Medical expert of the article
New publications
Exacerbation of chronic cystitis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Infectious and inflammatory disease of the bladder mucosa begins suddenly with frequent urge to urinate, pain and burning during urination, pain in the lower abdomen, and other ailments. This condition requires a response. The absence of therapy or its insufficiency leads to the transition of cystitis into a chronic condition, in which periodic exacerbations are possible.
Recurrent urinary tract infection (RUTI) is defined as three episodes of exacerbation with three positive urine cultures within a 12-month period or two infections within the previous 6 months.[ 1 ]
Epidemiology
Urinary tract infections are more common in women than in men, with a ratio of 8:1. [ 2 ] Recurrent UTIs (RUTIs) are mainly caused by repeated infection with the same pathogen.
According to statistics, in a third of all cases of cystitis, it becomes chronic. Most exacerbations occur in the first 3 months after the acute form. Every sixth man and every second woman are subject to relapse.
Survey data show that 1 in 3 women will be diagnosed and treated for a UTI by age 24, and more than half of these will have one during their lifetime.[ 3 ] One 6-month study found that 27% of cases of chronic cystitis recur once and 3% recur two or more times.[ 4 ]
Causes exacerbation of chronic cystitis
Chronic cystitis has both periods of calm and relapses. What are the causes of exacerbations? The following can be distinguished:
- poor personal hygiene leading to infection in the urethra;
- uncontrolled long-term use of medications that provoke irritation of the organ walls;
- stagnation of fluid in the bladder (it is impossible to restrain the urge to defecate);
- constipation;
- wearing tight underwear and trousers, which causes blood stagnation in the pelvic organs;
- bladder injuries;
- hypothermia and other factors that reduce immunity;
- allergy to intimate hygiene products;
- kidney disease, presence of stones in the kidneys;
- sexually transmitted infections.
Risk factors
Major risk factors that predispose to recurrent uncomplicated UTI include menopause, family history, sexual activity, spermicide use, and recent antimicrobial use.[ 5 ]
Intensive sexual activity can contribute to the exacerbation of cystitis. This does not always indicate the presence of a sexually transmitted infection. Physical impact, friction of the external genitals leads to inflammation of their tissues, which also affects the urethra. In women, exacerbation can be provoked by the penetration of strains of microorganisms alien to her immunity.
The patient's age plays a significant role in the development of the disease. In older people, such phenomena occur more often due to a slowdown in the processes of epithelial regeneration. In postmenopausal women, the frequency of UTIs is higher due to pelvic prolapse, lack of estrogen, a decrease in the number of lactobacilli in the vaginal flora, increased periurethral colonization with Escherichia coli (E. coli), and a higher incidence of diseases such as diabetes mellitus. [ 6 ]
The risk factor for an outbreak of the disease is the period before menstruation. This is due to hormonal surges characteristic of the cycle, and may be a manifestation of such pathologies as uterine fibroids, endometriosis.
Chronic infections of other organs also lead to exacerbations of bladder inflammation, and a lack of vitamins in the body.
There is a large group of patients with painful bladder syndrome, or interstitial cystitis, whose symptoms are aggravated by certain foods. The most common foods include coffee, tea, soda, alcoholic beverages, citrus fruits and juices, artificial sweeteners, and hot peppers.[ 7 ]
In the treatment of chronic cystitis, the biologically active supplement "Urolife" is often used in a solution for instillations to restore the protective layer of the bladder or in the form of oral capsules (they act as a protector, maintaining a constant concentration of active substances in the epithelium of the organ). In case of hypersensitivity to the components of the product, exacerbations are also possible.
Pregnancy, diabetes mellitus, and immunosuppression increase the risk of recurrent urinary tract infections (RUTI) in women by facilitating access to uropathogens that overcome the body's normal defense mechanisms. [ 8 ] Patients with diabetes mellitus have a higher risk of developing asymptomatic bacteriuria, UTI, and pyelonephritis.
