respiratory and digestive systems, etc., the necessary measures are taken and appropriate treatment is prescribed. Often it is necessary to resort to consultations with various specialists.
Due to the anatomical connection of the bones of the cranium and face, all structures of the cranial part of the skull suffer in case of trauma to the maxillofacial region. The force of the acting factor in its intensity usually exceeds the limit of elasticity and strength of individual facial bones. In such cases, adjacent and deeper parts of the facial and even cranial part of the skull are damaged.
A feature of combined facial and brain trauma is that brain damage can occur even without a blow to the brain part of the skull. The traumatic force that caused a facial bone fracture is transmitted directly to the adjacent brain, causing neurodynamic, pathophysiological and structural changes of varying degrees. Therefore, combined damage to the maxillofacial region and the brain can be caused by the impact of a traumatic agent only on the facial part of the skull or on the facial and brain parts of the skull simultaneously.
Clinically, closed craniocerebral injury manifests itself with general cerebral and local symptoms. General cerebral symptoms include loss of consciousness, headache, dizziness, nausea, vomiting, amnesia, and local symptoms include dysfunction of the cranial nerves. All patients with a history of concussion require complex treatment with a neurosurgeon or neurologist. Unfortunately, concussion combined with facial bone trauma is usually diagnosed only in cases with pronounced neurological symptoms.
Complications of jaw fracture, prevention and treatment
All complications arising from jaw fractures can be divided into general and local, inflammatory and non-inflammatory; by time they are divided into early and remote (late).
Common early complications include disturbances of psycho-emotional and neurological status, changes in the circulatory system and other systems. Prevention and treatment of these complications are carried out by maxillofacial surgeons together with relevant specialists.
Among local early complications, the most frequently observed are dysfunction of the masticatory apparatus (including the temporomandibular joints), traumatic osteomyelitis (in 11.7% of victims), suppuration of hematomas, lymphadenitis, arthritis, abscesses, phlegmon, sinusitis, delayed consolidation of fragments, etc.
To prevent possible general and local complications, it is advisable to carry out novocaine trigemino-sympathetic and carotid sinus blockades, which allow turning off extracerebral reflexogenic zones, due to which cerebrospinal fluid dynamics, respiration, and cerebral circulation are normalized.
Trigemino-sympathetic block is performed according to the well-known method of M. P. Zhakov. Carotid sinus block is performed as follows: a bolster is placed under the back of the victim lying on his back, at the level of the shoulder blades, so that the head is slightly thrown back and turned in the opposite direction. A needle is injected along the inner edge of the sternocleidomastoid muscle, 1 cm below the level of the upper edge of the thyroid cartilage (projection of the carotid sinus). As the needle advances, novocaine is injected. When the fascia of the vascular-nerve bundle is punctured, a certain resistance is overcome and pulsation of the carotid sinuses is felt. 15-20 ml of 0.5% novocaine solution is injected.
Given the increased risk of developing septic complications in patients with damage to the maxillofacial region, brain and other areas of the body, it is necessary to prescribe massive doses of antibiotics (after an intradermal test for individual tolerance) already in the first day after admission to the hospital.
If complications from the respiratory system occur (which are often the cause of death in such patients), hormone therapy and dynamic X-ray observation (with the involvement of appropriate specialists) are indicated. Specialized care for such patients should be provided by a maxillofacial surgeon immediately after the victims are brought out of shock, but no later than 24-36 hours after the injury.
Various local and general adverse factors (infection of the oral cavity and decayed teeth, crushing of soft tissues, hematoma, insufficiently rigid fixation, exhaustion of the patient due to disruption of normal nutrition, psycho-emotional stress, dysfunction of the nervous system, etc.) contribute to the occurrence of inflammatory processes. Therefore, one of the main points of the treatment of the victim is stimulation of the healing process of the jaw fracture by increasing the regenerative abilities of the patient's body and preventing inflammatory layers in the area of damage.
In recent years, due to the increased resistance of staphylococcal infection to antibiotics, the number of inflammatory complications in facial bone injuries has increased. The greatest number of complications in the form of inflammatory processes occur in fractures localized in the area of the angle of the lower jaw. This is explained by the fact that the masticatory muscles located on both sides of the fracture area reflexively contract, penetrate the gap and are pinched between the fragments. As a result of the fact that the mucous membrane of the gum in the area of the angle of the lower jaw is tightly fused with the periosteum of the alveolar process and ruptures at the slightest displacement of the fragments, constantly gaping entry gates for infection are formed, through which pathogenic microorganisms, saliva, exfoliated epithelial cells and food masses enter the bone gap. During swallowing movements, muscle fibers pinched by fragments contract, as a result of which there is an active flow of saliva into the depth of the bone gap.
Evidence of increasing inflammation of the bone and soft tissues is usually the rapidly developing hyperemia of the skin, pain, infiltration, etc.
The development of complications is facilitated by such factors as periodontitis (in 14.4% of victims), delayed hospitalization and untimely provision of specialized care, advanced age of patients, the presence of chronic concomitant diseases, bad habits (alcoholism), decreased reactivity of the body, incorrect diagnosis and choice of treatment method, dysfunction of the peripheral nervous system resulting from a fracture (damage to the branches of the trigeminal nerve), etc.
A significant factor that delays the consolidation of jaw fragments is traumatic osteomyelitis, which, along with other inflammatory processes, occurs especially often in cases where repositioning and immobilization of fragments was carried out at a later stage.
It is necessary to take into account that any injury causes an inflammatory reaction around the wound. Regardless of the type of damaging agent (physical, chemical, biological), the pathogenetic mechanisms of the developing inflammatory process are the same and are characterized by a violation of the state of microcirculation, oxidation-reduction processes and the action of microorganisms in damaged tissues. In case of injuries, bacterial contamination of the wound is inevitable. The severity of the purulent-inflammatory process depends on the characteristics of the infectious agent, the immunobiological state of the patient's body at the time of introduction of the pathogen, the degree of vascular and metabolic disorders of the tissues at the site of injury. The resistance of damaged tissues to purulent infection is sharply reduced, conditions are created for the reproduction of the pathogen and the manifestation of its pathogenic properties, causing an inflammatory reaction and having a destructive effect on the tissues.
At the site of action of the damaging factor, optimal conditions are created for the activation of proteolytic enzymes released from microorganisms, affected tissues, leukocytes, and the formation of inflammation-stimulating mediators - histamine, serotonin, kinins, heparin, activated proteins, etc., which cause disruption of microcirculation, transcapillary exchange, blood coagulation. Tissue proteases, products of microbial activity, contribute to the disorder of oxidation-reduction processes, the separation of tissue respiration.
The resulting accumulation of under-oxidized products and the development of tissue acidosis leads to secondary disorders of microhemodynamics at the site of injury and the development of local vitamin deficiency.
