Medical expert of the article
New publications
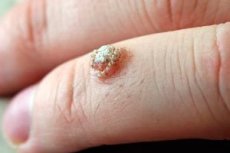
Dry warts on hands and feet
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Probably everyone has heard of such a benign formation as a dry wart. But few people know what causes its appearance and how to stop the growth and spread of the growth.
A dry wart is a hyperplastic area of epidermal tissue. Hyperplasia itself can be the result of the activity of a virus (HPV), which is usually contracted through direct contact with a sick person. The risk of infection is especially high if a person has microtraumas on the skin or a weakened general immune defense.
Epidemiology
According to statistics, at least 80% of adults have some karyotropic DNA viral cells in their bodies. However, the virus itself does not show up in everyone: a person can live peacefully with HPV and not even know about it for the rest of their life. The fact is that a dry wart appears on the skin only when certain favorable conditions for it are created in the body - for example, a sharp drop in immunity, intensive changes in hormone levels, an abundance of unhealthy habits, etc.
A dry wart can grow on both skin and mucous membranes. Its growth is often unpredictable: it is believed that it is very, very difficult, almost impossible, to “drive” the virus out of the body, but there are many known cases when the wart disappeared on its own. Scientists still cannot answer why this happens.
Both men and women have equal chances of becoming infected with the virus, so a dry wart can be found in anyone – and in any age category, even in children.
Most often, the growth appears on the limbs, especially on the hands and feet.
Causes dry wart
There is no single cause for dry warts. Of course, the main factor is the presence of a virus (HPV) - it is transmitted through direct contact with a sick person, or through contact with his personal items, or even from a carrier who does not show any signs of infection (even he himself does not know about its existence). HPV is the most common sexually transmitted infection (STI). 79 million Americans over the age of 20 are infected with HPV. [ 1 ]
The so-called “self-infection” is also possible; for example, a dry wart can appear after razor cuts or intensive peeling procedures.
Dry warts on the feet often appear as a result of abrasions of the skin by shoes, or against the background of other minor injuries. On the hands, growths often appear after frequent use of household chemicals, as well as with various microcracks received at work or during work, for example, in the garden.
Children can become infected with the papillomavirus by coming into contact with other children in kindergarten or at school, but the infection is often transmitted to a child from his mother during pregnancy or during childbirth.
Risk factors
Not everyone gets dry warts, even if they have the virus. It is estimated that up to 70% of sexually active women will become infected with the human papillomavirus (HPV), which causes warts, during their lifetime. [ 2 ] The following factors increase the risk of developing warts:
- Damage to the skin and mucous membranes: these can be scratches, cracks, ulcers, abrasions. The danger is that the papillomavirus can survive on surrounding objects for up to three hours, so it can easily get on the skin, and through damage - into the human bloodstream. Penetration of the virus becomes even more likely if the skin is moist, or, conversely, excessively dry and sensitive, chapped.
- High humidity combined with elevated air temperature: for example, when regularly wearing closed, un-dried shoes, especially those made of artificial materials, both dry warts and calluses can appear on the feet. The situation is worsened by a tendency to excessive sweating.
- Weak immune protection: with initially weak immunity, the virus gains additional opportunities to reproduce and spread. Immune protection weakens under the influence of poor nutrition, unhealthy lifestyle, hormonal changes, systematic lack of rest, and other infectious and inflammatory processes in the body.
Pathogenesis
The basic factor in the growth of dry warts is considered to be the HPV virus. The virus affects not only the skin, but also the mucous membranes in the mouth, nose, and genitourinary system. The virus belongs to the A-subgroup of the Papovaviridae family. The existence of more than seven dozen varieties of papillomavirus has been scientifically proven.
Infection is possible only through contact and everyday life: through handshakes, through the shared use of certain things, clothing, and toys.
When an infection gets on the skin, it begins to actively multiply if certain favorable conditions accompany it.