Pathogenesis
The intact urothelium of the bladder walls is able to protect itself by synthesizing phagocytes, the action of which is aimed at suppressing the growth of pathogenic bacteria. The occurrence of a damaging factor due to the listed reasons, leading to hypoxia, transient dysfunction of the immune system, leads to an exacerbation of the pathology.
The recurrent infection process results from the failure of tissue regeneration. Ascending infection is thought to be caused by bacterial virulence factors that allow for improved adhesion, infection, and colonization by uropathogens. Common uropathogens include Escherichia coli, Staphylococcus saprophyticus, Klebsiella pneumoniae, and Proteus mirabilis.[ 9 ]
The pathogenesis of recurrent UTI or exacerbation of chronic cystitis involves bacterial reinfection or bacterial persistence, with the former being much more common.[ 10 ] When bacteria persist, the same bacteria can be cultured in urine 2 weeks after initiation of susceptibility-corrected therapy. Reinfection is a relapse with a different organism, the same organism 2 weeks after treatment, or a sterile intermediate culture.[ 11 ]
Symptoms exacerbation of chronic cystitis
The first signs of pathology are difficult to miss, since its symptoms cause pain, discomfort when emptying the bladder, and the frequency of urges is especially annoying.
Common symptoms of acute exacerbation of chronic cystitis include dysuria, urinary frequency, suprapubic pain, and possible hematuria. Systemic symptoms are usually mild or absent. Urine may be foul-smelling and cloudy. Diagnosis is based on characterization of clinical features, history, three positive urine cultures within the previous 12-month period in symptomatic patients, and the presence of neutrophils in the urine (pyuria).[ 12 ] Urinary symptoms are present in 25–30% of women with RUTI. The likelihood of finding a positive culture in the presence of the above symptoms and no vaginal discharge is about 81%.[ 13 ] In complicated UTIs such as pyelonephritis, UTI symptoms will persist for more than a week with systemic symptoms of persistent fever, chills, nausea, and vomiting.[ 14 ]
The pain is most often localized in the pubic area or deep in the pelvis. The pain appears mainly at the end of urination, but can also occur at the beginning. All this is accompanied by a general feeling of being unwell, and sometimes the body temperature rises.
Urine becomes cloudy, flakes may float in it, and blood may be mixed in.
Exacerbation of cystitis during pregnancy
Pregnancy is often accompanied by an exacerbation of cystitis. This does not happen by chance. The growing uterus compresses the bladder and ureter. The outflow of urine and blood circulation are disrupted, which leads to the development of infection.
In the early stages of pregnancy, inflammation is promoted by decreased immunity due to hormonal changes. During pregnancy, manifestations of pathology cannot be neglected, since this can negatively affect not only the health of the expectant mother, but also the child, leading to a miscarriage. [ 15 ]
In pregnancy, factors that contribute to the risk of exacerbation of chronic cystitis include dilation of the ureter and renal pelvis; increased urine pH; decreased ureteral muscle tone and glucosuria, which promote bacterial growth. Treatment of asymptomatic bacteriuria in pregnancy reduces the risk of developing pyelonephritis. Because RUTIs are common during pregnancy, they require prophylactic treatment. Screening for bacteriuria is recommended for all pregnant women at their first antenatal visit and again in the third trimester.[ 16 ] They should then be treated with antibiotics such as nitrofurantoin, sulfisoxazole, or cephalexin.[ 17 ],[ 18 ] Antibiotic prophylaxis of RUTIs in pregnancy is effective when used as continuous or postcoital regimens. The causative organisms of UTIs during pregnancy are similar to those found in non-pregnant patients, with E. coli accounting for 80–90% of infections. [ 19 ], [ 20 ]
Complications and consequences
Untreated cystitis is dangerous not only because it becomes chronic, but also because of more severe consequences and complications related to kidney damage, such as inflammation of the organ - pyelonephritis. If bacteria enter the bloodstream, they can cause serious complications, including septicemia, shock and, rarely, death. [ 21 ]
Diagnostics exacerbation of chronic cystitis
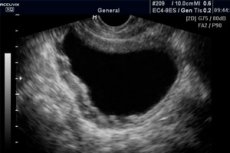
Diagnosis of cystitis is carried out according to the clinical picture characteristic of the disease, and also requires laboratory and instrumental studies (including cystoscopy, CT urogram or ultrasound of the abdominal cavity), an analytical approach to the results obtained. [ 22 ] Examination of the patient includes a thorough collection of anamnesis, other existing stages of diagnosis, necessarily taking into account the condition of the genitals and the characteristics of sexual life.