Particularly severe damage to tissue regeneration processes is observed when vitamin C deficiency occurs in them, leading to inhibition of connective tissue collagen synthesis and wound healing; in this case, the vitamin C content is significantly reduced in the flaccid granulations of infected wounds.
In any injury, a significant role in limiting the inflammatory process is given to the hemostatic reaction, since the formation of a fibrin layer and the deposition of toxic substances and microorganisms on its surface prevents the further spread of the pathological process.
Thus, with purulent complications of injuries, a closed chain of pathological processes occurs that promote the spread of infection and prevent wound healing. Therefore, the early use of various biologically active drugs with anti-inflammatory, antimicrobial, antihypoxic and reparative process stimulating effects is pathogenetically justified in order to reduce purulent complications and increase the effectiveness of complex treatment.
The Kiev Research Institute of Orthopedics of the Ministry of Health of Ukraine conducted research on the mechanism of action of biologically active substances and recommended amben, galascorbin, Kalanchoe, and propolis for use in purulent-inflammatory diseases.
Unlike natural inhibitors of proteolysis (trasylol, contrycal, iniprole, tsalol, gordox, pantrypin), amben easily penetrates all cell membranes and can be used locally as a 1% solution, intravenously or intramuscularly at 250-500 mg every 6-8 hours. Within 24 hours, the drug is excreted unchanged by the kidneys. When applied locally, it penetrates well into tissues and completely neutralizes tissue fibrinolysis of damaged tissues within 10-15 minutes.
In purulent-inflammatory complications of jaw fractures, amoxiclav is successfully used - a combination of clavulanic acid with amoxicillin, which is administered intravenously at 1.2 g every 8 hours or orally at 375 mg 3 times a day for 5 days. For patients who have undergone elective surgery, the drug is prescribed intravenously at 1.2 g once a day or orally in the same doses.
The biological activity of galascorbin significantly exceeds the activity of ascorbic acid due to the presence of ascorbic acid in the preparation in combination with substances with P-vitamin activity (polyphenols). Galascorbin promotes the accumulation of ascorbic acid in organs and tissues, thickens the vascular wall, stimulates wound healing processes, accelerates the regeneration of muscle and bone tissue, and normalizes oxidation-reduction processes. Galascorbin is used orally at 1 g 4 times a day; locally - in 1-5% freshly prepared solutions or in the form of a 5-10% ointment.
Propolis contains 50-55% of plant resins, 30% of wax and 10-18% of essential oils; it includes various balms, it contains cinnamic acid and alcohol, tannins; it is rich in microelements (copper, iron, manganese, zinc, cobalt, etc.), antibiotic substances and vitamins of groups B, E, C, PP, P and provitamin A; it has an analgesic effect. Its antibacterial effect is most pronounced. Antimicrobial properties of propolis have been established in relation to a number of pathogenic gram-positive and gram-negative microorganisms, while its ability to increase the sensitivity of microorganisms to antibiotics, change the morphological, cultural and tinctorial properties of various strains has been noted. Under the influence of propolis, wounds are quickly cleared of purulent and necrotic cover. It is used in the form of an ointment (33 g of propolis and 67 g of lanolin) or sublingually - in the form of tablets (0.01 g) 3 times a day.
Other measures are also recommended to prevent inflammatory complications and stimulate osteogenesis. Some of them are listed below:
- Administration of antibiotics (taking into account the sensitivity of microflora) into soft tissues surrounding the open fracture area, starting from the first day of treatment. Local administration of antibiotics allows to reduce the number of complications by more than 5 times. When antibiotics are administered at a later stage (on the 6th-9th day and later), the number of complications does not decrease, but the elimination of already developed inflammation is accelerated.
- Intramuscular administration of antibiotics if indicated (increasing infiltrate, increased body temperature, etc.).
- Local UHF therapy from the 2nd to the 12th day from the moment of injury (10-12 minutes daily), general quartz irradiation from the 2nd-3rd day (about 20 procedures), calcium chloride electrophoresis on the fracture area - from the 13th-14th day until the end of treatment (up to 15-20 procedures).
- Oral administration of multivitamins and 5% calcium chloride solution (one tablespoon three times a day with milk); ascorbic acid and thiamine are especially useful.
- In order to accelerate the consolidation of fragments, O. D. Nemsadze (1991) recommends additional use of the following medications: anabolic steroid (for example, nerobol per os, 1 tablet 3 times a day for 1-2 months, or retabolil 50 mg intramuscularly once a week for 1 month); sodium fluoride 1% solution, 10 drops 3 times a day for 2-3 months; protein hydrolysate (hydrolysine, casein hydrolysate) for 10-20 days.
- In order to reduce the spasm of blood vessels in the fracture zone (which, according to A. I. Elyashev (1939), lasts 1-1.5 months and inhibits bone formation), as well as to accelerate the consolidation of fragments, O. D. Nemsadze (1985) suggests intramuscular administration of antispasmodic drugs (gangleron, dibazol, papaverine, trental, etc.) 3 days after the injury for 10-30 days.
- Intramuscular administration of lysozyme 100-150 mg twice a day for 5-7 days.
- Use of a complex of antioxidants (tocopherol acetate, flacumin, ascorbic acid, cysteine, eleutherococcus extract or acemine.
- Application of local hypothermia according to the technique described by A. S. Komok (1991), provided that a special device for local hypothermia in the maxillofacial area is used; allows for maintaining the temperature regime of injured tissues, including the lower jaw bone, in the range of +30°C - +28°C; due to balanced tissue cooling using the external and intraoral chambers, the temperature of the circulating coolant can be reduced to +16°C, which makes the procedure well tolerated and allows it to be continued for a long time. A. S. Komok indicates that reducing the local tissue temperature in the fracture zone of the lower jaw to the levels of: on the skin +28°C, the mucous membrane of the cheek +29°C and the mucous membrane of the alveolar process of the lower jaw +29.5°C - helps to normalize blood flow, eliminate venous congestion, swelling, prevents the development of hemorrhages and hematomas, and eliminates pain reactions. Layered, uniform, moderate tissue hypothermia in a cooling mode of +30°C - +28°C for the next 10-12 hours after double-jaw immobilization in combination with medications allows for normalization of blood flow in tissues by the third day, elimination of temperature reactions and inflammatory phenomena, and causes a pronounced analgesic effect.
At the same time, A. S. Komok also emphasizes the complexity of this method, since, according to his data, only a complex of electrophysiological methods, including electrothermometry, rheography, rheodermatometry and electroalgesimetry, allows for a fairly objective assessment of blood flow, heat exchange and innervation in injured tissues and the dynamics of changes in these indicators under the influence of the treatment.