Self-infection is also not uncommon. For example, you can become infected through razor cuts, intensive peeling procedures, the habit of biting your nails, etc. The risk group includes people who regularly visit public baths and swimming pools, gyms, as well as those who work in meat processing plants, poultry farms, etc.
The minimum incubation period for HPV can be from six to twenty weeks. However, as we have already said, the disease does not always manifest itself externally, but proceeds hidden, asymptomatically. If dry warts do appear, they are found mainly on the extremities, less often on the face, neck, shoulders.
Symptoms dry wart
A dry wart looks like a dense and dry elevation above the skin surface. The size of the growth can vary, but usually does not exceed 4-8 mm. The most common localization of dry warts is the arms, legs (usually fingers, palms and feet), and face. The color range of the neoplasms also varies - from grayish-dirty to brownish-yellow or matte-flesh.
The first signs of wart formation also have their own characteristics. When the virus is activated, small papillary structures are formed on the skin. The epidermis layer in the affected area begins to keratinize. A warty growth is formed from the papillae, and a small network of vessels develops. With necrosis of some papillary structures, a dry rough surface is formed - this is a dry wart. Externally, it can have much in common with a callus, but inside there are rods with dark or reddish dots - roots.
After some time, the layer of skin above the papillae peels off, and the roots are exposed. The wart then continues to grow, and multiple growths located next to each other can merge. If such growths reach large sizes, they can cause discomfort, pain, or even periodically bleed.
- A dry wart on the foot and hands is considered the most common neoplasm. It can be superficial or deep: the latter option is usually accompanied by pain and has a small dry pit in the center. A superficial growth is characterized by hyperkeratosis. Dry warts in the foot area cause particular discomfort, since it becomes unpleasant for the patient to step on the affected limb. Since a wart of this localization is often mistaken for an ordinary callus, people seek medical help only in advanced cases, with large neoplasms.
- Dry warts on the body are found less often than on the hands and feet. However, their appearance is possible in the neck, armpits, chest and upper back. The problem occurs especially often in people prone to excessive sweating. Warts are usually uneven, hemispherical, with a yellowish or pinkish tint. The consistency of the growths varies from elastic-soft to dense, dry. The sizes also vary - from a couple of millimeters to 3 centimeters.
- A dry wart on the face is most often found in adolescence. Such a neoplasm is usually small and has a smooth (less often rough) surface. The color of the growth can blend with the skin tone, so in many cases a facial wart does not particularly attract the owner's attention. Patients often consult doctors when the problem is widespread.
Complications and consequences
The most likely complications of dry warts include the following:
- discomfort, itching and pain in the area of the growth;
- frequent damage to the protruding wart, associated bleeding, increased growth of the neoplasm;
- secondary infection, the penetration of microbes or fungal infection into the wound;
- expansion of the lesion, spread of warts throughout the limb and/or body;
- malignant transformation, malignancy of a wart.
Almost all of the above complications occur in advanced forms of pathological formations. Therefore, it is better not to wait for troubles to appear, but to start treating a dry wart at an early stage of development.
Diagnostics dry wart
Before referring a patient for removal of a dry wart, the doctor will definitely carry out the necessary diagnostic measures, since sometimes it can be difficult to distinguish a wart from other neoplasms.
If the doctor has even the slightest doubt about the origin of the growth, he will prescribe the necessary examinations and tests:
- Wart tissue scraping is used infrequently, but only in the case of bleeding, ulceration of the growth. The essence of the procedure is as follows: using a medical instrument, wart cells are "scraped" from the surface, transferred to a glass slide, and then sent for laboratory microscopic examination.
- A biopsy is the collection of biological material followed by histological analysis. Wart cells and tissues are collected with a needle or scalpel. The study allows one to evaluate the cellular composition of the material and rule out oncological disease.
- The polymerase chain reaction method is used to find out whether the papilloma virus is present in the body. The material for the study does not necessarily have to be taken directly from the wart: it can be blood, salivary secretion, etc. This method allows you to detect even the hidden existence of the virus in the body.
- Restriction endonucleosis DNA analysis, enzyme immunoassay, Digene test.