Bacteriological examination of urine is a basic analysis for cystitis. It is also necessary to determine the sensitivity of flora to antibiotics. General urine and blood tests are also done to detect leukocytes. Based on the presumed diagnosis, others are possible, for example, for venereal diseases.
Of the instrumental methods, ultrasound of the pelvic organs and upper urinary tract is most often used. X-rays of the organs may also be needed. At the final stage, an endoscopic examination is mandatory, but a complete picture of histological changes in the bladder mucosa will be clarified by optical coherence tomography (OCT) and multifocal biopsy.
Differential diagnosis
Exacerbation of cystitis is differentiated from gynecological and venereal diseases, acute appendicitis. Changes in the walls of the organ caused by the chronic course of the pathology are similar to dysplasia, metaplasia, hyperplasia - precancerous conditions. OCT is used for clarification.
Treatment exacerbation of chronic cystitis
Cystitis is treated with antibacterial drugs, herbal diuretics, but to get the right therapy, you need to see a doctor and get tested.
If it happens at an inappropriate time or place, what should you do? What emergency aid can be used?
Patients should be encouraged and encouraged to drink plenty of fluids (two to three liters per day) and urinate frequently to help flush bacteria from the bladder. Holding urine for long periods of time allows bacteria to multiply in the urinary tract, leading to cystitis.
Women are advised to avoid spermicidal contraceptives, diaphragms, and vaginal douches, which can irritate the vagina and urethra and promote bacterial entry and colonization in the urinary tract. It is best to avoid skin allergens introduced into the genital area, such as bubble baths, bath oils, vaginal creams and lotions, deodorant sprays, or soaps, as these can alter the vaginal flora and eventually lead to UTIs.[ 23 ]
You can put a warm heating pad on the lower abdomen or between the legs, take a pain reliever, antispasmodic, or nonsteroidal anti-inflammatory drug.
Medicines
Continuous low-dose antibiotic prophylaxis is effective in preventing UTIs. A 2008 Cochrane Database systematic review pooled 10 trials involving 430 women to evaluate continuous antibiotic prophylaxis versus placebo. A meta-analysis of these trials found that the relative risk of clinical relapse per patient-year (CRPY) was 0.15 (95% CI 0.08–0.28) in favour of antibiotics. The relative risk of severe adverse events (requiring treatment discontinuation) was 1.58 (95% CI 0.47–5.28) and other adverse events was 1.78 (95% CI 1.06–3.00) in favour of placebo. Adverse events included vaginal and oral candidiasis and gastrointestinal symptoms. Severe adverse events were most commonly skin rash and severe nausea. No additional trials were identified to contradict this systematic review.[ 24 ]
Because the optimal prophylactic antibiotic is unknown, antibiotic choice should be guided by allergy, prior susceptibility, local resistance patterns, cost, and side effects. Nitrofurantoin and cephalexin have demonstrated the highest efficacy. Before prophylaxis, patients should understand common side effects and the fact that serious side effects are rare.[ 25 ]
Ampicillin, amoxicillin, and sulfonamides are no longer the drugs of choice for empirical treatment due to widespread resistance in 15–20% of E. coli.[ 26 ],[ 27 ] Nitrofurantoin or amoxicillin/clavulanic acid remain effective in terms of bacterial susceptibility, but nitrofurantoin should be avoided in patients with pyelonephritis due to its low serum and tissue levels. Less than 5% of E. coli strains are resistant to nitrofurantoin, while other strains are often resistant.