According to V. P. Korobov et al. (1989), correction of metabolic shifts in the blood in fractures of the lower jaw can be achieved either by ferramid or (which is even more effective) by coamide, which promotes accelerated fusion of bone fragments. In the case of acute traumatic osteomyelitis, the abscess is opened and the fracture gap is washed; fractional autohemotherapy is also desirable - reinfusion of blood irradiated with ultraviolet rays 3-5 times along with active anti-inflammatory antiseptic therapy according to the generally accepted scheme; In the chronic inflammation stage, it is recommended to activate bone regeneration according to the following scheme: levamisole (150 mg orally once a day for 3 days; a break between cycles is 3-4 days; there are 3 such cycles), or T-activin subcutaneously (0.01%, 1 ml for 5 days), or exposure to a helium-neon laser on biologically active points of the face and neck (10-15 s per point with a light flux power of no more than 4 mW for 10 days). After the onset of stiffness in the fracture zone, dosed mechanotherapy and other general biological effects were prescribed. According to the authors, the duration of inpatient treatment is reduced by 10-12 days, and temporary disability - by 7-8 days.
Many other means and methods have been proposed for the prevention or treatment of traumatic osteomyelitis of the jaws, such as a suspension of demineralized bone, Nitazol aerosol, staphylococcal anatoxin with autologous blood, vacuum aspiration of the fracture gap contents and rinsing the bone wound under pressure with a stream of 1% dioxidine solution; immunocorrective therapy. E. A. Karasyunok (1992) reports that he and his co-workers have experimentally studied and clinically proven the advisability of using, against the background of rational antibiotic therapy, a 25% solution of acemine orally at 20 ml 2 times a day for 10-14 days, as well as sounding the fracture area with the UPSK-7N device in a continuous labile mode, and the introduction of a 10% solution of lincomycin hydrochloride by electrophoresis. The use of this technique resulted in a reduction in complications from 28% to 3.85% and a reduction in temporary disability by 10.4 days.
R. 3. Ogonovsky, I. M. Got, O. M. Sirii, I. Ya. Lomnitsky (1997) recommend using cellular xeno-brephotransplantation in the treatment of long-term non-healing jaw fractures. For this purpose, a suspension of devitalized bone marrow cells of 14-day embryos is introduced into the fracture gap. On the 12-14th day, the authors observed thickening of the periosteal bone callus, and on the 20-22nd day, the onset of stable consolidation of the fracture, which had not healed during 60 days of immobilization. The method allows one to get rid of repeated surgical interventions.
Domestic and foreign literature abounds with other proposals, which, unfortunately, are currently only available to doctors working in clinics well equipped with the necessary equipment and medications. But every doctor should remember that there are other, more accessible means of preventing complications in the treatment of facial bone fractures. For example, one should not forget that such a simple procedure as calcium chloride electrophoresis (introduction of a 40% solution from the anode at a current of 3 to 4 mA) promotes rapid compaction of the forming bone callus. In case of fracture complication by inflammation, in addition to antibiotic therapy, it is advisable to use an alcohol-novocaine blockade (0.5% novocaine solution in 5% alcohol). Complex treatment according to the described scheme allows to reduce the time of fragment immobilization by 8-10 days, and in case of fractures complicated by the inflammatory process - by 6-8 days.
We observed a significant reduction in the hospitalization period when introducing 0.2 ml of osteogenic cytotoxic serum (stimoblast) in isotonic sodium chloride solution (dilution 1:3) into the fracture area. The serum was administered on the 3rd, 7th, and 11th day after the injury.
Some authors recommend including microwave and UHF therapy in combination with general ultraviolet irradiation and calcium chloride electrophoresis in complex treatment to accelerate the consolidation of jaw fragments, and V.P. Pyurik (1993) recommends using interfragment injection of the patient's bone marrow cells (at a rate of 1 mm3 of cells per 1 cm2 of bone fracture surface).
Based on the mechanism of development of inflammatory complications of fractures in the area of the angles of the lower jaw, their prevention requires the earliest possible immobilization of bone fragments in combination with targeted anti-inflammatory drug therapy. In particular, after treating the oral cavity with a furacilin solution (1:5000), infiltration anesthesia should be performed in the fracture area with a 1% solution of novocaine (from the skin side) and, after making sure that the needle is in the fracture gap (blood gets into the syringe and the anesthetic gets into the mouth), repeatedly wash out (with a furacilin solution) the contents from the gap into the oral cavity through the damaged mucous membrane (L. M. Vartanyan).
Before immobilizing the jaw fragments using rigid intermaxillary fastening (traction) or the least traumatic (percutaneous) osteosynthesis method with a Kirschner wire, it is recommended to infiltrate the soft tissues in the area of the mandibular angle fracture with a broad-spectrum antibiotic solution. Inflicting more significant trauma (for example, exposing the angle of the jaw and applying a bone suture) is undesirable, as it contributes to the intensification of the inflammatory process that has begun.
In the presence of developed traumatic osteomyelitis, after sequestrectomy, the fracture can be fixed with a metal pin inserted transfocally (through the fracture gap), but more effective is fixation of the lower jaw fragments with external extrafocal compression devices, which, in fractures complicated by traumatic osteomyelitis (in the acute stage of the course), ensure consolidation within the usual time frame (not exceeding the healing of fresh fractures) and help stop the inflammatory process due to the fact that compression is carried out without preliminary intervention in the lesion. Extrafocal fixation of fragments allows for the necessary surgical intervention in the future (opening an abscess, phlegmon, removing sequesters, etc.) without violating immobilization.
Traumatic osteomyelitis almost always has a sluggish course, does not significantly affect the general condition of the patient. Long-term swelling of soft tissues in the fracture zone is associated with congestion, periosteal reaction, and lymph node infiltration. Rejection of bone sequesters from the fracture gap occurs slowly; their size is usually insignificant (several millimeters). Periodically, exacerbations of osteomyelitis, periostitis, and lymphadenitis are possible with the formation of perimandibular abscesses, phlegmon, and adenophlegmon. In these cases, it is necessary to dissect the tissues to evacuate pus, drain the wound, and prescribe antibiotics.
In the chronic stage of osteomyelitis, it is advisable to use compression rapprochement of jaw fragments, or prescribe pentoxyl 0.2-0.3 g 3 times a day for 10-14 days (both after dental splinting and after percutaneous osteosynthesis), or inject (through a Dufour needle) 2-3 ml of a suspension of lyophilized fetal allobone powder into the fracture gap. It is recommended to inject the suspension once, under local anesthesia, 2-3 days after repositioning and fixation of the fragments, i.e. when the healed wound on the gum prevents the suspension from leaking into the oral cavity. Thanks to this tactic, intermaxillary traction can be removed, both in single and double fractures, 6-7 days earlier than usual, reducing the total duration of disability by an average of 7-8 days. Extraoral injection of 5-10 ml of 10% alcohol solution in 0.5% novocaine solution into the fracture area also accelerates clinical consolidation of fragments by 5-6 days and reduces the duration of disability by an average of 6 days. The use of allocosteum and pentoxyl allows to significantly reduce the number of inflammatory complications.