- Genetic amplification techniques combined with genotyping can identify specific HPV types. However, knowledge of the HPV genotype in benign warts does not influence the choice of therapy. [ 3 ]
Differential diagnosis
Differential diagnostics are mandatory, since it is important for the doctor to exclude other possible pathologies that are similar in manifestation to a dry wart.
What is the difference between a dry callus and a wart? What else should a dry wart be differentiated from?
Dry wart |
It has a dry, dense surface on which you can find barely noticeable dark spots - these are the capillaries that feed the neoplasm. A dry wart can cause not only discomfort: it can be quite painful, especially if it is located on the foot or palm. The wart is characterized by constant growth - both external and deep into the tissues. |
Dry callus |
It has a dense surface with a pronounced papillary pattern. Dark spots - capillaries - are absent. If you squeeze the callus from the transverse sides, then there will be no pain, but pressing from above can be quite painful. As a rule, a dry callus does not appear in a random place, but where there is constant or regular load, friction, pressure. |
Molluscum contagiosum |
The growths are skin formations with a diameter of one to eight millimeters. They are found mainly on the feet and genitals. Externally, the growth has much in common with a wart, but has a peculiar "crater" in the center, from which a curd-like liquid is released. |
Foreign body in the skin, splinter |
The appearance of a foreign body in the skin is characterized by an acute onset, squeezing the formation in any direction causes pain. As inflammation develops, the damaged area swells, turns red, and pus or serous fluid is released. |
Who to contact?
Treatment dry wart
There is currently no cure for HPV infection, and treatment does not affect transmission. [ 4 ] Therefore, current treatment is aimed at relieving signs and symptoms. No treatment is completely effective.
In 1995, the American Academy of Dermatology developed criteria for indications for treatment of warts [ 5 ], including:
- the patient's desire for therapy,
- symptoms of pain, bleeding, itching or burning,
- disabling or disfiguring lesions,
- a large number or large size of lesions,
- the patient's desire to prevent the spread of warts to unaffected skin, and
- a state of weakened immunity.
Treatment of a dry wart primarily involves its removal. This becomes possible thanks to a variety of surgical and medicinal means.
However, the answer to the question of how to remove a dry wart is given in each specific case by the doctor. Only he can decide which method is suitable for a particular patient - whether it will be surgical or chemical removal, or whether it is optimal to use other existing methods.
Any remedies for dry warts are used in combination - for example, the growth is cauterized and keratolytics are used at the same time. Treatment is often carried out with Solcoderm, Condyline, lactic acid solutions or silver nitrate.
To get rid of a viral infection, the doctor may prescribe oxolinic ointment, bromonaphthoquinone, etc.
The growth can be removed quickly using liquid nitrogen, electrocoagulation, or chemical agents – Feresol, acids (salicylic or trichloroacetic, etc.).
To strengthen the immune system, immunostimulants and vitamin complexes are prescribed, and after the removal procedure, anti-inflammatory therapy is relevant.
Dry Wart Remedies
Solcoderm |
An acid-containing solution that causes necrosis and mummification of wart tissue. The preparation acts only in the area of application. After treatment, the wart darkens, a scab forms, which falls off within a few days or weeks (depending on the size and depth of the growth). |
Condyline |
A podophyllotoxin preparation, has cytostatic and antimitotic properties. The solution is applied to the wart in the morning and evening for three days. If necessary, the course of treatment is repeated after 4 days. Possible side effects: redness and soreness in the area of application. |
Silver nitrate 10% |
The drug has a bactericidal and cauterizing effect, is used for application directly to the wart area, avoiding nearby healthy tissues. Side effects - mild discomfort at the site of application. |
Oxolinic ointment |
An external preparation with antiviral activity. The ointment is applied to the wart three times a day for several days or weeks, until the growth size is steadily reduced. The preparation is suitable for use in patients of different age categories and has virtually no contraindications or side effects. |
Feresol |
A cauterizing and bactericidal preparation based on phenol and tricresol. The product is applied precisely to the dry wart. Repeated treatment is possible a week after the scab has peeled off. Up to five procedures are allowed. A side effect is a burning sensation in the area of application. |
Glutaraldehyde is virucidal and is available as a 10% water-miscible gel or alcohol solution. Glutaraldehyde is usually applied twice daily and may stain the skin brown and cause contact sensitivity. 1 Treatment has been reported to be as effective as salicylic acid with cure rates greater than 70%. No randomized controlled trials have been published on the treatment of warts with glutaraldehyde.[ 6 ]
Formaldehyde is also virucidal and acts by destroying the top layer of epidermal cells and possibly damaging the virions. Available 0.7% gels or 3% solutions are used to soak trimmed plantar warts to speed resolution. Formaldehyde, widely used as a preservative in many products such as lotions and shampoos, can cause sensitization and should be avoided in patients with eczema and allergies.