Penicillins and cephalosporins are considered safe during pregnancy, but trimethoprim, sulfonamides, and fluoroquinolones should be avoided. Oral antibiotic therapy resolves 94% of uncomplicated UTIs, although recurrence is not uncommon. Recently published International Clinical Practice Guidelines for the Management of Acute Cystitis recommend a 3-day regimen of trimethoprim-sulfamethoxazole (TMP-SMX) and a 5-day course of nitrofurantoin as first-line therapy for uncomplicated UTIs. A 5-day course of nitrofurantoin has high efficacy, equivalent to a 3-day course of TMP-SMX.[ 28 ],[ 29 ] A 3-7 day regimen of beta-lactams such as cefaclor or amoxicillin/clavulanic acid is appropriate when first-line therapy cannot be used. Although a 3-day course of fluoroquinolones can be quite effective, it is not generally recommended as first-line therapy due to emerging resistance and their potential side effects, as well as high cost; however, fluoroquinolones are the drug of choice in women who experience poor tolerability or allergic reaction after empirical therapy [ 30 ]. A meta-analysis showed that a single-dose regimen of fosfomycin trometamol is a safe and effective alternative for the treatment of UTI in both pregnant and non-pregnant women, as well as in the elderly and children. Due to its low efficacy, amoxicillin and ampicillin should not be used for the empirical treatment of UTI.
If you have chronic cystitis, you need to have several medications in your home medicine cabinet that can help in case of a sudden exacerbation. Among them are monural and urolesan.
- Monural is a broad-spectrum antibiotic that prevents bacteria from attaching to the epithelium of organ walls. It is taken on an empty stomach before bedtime once after dissolving the powder in half a glass of water.
Not prescribed to children under 12 years of age, women during breastfeeding. Pregnant women can take the drug on the advice of a doctor if there is an urgent need. Animal testing did not reveal any harmful effects on the fetus. Side effects may include heartburn, diarrhea, dizziness, and fatigue.
Monural is contraindicated for people with hypersensitivity to its components, severe renal failure, and undergoing hemodialysis.
- Urolesan - has 3 forms of release: capsules, drops, syrup. Contains a combination of many extracts and oils of medicinal plants. The drug is taken before meals in doses: 8-10 drops per sugar for adults, 5-6 drops for children aged 7-14; syrup: 5 ml and 2-4 ml, respectively; capsules: after 14 years - 1 pc. Three times a day.
Possible side effects include nausea, belching, skin rashes, itching, headache, and slow heartbeat. Contraindicated for children under the above age, pregnant and lactating women, people with ulcers, erosions, and kidney stones larger than 3 mm.
Other antibacterial agents used include fluoroquinolones: ofloxacin, norfloxacin, lomefloxacin.
As a rule, patients with chronic cystitis have abnormalities in their immune status. Immunotherapeutic drugs are used to stimulate immune mechanisms, one of which is Uro-Vaxom.
- Uro-vaxom - in acute situations, take one capsule daily in the morning before meals for at least 10 days in combination with other treatment. Children can be treated starting from 4 years of age by mixing the contents of the capsule with juice or water. The effect on pregnancy and breastfeeding has not been studied.
The drug can cause abdominal discomfort, swelling in the mouth, skin rash, itching, and sometimes fever.
To treat urogenital diseases in women, sex hormones - estrogen - are used. An example of this is the drug ovestin.