There is data on the effectiveness of using various other methods and means to stimulate osteogenesis (in the area of traumatic osteomyelitis): focal dosed vacuum, ultrasound exposure, magnetic therapy according to N.A. Berezovskaya (1985), electrical stimulation; low-intensity radiation of a helium-neon laser taking into account the stage of the post-traumatic process; local oxygen therapy and three-, four-fold X-ray irradiation in doses of 0.3-0.4 fairy (with pronounced signs of acute inflammation, when it is necessary to relieve swelling and infiltration or accelerate abscess formation, relieve pain symptoms and create favorable conditions for wound healing); thyrocalcitonin, ectericide in combination with ascorbic acid, nerobol in combination with protein hydrolysate, phosphrene, gemostimulin, fluoride preparations, osteogenic cytotoxic serum, carbostimulin, retabolil, eleutherococcus; inclusion of "Ocean" paste from krill, etc. in the patient's diet. At the stage of chronic traumatic osteomyelitis after necrectomy, some authors use radiotherapy at a dose of 0.5-0.7 gray (5-7 irradiations) to eliminate local signs of exacerbation of the inflammatory process, accelerate wound cleansing from necrotic masses, improve sleep, appetite and general well-being of patients. Good results in traumatic osteomyelitis of the lower jaw are obtained in the case of a combination of sequestrectomy with radical treatment of the bone wound, filling the bone defect with brefobone and rigid immobilization of jaw fragments.
When a fracture is combined with periodontitis, inflammatory phenomena in the soft tissues of the fracture area are especially pronounced. Such patients admitted on the 3rd-4th day have pronounced gingivitis, bleeding gums, foul odor from the mouth, and pus discharge from pathological pockets. Consolidation of the fracture in periodontitis is longer. In such cases, it is recommended to conduct complex treatment of periodontitis along with fracture treatment.
Physical therapy is of great importance in the treatment of lower jaw fractures. Active exercises for the masticatory muscles (with minimal range of motion), facial muscles, and tongue can be started 1-2 days after immobilization with a single-jaw dental splint or bone extraoral device. With intermaxillary traction, general tonic exercises, exercises for the facial muscles and tongue, and exercises for volitional tension for the masticatory muscles can be used from the 2nd-3rd day after the fracture (splinting) until the removal of the rubber traction. After the primary consolidation of the fracture and removal of the intermaxillary rubber traction, active exercises for the lower jaw are prescribed.
Impaired blood flow in the area of the masticatory muscles leads to a decrease in the intensity of regenerate mineralization in the angular fracture gap (V. I. Vlasova, I. A. Lukyanchikova), which is also the cause of frequent inflammatory complications. Timely prescribed physical activity regimen (therapeutic exercise) significantly improves electromyographic, gnathodynometric and dynamometric indices of masticatory muscle function. Early functional loading of the alveolar processes using gingival splints-prostheses used for fractures within the dental arch (in the presence of one edentulous fragment that can be manually reduced and held by the base of the splint-prosthesis, as well as in cases of rigidly stable immobilization using osteosynthesis) also helps to reduce the period of incapacity for work by an average of 4-5 days. When functional chewing loads are included in the complex of therapeutic measures, the regenerate undergoes restructuring more quickly, restores its histological structure and function, while maintaining its anatomical shape.
To reduce the degree of hypodynamic disorders in the masticatory muscles and in the area of the lower jaw fracture, it is possible to use the method of bioelectric stimulation (common in general traumatology, sports and space medicine) of the temporoparietal and masticatory muscles using the Myoton-2 device. The procedures are carried out daily for 5-7 minutes for 15-20 days, starting from the 1st to 3rd day after immobilization. Electrical stimulation leads to the contraction of the specified muscles without the occurrence of movements in the temporomandibular joints; due to this, blood circulation and neuroreflex connections in the maxillofacial area are restored faster, muscle tone is preserved. All this also helps to reduce the period of fracture consolidation.
According to V. I. Chirkin (1991), the inclusion of multichannel biocontrolled proportional electrical stimulation of the temporal, masticatory muscles and muscles that lower the lower jaw in the usual complex of rehabilitation measures in subthreshold and therapeutic mode in patients with unilateral trauma allowed by the 28th day to completely restore the blood supply to the tissues, increase the volume of mouth opening to 84%, and the amplitude of the M-response to 74% compared to the norm. It was possible to normalize the chewing function, and patients spent as much time and used the same number of chewing movements to chew food samples as healthy individuals.
In patients with bilateral surgical trauma of the masticatory muscles, procedures of multichannel biocontrolled proportional electrical stimulation in subthreshold, therapeutic and training modes can be started from an early stage (7-9 days after surgery), which ensures positive changes in the blood supply to the injury zone, as evidenced by the results of rheographic studies, which reached the norm by the time the splints were removed.
It was possible to increase the volume of mouth opening to 74%, the amplitude of the M-response also increased to 68%. The chewing function almost normalized, according to functional electromyography, the indicators of which reached the level of average indicators of healthy individuals. The author believes that the method of multichannel rheovasofaciography, stimulation electromyography of the masticatory muscles, registration of the periodontomuscular reflex and the method of multichannel functional electromyography with standard food samples are the most objective in studying the masticatory system and can be the methods of choice in examining patients with both jaw fractures and surgical (operational) trauma of the masticatory muscles.
Procedures of multichannel biocontrolled proportional electrical stimulation of masticatory muscles in three modes according to the method recommended by the author allow to start functional rehabilitation treatment from an early stage. This type of treatment best corresponds to the natural function of the masticatory system, is well dosed and controlled, which provides the highest results of restoration of function to date and allows to reduce the total time of incapacity of patients by 5-10 days.
The problem of treatment and rehabilitation of patients with fractures of the lower jaw, accompanied by damage to the inferior alveolar nerve, deserves special consideration. According to S. N. Fedotov (1993), damage to the inferior alveolar nerve was diagnosed in 82.2% of victims with a fracture of the lower jaw, of which 28.3% were mild, 22% were moderate, and 31.2% were severe. Mild injuries include those in which the reaction of all teeth on the side of the fracture was within 40-50 μA, and mild hypesthesia was observed in the area of the skin of the chin and the mucous membrane of the oral cavity; the moderate category includes a reaction of teeth up to 100 μA. With a reaction over 100 μA and partial or complete loss of sensitivity of soft tissues, the damage is considered severe. At the same time, neurological disorders in facial bone fractures and their treatment in practical medicine have not received enough attention to date. The depth of nerve damage, according to S. N. Fedorov, increases even more with surgical methods of joining fragments. As a result, long-term sensory disorders, neurotrophic destructive processes in bone tissue, slowing of fragment fusion, decreased chewing function and excruciating pain develop.
Based on his clinical observations (336 patients), the author developed a rational complex of restorative treatment of mandibular fractures accompanied by damage to the third branch of the trigeminal nerve, using physical methods and medicinal stimulating drugs (neurotropic and vasodilators). To prevent secondary damage to the inferior alveolar nerve and its branches during surgical treatment of fractures, a new version of osteosynthesis of fragments with metal spokes is proposed, based on a gentle attitude to the teeth, as well as to the branches of the inferior alveolar nerve.
