Medical expert of the article
New publications
Erythema nodosum
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Erythema nodosum (synonym: erythema nodosum) is a syndrome based on allergic or granulomatous inflammation of the subcutaneous tissue. The disease belongs to the group of vasculitis. Erythema nodosum is a polyetiological form of deep vasculitis.
Erythema nodosum is an independent form of panniculitis, which is characterized by the formation of red or purple palpable subcutaneous nodes on the shins and sometimes in other areas. Often develops in the presence of a systemic disease, especially with streptococcal infections, sarcoidosis and tuberculosis.
What causes erythema nodosum?
Erythema nodosum most often develops in women in their 20s and 30s, but can occur at any age. The etiology is unknown, but a connection with other diseases is suspected: streptococcal infection (especially in children), sarcoidosis, and tuberculosis. Other possible triggers are bacterial infections (Yersinia, Salmonella, mycoplasma, chlamydia, leprosy, lymphogranuloma venereum), fungal infections (coccidioidomycosis, blastomycosis, histoplasmosis), and viral infections (Epstein-Barr, hepatitis B); drug use (sulfonamides, iodides, bromides, oral contraceptives); inflammatory bowel disease; malignancy, pregnancy. 1/3 of cases are idiopathic.
The cause of erythema nodosum is primary tuberculosis, leprosy, yersiniosis, venereal lymphogranuloma and other infections. The occurrence of the disease after taking drugs containing the sulfanilamide group, contraceptives has been described. In half of the patients, the cause of the disease cannot be identified. The pathogenesis of the disease is characterized by a hyperergic reaction of the body to infectious agents and drugs. It develops in many acute and chronic, mainly infectious, diseases (tonsillitis, viral, yersiniosis infections, tuberculosis, leprosy, rheumatism, sarcoidosis, etc.), drug intolerance (iodine, bromine, sulfonamides), some systemic lymphoproliferative diseases (leukemia, lymphogranulomatosis, etc.), malignant neoplasms of internal organs (hypernephroid cancer).
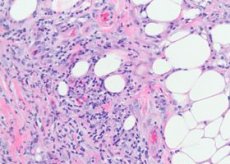
Pathomorphology of erythema nodosum
The vessels of the subcutaneous tissue are mainly affected - small arteries, arterioles, venules and capillaries. In the dermis, the changes are less pronounced, manifested only by small perivascular infiltrates. In fresh lesions, clusters of lymphocytes and a varying number of neutrophilic granulospas appear between the lobules of fat cells. In some places, more massive infiltrates of a lymphohistiocytic nature with an admixture of eosinophilic granulocytes can be seen. Capillaritis, destructive-proliferative arteriolites and venulitis are noted. In larger vessels, along with dystrophic changes in the endothelium, infiltration by inflammatory elements is found, in connection with which some authors believe that vasculitis with primary changes in the vessels underlies the skin lesion in this disease. In old elements, neutrophilic granulocytes are usually absent, granulation changes with the presence of foreign body cells predominate. Characteristic of this disease is the presence of small histiocytic nodules located radially around the central fissure. Sometimes these nodules are penetrated by neutrophilic granulocytes.
The histogenesis of erythema nodosum is poorly understood. Despite the undoubted association of the disease with a wide variety of infectious, inflammatory and neoplastic processes, in many cases it is not possible to identify the etiologic factor. In some patients, circulating immune complexes, increased levels of IgG, IgM and complement component C3 are detected in the blood.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ]
Histopathology
Histologically, the substrate of erythema nodosum is a perivascular infiltrate consisting of lymphocytes, neutrophils, a large number of histiocytes, endothelial proliferation of subcutaneous veins, capillary arterioles, edema of the dermis due to increased permeability of the vascular membrane, and acute nodular dermohypodermitis.
Symptoms of Erythema Nodosum
Erythema nodosum is characterized by the formation of erythematous soft plaques and nodules, which is accompanied by fever, general malaise and arthralgia.
Erythema nodosum type rashes are one of the main manifestations of Sweet's syndrome (acute febrile neutrophilic dermatosis), which is also characterized by high temperature, neutrophilic leukocytosis, arthralgia, the presence of other polymorphic rashes (vesiculopustular, bullous, erythema multiforme exudative type, erythematous, plaque, ulcerative), located mainly on the face, neck, limbs, in the development of which immune complex vasculitis is important. A distinction is made between acute and chronic erythema nodosum. Acute erythema nodosum usually occurs against the background of fever, malaise, manifested by rapidly developing, often multiple, fairly large dermohypodermal nodes of oval outlines, hemispherical shape, slightly raised above the surrounding skin, painful on palpation. Their borders are unclear. The predominant localization is the anterior surface of the shins, knee and ankle joints, the rash can also be widespread. The skin above the nodes is initially bright pink, then the color becomes bluish. A change in color over several days is characteristic, like a "blooming" bruise - from bright red to yellow-green. Resorption of the nodes occurs within 2-3 weeks, less often later; relapses are possible.

The acute process is characterized by nodular, dense, painful on palpation foci of a hemispherical or flattened shape. The rash often appears in waves, localized symmetrically on the extensor surfaces of the shins, less often on the thighs, buttocks, forearms. A few days after the appearance, the foci begin to regress with a characteristic change from pinkish-livid-red to livid-brownish and greenish-yellow according to the type of "blooming bruise". The evolution of the element is 1-2 weeks. The nodes do not merge with each other and do not ulcerate. An outbreak of rashes is usually noted in spring and autumn. They are accompanied by general phenomena: fever, chills, joint pain. Nodular erythema can acquire a chronic migratory character (nodular migratory erythema of Befverstedt).
Diagnosis of erythema nodosum
The diagnosis of erythema nodosum is made clinically, but other investigations should be performed to determine the causative factors, such as biopsy, skin testing (purified protein derivative), complete blood count, chest x-ray, throat swab. The erythrocyte sedimentation rate is usually elevated.
The disease should be differentiated from Bazin's erythema indurated, Montgomery-O'Leary-Barker nodular vasculitis, subacute migratory thrombophlebitis in syphilis, primary coliquative tuberculosis of the skin, Darier Russi's subcutaneous sarcoid, and skin neoplasms.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment of erythema nodosum
Erythema nodosum almost always resolves spontaneously. Treatment includes bed rest, elevation of the limb, cool compresses, and nonsteroidal anti-inflammatory drugs. Potassium iodide 300-500 mg orally 3 times daily is used to reduce inflammation. Systemic glucocorticoids are effective but should be used as a last resort because they may worsen the underlying disorder. If the underlying disorder is identified, treatment should be started.
Prescribe antibiotics (erythromycin, doxycycline, penicillin, ceporin, kefzol); desensitizing agents; salicylates (aspirin, askofen); vitamins C, B, PP, askorutin, rutin, flugalin, sinkumar, delagyl, plaquenil; angioprotectors - complamin, escusan, diprofen, trental; anticoagulants (heparin); non-steroidal anti-inflammatory drugs (indomethacin 0.05 g 3 times a day, voltaren 0.05 g 3 times a day, medintol 0.075 g 3 times a day - optional); xanthinol nicotinate 0.15 g 3 times a day (theonikol 0.3 g 2 times a day); prednisolone 15-30 mg per day (in cases of insufficient therapy effectiveness, with progression of the process). Sanitation of foci of infection is carried out. Dry heat, UHF, UV radiation, compresses with a 10% solution of ichthyol are prescribed locally.