- Ovestin - its active substance is estriol. It is prescribed for replacement therapy in case of atrophy of the mucous layer of the lower parts of the genitourinary system. The suppository is inserted into the vagina once a day. It is not used in case of thrombosis, tumors of the mammary glands and genitals, bleeding, diabetes mellitus, gallstone disease, pancreatitis, epilepsy, asthma. It can cause local reactions: itching, vaginal irritation, and soreness of the mammary glands.
Estrogen use stimulates the proliferation of lactobacilli in the vaginal epithelium, lowers pH, and prevents colonization of the vagina by uropathogens. After menopause, estrogen levels and lactobacilli fall; this plays an important role in the development of bacteriuria and makes postmenopausal women susceptible to UTI. Vaginal estrogen use reduces RUTI by 36–75% and has minimal systemic absorption. A Cochrane review in postmenopausal women with RUTI compared with placebo found that vaginal estrogens prevented RUTI, but oral estrogen did not have the same effect.[ 31 ],[ 32 ] Topical estrogen creams twice weekly and an estradiol-releasing vaginal ring are both effective in reducing attacks of RUTI. [ 33 ], [ 34 ] They restore vaginal flora, lower pH and therefore reduce UTIs; however, it takes at least 12 weeks for vaginal lactobacilli to reappear when using an estrogen vaginal ring. [ 35 ] Although evidence does not support the use of a specific type or form of vaginal estrogen, topical creams are less expensive than the estradiol-releasing vaginal ring but have more side effects.
Probiotics are beneficial microorganisms that may protect against UTIs. Lactobacillus strains are the best known probiotics and are found in fermented milk products, mainly yogurt. Other probiotics include Lactobacilli bifidobacteria, rhamnosus, casei, bulgaricus, and salivarius; Streptococcus thermophiles, and Enterococcus faecium. Reid et al. showed in vitro that lactobacilli can prevent uropathogenic infections. [ 36 ] Other studies have shown that L. rhamnosus gr-1 and L. fermentum rc-14 can colonize the vagina, which could subsequently prevent UTIs. However, more clinical studies are needed to determine their role in the prevention of RUTIs. [ 37 ]
Vitamins
Since exacerbations of cystitis often occur due to a lack of vitamins, a decrease in the body's defenses, they should be included in the complex treatment of the pathology. Multivitamin complexes containing vitamins A, C, E, B, as well as food products rich in them, with the exception of citrus fruits and tomatoes, are considered beneficial in terms of their effect on the genitourinary organs.
Physiotherapy treatment
A very effective method in the treatment of cystitis is hydrotherapy. The mineral water "Naftusya" has proven itself in this.
Recent studies show that the rate of cystitis among cystitis-prone women who received acupuncture was one-third less than among untreated women, and half that among women treated with sham acupuncture. Thus, acupuncture may prevent RUTI in healthy adult women. [ 38 ], [ 39 ], [ 40 ]
Folk remedies
Folk recipes can alleviate the patient's condition, speed up recovery, but do not replace it. Drinking plenty of cranberry and lingonberry juice, rosehip and chokeberry infusions, which contain a large amount of vitamin C, remove pathogenic microorganisms and improve immunity. A Cochrane review found that the evidence for the benefits of cranberry juice in preventing UTIs is limited; thus, cranberry juice cannot be recommended for preventing UTIs. [ 41 ]
Phytotherapy is effective for recurrent urinary tract infections. [ 42 ] Warm baths with decoctions of soothing, anti-inflammatory, disinfectant herbs: succession, [ 43 ] chamomile, [ 44 ] calendula, [ 45 ] eucalyptus leaves, [ 46 ] will reduce the symptoms of the disease.
A major role in the therapy of exacerbations of cystitis belongs to the internal use of herbal potions. The leaders in this are knotweed, bearberry, pol-pola, corn silk, parsley seeds, shepherd's purse.