For some patients with neurological disorders, the author prescribed exposure to a UHF electric field or a Sollux lamp already on the 2nd-3rd day after immobilization of the fragments; in the presence of pain along the inferior alveolar nerve, electrophoresis of a 0.5% solution of novocaine with adrenaline according to A.P. Parfenov (1973) was used. Other patients, according to indications, were prescribed only ultrasound. After 12 days, at the stage of formation of the primary bone callus, electrophoresis with a 5% solution of calcium chloride was prescribed.
Simultaneously with physical treatment, starting from the 2nd-3rd day, medicinal stimulants were also used: vitamins B6 B12; dibazol at 0.005; for deep disorders - 1 ml of 0.05% proserin solution according to the scheme. At the same time, drugs were prescribed to stimulate blood circulation (papaverine hydrochloride 2 ml of 2% solution; nicotinic acid 1% 1 ml; complamine 2 ml of 15% solution, for a course of 25-30 injections).
After a 7-10 day break, if nerve damage persisted, electrophoresis with 10% potassium iodide solution or electrophoresis with enzymes was prescribed for a course of 10-12 procedures; galantamine 1% 1 ml was used for a course of 10-20 injections, paraffin and ozokerite applications. After 3-6 months, if neurological disorders persisted, the treatment courses were repeated until complete recovery. An obligatory component of the treatment recommended by S. N. Fedotov is constant monitoring of its effectiveness according to neurological research methods. The use of the described complex of restorative treatment contributed to a more rapid restoration of the conductivity of the inferior alveolar nerve: for mild functional disorders - within 1.5-3 months, moderate and severe - within 6 months. In the group of patients treated with traditional methods, the conductivity of the inferior alveolar nerve with mild disorders was restored within 1.5-3-6 months, with disorders of moderate and severe degree - within 6-12 months. According to S. N. Fedorov, approximately 20% of patients had persistent and deep disorders of pain sensitivity for over a year. Moderate and severe injuries of the inferior alveolar nerve are most likely accompanied by overstretching of the nerve trunk at the time of displacement of fragments, contusions with a break in nerve fibers, partial or complete ruptures. All this slows down reinnervation. Earlier restoration of the trophic function of the nervous system had a beneficial effect on the quality and timing of consolidation of fragments. In the first (main) group of patients, consolidation of fragments occurred on average after 27 + 0.58 days, the periods of incapacity for work were 25 ± 4.11 days. The chewing function and muscle contractility reached normal values by 1.5-3 months. In the second (control) group, these indicators were 37.7+0.97 and 34+5.6 days, respectively, and the chewing function and muscle contractility were restored later - by 3-6 months. The specified measures for the follow-up treatment of patients with trauma should be carried out in rehabilitation rooms.
In addition to traumatic osteomyelitis, abscesses and phlegmons in case of jaw fractures, submandibular lymphadenitis may occur against the background of sluggish bone inflammation, which is not amenable to conventional treatment methods. Only with a detailed comprehensive examination of such patients using radiography, indirect radionuclide scan-lymphography using a colloidal solution of 198 Au, and immunodiagnostic tests can a diagnosis of secondary (post-traumatic) actinomycosis of the submandibular lymph nodes be confidently established.
It is possible that fractures of the lower jaw may be complicated by actinomycosis and tuberculosis simultaneously (more often in patients with tuberculosis). There may also be rarer but no less severe complications of maxillofacial injuries: Jansoul-Ludwig angina; late bleeding after osteosynthesis complicated by inflammation; asphyxia after intermaxillary traction, sometimes leading to the death of the patient due to aspiration of blood during bleeding from the lingual or carotid artery; false aneurysm of the facial artery; thrombosis of the internal carotid artery; secondary facial nerve paralysis (with a fracture of the lower jaw); facial emphysema (with a fracture of the upper jaw); pneumothorax and mediastinitis (with a fracture of the zygomatic bone and upper jaw), etc.
The length of stay of patients in hospital depends on the location of the injury to the maxillofacial region, the course of the consolidation period, and the presence of complications.
The specified terms are not optimal, in the future, as the economic crisis is overcome and the hospital bed capacity expands, it will be possible to extend the stay of patients in the hospital until the full completion of treatment for facial trauma of various localizations. Patients with maxillofacial injuries from rural areas should stay in the hospital longer, since they, as a rule, cannot come to the city for outpatient observation and treatment due to the distance. The availability of well-established trauma care, rehabilitation rooms for patients with such injuries in dental institutions of the city allows for a slight reduction in their stay in the hospital.
Outpatient treatment (rehabilitation) of victims with injuries to the maxillofacial region
The organization of the outpatient stage of treatment of victims with injuries to the maxillofacial region is not always sufficiently clear, since patients in many cases are under the supervision of doctors from various institutions who do not have sufficient training in the field of maxillofacial traumatology.
In this regard, it is possible to recommend using the experience of the rehabilitation room at the maxillofacial clinic of the Zaporizhzhya State Institute of Advanced Medical Studies and the regional dental clinic, which has introduced into its practice exchange cards containing all information about the treatment of the victim in the hospital, in the clinic at the place of residence and in the rehabilitation room.
When rehabilitating patients with maxillofacial injuries, it should be taken into account that such injuries are often combined with closed craniocerebral injuries and are also accompanied by dysfunction and structure of the temporomandibular joints (TMJ). The severity of these disorders depends on the location of the fracture: with condylar process fractures, degenerative changes in both joints are observed more often than with extra-articular fractures. Initially, these disorders have the character of functional insufficiency, which after 2-7 years can develop into degenerative changes. Unilateral arthrosis develops on the side of the injury after single fractures, and bilateral - after double and multiple fractures. In addition, all patients with mandibular fractures show, judging by electromyography data, pronounced changes in the masticatory muscles. Therefore, to ensure continuity in the follow-up treatment of trauma patients in dental clinics, they should be seen by a dentist-traumatologist who provides comprehensive treatment for patients with facial injuries of any localization.
Particular attention should be paid to the prevention of complications of an inflammatory nature and psychoneurological disorders - cephalgia, meningoencephalitis, arachnoiditis, autonomic disorders, hearing and vision impairment, etc. For this purpose, it is necessary to use physiotherapeutic methods of treatment and exercise therapy more widely. It is necessary to carefully monitor the condition of fixing bandages in the oral cavity, the condition of the teeth and mucous membrane, and also to carry out timely and rational dental prosthetics. When determining the terms of immobilization, the duration of temporary disability and treatment, it is necessary to approach each patient individually, taking into account the nature of the injury, the course of the disease, the age and profession of the patient.