One controlled trial of formaldehyde treatment for plantar warts included 192 patients with plantar warts. Cure rates ranged from 61% to 67% at 2 months but were not significantly different among four treatment groups: 3% formalin, 3% formalin, water (placebo), and sucrose (placebo).
Formic acid is a chemical irritant found in the bites and stings of many hymenoptera insects, including bees and ants, and was first isolated from red ants, hence the name from the Latin for "ant", formica. In a non-randomized, placebo-controlled, open-label study of 100 patients, the 85% ant/needle puncture technique of topical application resulted in a complete clearance of 92% compared with 6% in the placebo (water) group.[ 7 ] The mechanism of action of this agent is unknown.
Bleomycin, an antibiotic derived from Streptomyces verticillus, selectively affects squamous and reticuloendothelial tissues.[ 8 ] Five randomized controlled trials have assessed the efficacy of bleomycin;[ 9 ] however, it is difficult to compare trials. Cure rates ranged from 16% to 94%.
Dietary zinc has a profound effect on the human immune system, and deficiency results in decreased immune capacity. [ 10 ] Based on this, a placebo-controlled clinical trial was undertaken using oral zinc sulfate (10 mg/kg daily) for the treatment of recalcitrant warts. Complete clearance was noted in 87% of patients in the treatment group compared to no clearance in the placebo group. [ 11 ]
Fluorouracil has been used topically as an antiproliferative agent for warts.[ 12 ] In one prospective, placebo-controlled, single-blind, randomized study, up to 70% of warts regressed with treatment with 5-FU in combination with lidocaine to reduce pain and epinephrine to induce vasoconstriction to maintain high topical drug concentrations.[ 13 ]
Daily doses of 20 to 40 mg/kg of cimetidine, an H2 receptor antagonist, clear 82% of warts from skin in open-label studies.[ 14 ] Cimetidine is thought to act as an immunomodulator at high doses by inhibiting suppressor T cell function while increasing lymphocyte proliferation, thereby enhancing cellular immune responses.[ 15 ]
Imiquimod 5% cream is an immunomodulator that can stimulate cytokines including interferon-α, interleukin-1, interleukin-6, tumor necrosis factor-α, granulocyte-macrophage colony-stimulating factor, and granulocyte colony-stimulating factor. Absorption of imiquimod through intact skin is minimal. Its use in the treatment of external anogenital warts was approved by the US Federal Drug Administration in 1997 and has recently been approved for the treatment of nonhyperkeratotic, nonhypertrophic actin keratoses and superficial basal cell carcinomas.
The use of imiquimod for the treatment of nongenital warts has not been formally evaluated in a randomized controlled trial. However, in an open-label, uncontrolled trial using 5% imiquimod cream for the treatment of common cutaneous warts, patients applied 5% imiquimod cream to the warts once daily for five days a week and washed it off in the morning with soap and water.[ 16 ] Patients continued this treatment for 16 weeks or until the warts were completely cleared. Complete clearance of warts occurred in 30% of patients; 26% of patients experienced a reduction in wart size by >50%.