Homeopathy
In pharmacies you can buy homeopathic preparations, the parallel use of which with the main treatment will speed up recovery. Thus, the complex remedy Arnica-Heel is indicated for acute and chronic diseases of bacterial and viral origin. Drops are dissolved in water (10 drops per 10 ml) and taken 3 times a day 20 minutes before meals or an hour after. Not prescribed to pregnant women and children. Cases of side effects are very rare and manifest themselves in the form of allergies or intestinal disorders.
Berberis-Gomacord - a herbal preparation relieves pain and inflammation of the genitourinary tract. It is used for children from 12 years of age. Ten drops of the solution are mixed with water or immediately under the tongue and held there for some time before swallowing. Contraindicated in case of allergy to the components and in the first trimester of pregnancy.
Gentos - tablets, relieve inflammation, swelling, improve blood circulation in the pelvic organs, reduce congestion. Children 5-12 years old are recommended half a tablet 2 times a day, teenagers and adults - a whole one. At the acute stage of cystitis in the first 2 days, the frequency of administration can be increased to 4 times. Possible side effects: skin rashes, itching.
Kalium floratum salt Dr. Schussler No. 4 - tablets, used for the youngest patients: up to one year 1 tablet 2 times, 1-5 years - 3 times, 6-11 years - 4 times, after 12 years - 6 times during the day. The drug is contraindicated in case of wheat allergy. There is also a primary temporary exacerbation of the pathology, which requires stopping treatment and consulting a doctor.
Diet for exacerbation of cystitis
Chronic cystitis, especially its exacerbation, requires a special diet. It is necessary to exclude spicy, salty, smoked, spicy foods, alcohol from food. The menu should contain more non-acidic vegetables and fruits (fresh cucumbers, zucchini, cauliflower, melons, watermelons, pears, peaches), as well as cottage cheese, fermented milk products. Compotes, juices, weak tea should be consumed.
Prevention
There is no convincing evidence for conservative measures to prevent recurrent UTIs. Modifiable predisposing factors for UTIs, including sexual activity and use of spermicides, may be recommended to patients.[ 47 ],[ 48 ]
In case of cystitis, as preventive measures, it is necessary to observe proper hygiene of the genitourinary organs, anus after defecation, dress according to the weather, do not sit on cold surfaces, maintain your immunity with good and proper nutrition, vitamin complexes. Sufficient daily drinking is another way to avoid exacerbations.
The evidence supporting lactobacilli probiotics in the prevention of UTIs is also inconclusive.[ 49 ],[ 50 ]
Preventive measures against recurrent uncomplicated urinary tract infections:
- Conservative measures, including limiting the use of spermicides and postcoital voiding, have no evidence of effectiveness but are unlikely to be harmful (evidence level 4, grade C recommendation).
- Cranberry products have conflicting evidence on their effectiveness (evidence level 1, recommendation grade D).
- Continuous antibiotic prophylaxis [ 51 ] is effective for preventing UTIs. (Evidence level 1, recommendation level A).
- Postcoital antibiotic prophylaxis within 2 hours of intercourse is also effective in preventing UTIs (level of evidence 1, grade A recommendation).
- Self-initiation of antibiotic therapy with a 3-day dose of antibiotic for symptomatic treatment is another safe treatment option for recurrent uncomplicated UTI (level of evidence 1, grade A recommendation).
Oral immunoprophylaxis may be an effective alternative to antibiotics in preventing exacerbations of chronic cystitis. A meta-analysis of 5 studies showed that the oral immunoprophylaxis drug Uro-Vax® with E. coli extract (Terra-Lab, Zagreb, Croatia) taken for 3 months was effective in preventing exacerbations of chronic cystitis for 6 months. [ 52 ] Another double-blind study confirmed that E. coli extracts are effective and well tolerated in the treatment of UTIs, reducing the need for antibiotics and preventing UTIs. [ 53 ]
Forecast
Timely treatment, the recommended course even if symptoms disappear (usually internal processes are longer than external manifestations) gives a favorable prognosis for recovery. Ignoring the problem threatens kidney damage.