The patient must complete treatment in the rehabilitation dental office. Therefore, by a special order of the relevant health department, the doctor of this office is granted the right to issue and extend certificates of temporary incapacity for work regardless of the patient's place of work and residence. It is desirable to organize one dental rehabilitation office for 200-300 thousand people. In the event of a decrease in the frequency of injuries, the tasks of the office can be expanded by providing assistance to surgical patients of other profiles, discharged from the hospital for outpatient treatment.
In rural areas, follow-up treatment of victims with injuries to the maxillofacial region should be carried out in district clinics (hospitals) under the supervision of a district dental surgeon.
The treatment system for patients with facial trauma should include a systematic examination of the long-term results of treatment.
Inpatient dental departments of regional hospitals and regional (territorial) dental clinics must implement organizational and methodological guidance for the provision of dental care in the region, including to patients with facial trauma.
Centers for specialized dental care are often clinical bases for departments of maxillofacial surgery of medical universities and institutes (academies, faculties) for advanced training of doctors. The presence of highly qualified personnel makes it possible to widely apply the latest methods of diagnostics and treatment of various injuries of the maxillofacial region and also allows for significant savings.
The chief dentist and maxillofacial surgeon of the region, territory, city, and the head of the maxillofacial department are faced with the following tasks to improve the state of care for victims of facial trauma:
- Injury prevention, including identification and analysis of the causes of industrial injuries, especially in agricultural production; participation in general preventive measures to prevent industrial, transport, street, and sports injuries; prevention of injuries to children; conducting extensive explanatory work among the population, especially young people of working age, in order to prevent domestic injuries.
- Development of necessary recommendations for providing first aid and first medical aid to patients with facial trauma at health centers, paramedic stations, trauma centers, ambulance stations; familiarization of mid-level medical personnel and doctors of other specialties with elements of first aid and first medical aid for facial trauma.
- Organization and implementation of ongoing cycles of specialization and advanced training for dentists, surgeons, traumatologists, and general practitioners on issues of providing assistance to patients with facial injuries.
- Application and further development of the most advanced methods of treating jaw fractures; prevention of complications, especially of an inflammatory nature; wider application of complex methods of treating traumatic facial injuries.
- Training of mid-level medical personnel with basic skills in providing first aid to patients with facial and jaw injuries.
When analyzing the quality indicators of dental institutions, the state of care for patients with facial injuries should also be taken into account. Particular attention should be paid to analyzing errors made in providing care. A distinction should be made between diagnostic, therapeutic and organizational errors, for which it is recommended to keep a special journal (for each city and district).
Selection of the method of reposition and fixation of jaw fragments in old fractures
Depending on the age of the fracture of the upper or lower jaw and the degree of stiffness of the fragments, orthopedic or surgical methods are used. Thus, in case of fractures of the alveolar process of the upper jaw with difficult-to-remove displacement of fragments, splints made of steel wire intended for skeletal traction are used. The elasticity of the steel wire facilitates the reduction of the fragment horizontally and vertically. In particular, if a fragment of the frontal section of the alveolar process is displaced backwards, a smooth splint-bracket is applied, fixing it in the usual way to the teeth on both sides of the fracture line; the teeth of the fragment are fixed to the wire with so-called "suspension" ligatures with slight tension. Gradually (at one time or over several days - depending on the age of the fracture), tightening the ligature wire by twisting, the fragment of the alveolar process is slowly reduced. For the same purpose, you can use thin rubber rings that cover the neck of the tooth and are fixed in front on a wire, which in this case does not necessarily have to be steel.
If the lateral section of the alveolar process of the upper jaw is displaced inward, the steel wire splint is bent to the shape of the normal dental arch. Gradually, the fragment returns to the correct position in relation to the lower dental arch. In the case of displacement of the lateral section of the alveolar process outward, it is adjusted inward using elastic traction installed across the hard palate.
In case of stiffness of the downwardly displaced fragment of the alveolar process of the upper jaw, rubber rings or a Shelgorn bandage applied through the surface of the teeth occlusion can be used for traction.
In case of stiffness of the lower jaw fragments, intermaxillary traction is used with the help of dental splints. If there are no teeth on the stiff jaw fragments, devices for repositioning and fixation of fragments can be used or repositioning and fixation of fragments can be performed through extraoral or intraoral access.
Examination of temporary disability in case of jaw fractures
Every citizen has the right to financial security in old age, in case of illness, total or partial loss of ability to work, as well as loss of a breadwinner.
This right is guaranteed by social insurance of workers, employees and peasants, benefits for temporary disability and many other forms of social security.
Loss of working capacity after an injury is stated in the event of the inability to perform socially useful work without damage to health and production efficiency.
In case of jaw fractures, temporary and permanent loss of working capacity is possible, the latter is divided into complete and partial.
If the jaw dysfunctions that prevent professional work are reversible and disappear with treatment, the disability is temporary. In case of total temporary disability, the victim cannot perform any work and requires treatment according to the regimen prescribed by the doctor. For example, patients with jaw fractures in the acute period of injury with severe pain syndrome and dysfunction are considered to be completely temporarily disabled.
Partial temporary disability is stated in cases where the victim is unable to work in his specialty, but can perform other work without harm to health, which ensures rest or an acceptable load on the damaged organ. For example, a miner in a mine who has a fracture of the lower jaw, with a delayed consolidation of fragments, is usually unable to work in his specialty for 1.5-2 months. However, after the elimination of acute phenomena 1.5 months after the injury, by decision of the VKK, the worker can be transferred to easier work (for a period of no more than 2 months): as a hoist operator, a charger in a lamp room, etc. When transferring to another job due to the consequences of a jaw fracture, sick leave certificates are not issued.
An expert examination of the victim should begin with establishing the correct diagnosis, which helps determine the work prognosis. Sometimes, having made the correct diagnosis, the doctor does not take into account the work prognosis. As a result, the victim is either prematurely discharged to work, or when his ability to work is restored, his sick leave is unreasonably extended. The first leads to various complications that adversely affect health and delay treatment; the second - to unjustified spending of funds on paying for sick leave.
Therefore, the main differential criterion for temporary loss of working capacity is a favorable clinical and working prognosis, characterized by complete or significant restoration of jaw dysfunction as a result of injury and working capacity in a relatively short period of time. Restoration of working capacity in case of jaw fractures is characterized by the degree of restoration of the function of the damaged jaw, namely: good consolidation of fragments in the correct position, preservation of normal dental occlusion, sufficient mobility in the temporomandibular joints, absence of pronounced disorders of blood and lymph circulation, pain and any other disorders associated with damage to the peripheral nerves in the maxillofacial region.
Temporary loss of working capacity due to jaw fractures may be caused by work-related injuries and domestic trauma. Determining the cause of temporary loss of working capacity due to jaw fractures is one of the important tasks of a dentist, since it is necessary to resolve issues that require not only medical but also legal competence.
An illness is considered to be related to an "industrial injury" in the following cases: while performing work duties (including a business trip during working hours), while performing an action in the interests of an enterprise or firm, although without the authority thereof; while performing public or state duties, as well as in connection with the performance of special assignments of state, trade union or other public organizations, even if these assignments were not related to the given enterprise or institution; on the territory of an enterprise or institution or in another place of work during working hours, including established breaks, as well as during the time necessary to put in order production tools, clothing, etc. before the start and after the end of work; near an enterprise or institution during working hours, including established breaks, if being there did not contradict the rules of the established routine; on the way to work or home from work; while performing a citizen's duty to protect law and order, save human life and protect state property.
To establish the cause of temporary disability, an accident report is required, which is drawn up promptly and in the correct form by the administration of the enterprise where the accident occurred. The report must indicate that the accident occurred during work, describe its nature, etc. In case of group accidents, reports must be drawn up for each victim.
An act cannot be drawn up if the accident occurred on the way to or from work. In these cases, it is necessary to have a certificate from the transport administration, a report drawn up by the police, a certificate from the enterprise or institution where the victim works, indicating the start and end time of his work on this date, as well as a certificate of residence.
The greatest difficulties arise when determining the nature of the loss of working capacity (temporary or permanent), as well as when establishing the end date of temporary loss of working capacity, which is individual for each patient.
It should be taken into account that in some cases the period of temporary disability does not correspond to the period for which the patient is issued a certificate of incapacity (for example, in case of a domestic injury, etc.). Therefore, to characterize the average period of disability, it is necessary to accurately indicate the period between the moment of injury and the moment the victim returns to work.
Patients with jaw fractures continue to be treated on an outpatient basis after the end of the inpatient treatment period, and until their disability group is established, the loss of ability to work is documented by a certificate of incapacity. However, the period of being on a certificate of incapacity for patients who are subsequently recognized as disabled cannot be identified with the average duration of temporary loss of ability to work. This period, preceding the transfer of the patient to disability, is correctly called the pre-disability period.
When deciding on the period of temporary disability, it is necessary to take into account not only the nature of the injury, but also the patient's profession, working and living conditions, and the type of injury (work or domestic injury, etc.). Thus, the ability to work is restored most quickly in the case of relatively minor sports injuries; in the case of industrial and transport injuries, the period of temporary disability is longer.
To exclude possible aggravation, objective research methods such as palpation, mastication, radiography, and osteometry should be widely used.
The period of disability for jaw fractures also depends on the characteristics of the victim's profession: for mental workers, temporary disability is shorter than for people engaged in physical labor; they can be discharged to work 20-25 days after the injury, continuing treatment on an outpatient basis. At the same time, patients whose profession is associated with constant tension and movement of the muscles of the maxillofacial region (artists, lecturers, musicians, teachers, etc.) are allowed to return to work only after full restoration of jaw function.
The period of temporary disability is especially long for patients engaged in heavy physical labor. For this group of patients, the sick leave is extended after the removal of fixing splints and devices for another 2-3 days for full adaptation of the chewing process. If they are discharged to work prematurely, complications may develop (osteomyelitis, jaw refractures, etc.). In addition, such patients are often unable to perform the full volume of basic work processes. For example, workers in the coal industry have a longer period of temporary disability than workers in other professions, which is due to the special specifics of work in underground conditions and the nature of injuries, which are often accompanied by damage to the soft tissues of the face.
In people over 50 years of age, the duration of the period of temporary disability increases due to a slowdown in consolidation.
Consolidation of the mandibular fracture in patients with periodontitis lasts 1.5-2 months longer. In patients without periodontitis, it occurs on average 3-4 months after the injury. Environmental factors should also be taken into account when determining both the duration of fixation and the period of temporary disability.
The use of compression extrafocal methods of treating jaw fractures in combination with general effects on the body and treatment of periodontitis, as well as timely and rational local orthopedic and surgical measures aimed at repositioning and fixing jaw fragments, help to reduce the period of temporary disability.
If in the acute period of injury the issues of examination of working capacity are relatively easy to resolve, then later, when the patient develops certain complications (delayed consolidation of fragments, contracture, ankylosis, etc.), difficulties arise in determining the period and type of loss of working capacity of the victim. Based on the nature of the fracture, its clinical course and the complications that have occurred, the dental surgeon must determine, at least approximately, the duration of temporary loss of working capacity of the victim and make a correct work prognosis, which is the criterion for establishing temporary or permanent disability.
The prognosis for work may be favorable, unfavorable, or questionable. With a favorable prognosis for work, it is possible to restore the ability to work and return the victim to his previous or equivalent work. The prognosis for work is unfavorable in cases where, as a result of the injury or its complications, the victim cannot work in his specialty and there is a need to transfer him to another job that corresponds to his state of health, or when the victim is unable to perform any work. A questionable prognosis for work means that at the time of the examination there is no data necessary to resolve the issue of the outcome of the jaw fracture and the possibility of restoring the ability to work. Certain difficulties are presented by the prognosis in case of delayed consolidation of jaw fractures complicated by traumatic osteomyelitis. In some cases, with the use of surgical, physiotherapeutic, and other methods of treatment, fusion of fragments in the correct position still occurs and the ability to work is restored, in others, despite the treatment, bone defects are formed that lead to a persistent impairment of work capacity.
It should be noted that the labor prognosis is closely related to the clinical one, depends on it, but does not always coincide with it. Thus, even with an unfavorable clinical outcome of jaw fractures (malunion without bite disorder or with edentulous jaws), the labor prognosis may be favorable, since it is determined not only by anatomical changes, but also, mainly, by the degree of restoration of function, the development of compensatory devices, the profession of the victim, as well as other factors.
Examination of temporary disability in case of fractures of the lower jaw
The average duration of temporary disability in case of mandibular fractures is 43.4 days. The time of recovery of working capacity depends on the location of the fractures. In cases of fractures in the area of the condylar process and the branch of the jaw with good alignment of bone fragments, the duration of the period of temporary disability is minimal (36.6 days). Fractures of such localization are usually closed and uninfected.
The main factors contributing to rapid consolidation are good blood supply to the bone in the fracture area and the presence of a muscular sheath, which allows the intermaxillary rubber traction to be removed on the 12th-14th day. Early functional treatment helps to accelerate the consolidation of jaw fragments.
The treatment of victims with fractures and dislocations of the condylar processes of the lower jaw presents great difficulties, as a result of which the period of temporary disability of persons engaged in physical labor is on average 60 days.
To assess the degree of consolidation of jaw fragments, it is useful to use the EOM-01-ts echoosteometer with an oscillation frequency of 120±36 kHz. The echoosteometry indicator when using, for example, the extrafocal device of V. A. Petrenko et al. (1987) for the treatment of condylar process fractures almost normalizes only on the 90th day. Therefore, it is obvious that the mentioned 60-day period, previously established in the "Methodological Recommendations", is subject to either scientific justification or change, especially in areas of radioisotope, industrial and chemical contamination of soil, water, and food products.
In cases of fractures of the lower jaw with a tooth in the fracture gap, the duration of the period of temporary loss of working capacity is significantly longer than in cases of fractures outside the dental arch.
In case of central fractures of the lower jaw, the recovery period for working capacity is almost the same as in case of fractures localized in its lateral sections (44.2 days).
The recovery period for single fractures of the lower jaw is on average 41.2 days, for patients with double fractures - 44.8 days. Multiple fractures of the lower jaw are the most severe, since they almost always involve significant displacement of fragments, which can protrude into the oral cavity. Such fractures are open and susceptible to infection. The average period of temporary disability for them is 59.6 days.
In case of comminuted fractures of the lower jaw, the period of recovery of working capacity is somewhat longer than in case of linear fractures and is equal to 45.5 days on average.
In patients with mandibular fractures combined with concussion, the average period of disability increases to 47.4 days. The question of the possibility of discharging such patients from the hospital should be decided jointly with a neurologist.
The period of loss of working capacity also depends on the methods used to treat fractures of the lower jaw. The period of recovery of working capacity in patients with fractures of the lower jaw treated by non-surgical methods is on average 43.7 days, by surgical methods - 41.3 days. The minimum periods of loss of temporary working capacity are observed in the treatment of fractures of the lower jaw without displacement of fragments with self-hardening plastic caps (26.3 days) and sling-shaped bandage Z. I. Urbanskaya (36.7 days). The working capacity of victims who had dental two-jaw aluminum splints used for the treatment of fractures of the lower jaw was restored later (after 44.6 days).
The main reasons for the increase in the period of recovery of working capacity are long-term intermaxillary fixation without the use of early functional treatment, relative mobility of fragments, trauma to the interdental papillae of the gums by wire splints, loosening of teeth, etc.
 [ 18 ]
[ 18 ]
Examination of temporary disability in case of fractures of the upper jaw
The average duration of the period of temporary disability due to fractures of the upper jaw is 64.9 days.
The average duration of the period of incapacity for work depends on the nature of the injury to the upper jaw: in the case of a non-work injury it is 62.5 days, and in the case of an work injury - 68.3 days.
The duration of disability due to injury is determined to a certain extent by the severity of the injury. Recovery of working capacity due to a fracture of the alveolar process of the maxilla occurs on average within 43.6 days, and in case of a fracture of the body of the maxilla, the average period of disability is 69.9 days; according to Le Fort I type - 56.0 days, according to Le Fort II type - 65.4 and according to Le Fort III type - 74.7 days.
In uncomplicated fractures of the upper jaw, the period of incapacity for work is on average 60.1 days, and in complicated fractures - 120-130 days.
One of the features of maxillary fractures is their combined nature, due to the anatomical proximity of the facial and cerebral parts of the skull. Traumatic injuries to the bones of the skull and brain are not always diagnosed by dentists, which negatively affects the treatment of patients.
The periods of temporary disability for isolated and combined fractures of the upper jaw are different. Thus, for a fracture of the upper jaw combined with a concussion, they are 70.8 days, with a combination with a fracture of the lower jaw, the average periods of disability are 73.3 days, with a fracture of the base of the skull - 81.0 days, with a fracture of the vault of the skull - 126.7, with damage to the orbit - 120.5, with a fracture of other bones - 89.5 days.
Multiple fractures of the bones of the face, skull and trunk result in temporary disability of up to 87.5 days.
The duration of temporary disability also depends on the methods of treatment of upper jaw fractures. When orthopedic methods of treatment are used in patients with upper jaw fractures, the average duration of temporary disability is 59.2 days (55.4 for uncomplicated and 116.0 for complicated fractures), and when surgical methods are used, it is 76.0 days (69.3 for uncomplicated and 153.5 for complicated fractures).
The longer period of temporary disability with surgical methods of fracture treatment is due to the fact that they are used for the most severe injuries, when orthopedic methods are not indicated or ineffective.
 [ 19 ]
[ 19 ]
Registration of temporary disability
A dentist has the right to issue a sick leave certificate to a patient with a jaw fracture for a period of no more than six days. Medical control commissions (MCC) have the right to extend the sick leave certificate for a longer period (for patients with an injury, for up to 10 days at a time), but in general no more than 4 months from the date of injury. In this case, the persons who authorize the extension of the sick leave certificate are required to personally examine the patient. In the case of a long-term course of the disease, such examinations should be carried out at least once every 10 days, and if necessary, much more often, especially in the first period after the injury.
In the event of loss of ability to work due to an industrial injury, the doctor issues a certificate of incapacity for work, which is a document confirming temporary incapacity for work and giving the right to the injured party to receive social insurance benefits.
In case of loss of ability to work due to a domestic injury, the medical institution issues a certificate of incapacity for five days, and starting from the sixth day - a certificate of incapacity. In the event that the injured person contacts the doctor on the day that he has already worked at work, the doctor, if necessary, issues a certificate of incapacity, dating it on the day of the request, but releases the injured person from work only from the next day.
Patients with jaw fractures who are being treated in hospital are issued a sick leave certificate upon discharge, but in cases of a long stay in hospital, a certificate of incapacity for work can be issued before discharge in order to receive wages.
If the patient's ability to work is restored as a result of inpatient treatment, the sick leave certificate is closed. In the event that the patient remains incapacitated upon discharge from the hospital due to the consequences of the fracture, the sick leave certificate is not closed in the hospital, but a corresponding note is made on it about the need for outpatient treatment. Subsequently, the sick leave certificate is extended by the dentist of the medical and preventive institution where the patient continues treatment. It should be noted that persons who have received an injury due to intoxication or during actions due to intoxication and who need outpatient and inpatient treatment are not issued sick leave certificates.
The issue of discharging a patient to work or referring him/herself to the VTEK with a simple or complicated fracture of the upper jaw is decided depending on the clinical and work prognosis. In cases where, despite all therapeutic measures, the clinical and work prognosis remains unfavorable and the impairment of work capacity becomes persistent, patients should be referred to the VTEK to determine the disability group, for example, in the case of a fracture of the lower jaw complicated by osteomyelitis with subsequent formation of a large bone tissue defect and in the event of the need for restorative bone-plastic surgeries. In such cases, timely determination of the disability group and the release of the patient from work allow for the implementation of a full range of therapeutic measures to restore the health of the victim, after which he/she can perform work in his/her or any other specialty. The certificate of incapacity for work is closed on the day the VTEK conclusion is issued on the establishment of disability, regardless of its causes and group.
Rational employment of disabled people is of great importance, since feasible work contributes to a more rapid restoration or compensation of impaired functions, improves the general condition of disabled people and increases their material security.
Sometimes concomitant diseases, which in themselves do not cause significant impairment of working capacity, aggravate the patient's condition and, in combination with the main disease, cause more pronounced impairment of functions. Therefore, when conducting an examination of working capacity in such cases, extreme caution and a critical approach are necessary in order to correctly assess the specific weight of the said changes in the matter of reduction or loss of working capacity.