Antiviral drugs
Cidofovir is a nucleoside analogue of deoxycytidine monophosphate that inhibits DNA synthesis, causes DNA fragmentation, reduces epithelialization, and increases excoriation.[ 17 ] It has been used successfully in HIV-positive patients for the topical treatment of genital warts.[ 18 ]
Plaster for dry calluses and warts
The most common plaster for dry calluses and warts is considered to be Salipod. This is a well-known product, the basis of which is represented by salicylic acid, precipitated sulfur, rubber, lanolin, rosin, etc.
It is easy to use such a patch: a piece of the appropriate size is cut out and fixed on a previously steamed and dried wart. The patch is worn without removing for two days. If the wart remains in place after removal, the procedure is repeated. Usually after the second to fourth time the wart peels off and separates.
We remind you that removing warts on your own is dangerous. You should first consult a doctor.
Salicylic acid is the first-line therapy of choice for many patients because it is available over the counter. It is a keratolytic therapy with a mechanism of action that slowly destroys the virus-infected epidermis and may trigger an immune response from the mild irritation caused by salicylic acid.
Vitamins
Even if you have the papilloma virus in your body, you can prevent warts from appearing if you maintain your immunity at the proper level. And the first thing you need for this is a full supply of vitamins in your body.
What vitamins are most needed to prevent the spread of warts?
- Vitamin A is the immune system’s best helper in the fight against warts. Retinoids are also powerful immunomodulators. [ 19 ] There is some evidence that retinoids can suppress HPV transcription in affected cells. [ 20 ] Retinoids can be administered locally or systemically. It strengthens and enhances the body’s response to the introduction and activation of the papillomavirus. Vitamin A is present in sufficient quantities in carrots, bell peppers, grapes, parsley, and pumpkin.
- Vitamin E is always prescribed to solve various dermatological problems. Sufficient amounts of it can be obtained by eating seeds, nuts and vegetable oils. In addition, some experts advise treating dry warts directly with an oil solution of vitamin E: the solution should be applied three times a day for 2-3 weeks. Presumably, after such treatment, the growths should disappear on their own.
- Ascorbic acid is a well-known vitamin with antimicrobial, immunostimulating, and anti-inflammatory properties. Kiwi, citrus fruits, broccoli, and bell peppers contain a lot of vitamin C. These products should be included in the diet systematically, or the vitamin should be taken in a pharmacy version.
Additional enrichment of the body with vitamins increases the patient's chances of completely getting rid of dry warts. And as a "bonus" you can get a strengthening of the immune system, improvement of the skin, hair and nails.
Physiotherapy treatment
In addition to surgical methods, dry warts can be removed using physical procedures, such as:
- Medicinal electrophoresis with zinc has a keratolytic effect. For the procedure, 1-2% zinc chloride or sulfate is used. During the session, some pain occurs due to the cauterizing properties of zinc.
- Ultrasound treatment has much in common with radio wave therapy, but instead of radio waves, high-frequency sound is used. The dry wart is destroyed without causing unpleasant painful sensations.
- Alkaline baths are a great way to get rid of warts, especially if the growths are located on the body and in large quantities. The procedures are carried out daily or every other day for 3-4 weeks. For single warts, local baths are allowed.
- Simple sequential immersion treatments in hot water (45 to 48 °C) have been reported to significantly reduce the number of skin warts on the hands and feet.[ 21 ]
Physiotherapy treatment is prescribed by a doctor after diagnostic procedures: it is important to make sure that the warts are not malignant in origin and that the patient has no contraindications to such therapy.
Folk remedies
Many patients manage to get rid of warts forever using folk methods. Perhaps folk recipes will not immediately eliminate a dry wart, but with systematic use, many methods demonstrate a fairly good result. Of course, you should first consult a doctor.
- Take an apple, divide it into two parts using a thread. Rub the warts with the fruit parts, put the apple back and tie it with the same thread, bury it deep in the ground. It is believed that as the apple rots, the warts will disappear.
- Take a piece of dry ice, wrap it in a gauze napkin and apply it to the wart. Keep it there for as long as you can stand it. The growth should disappear after a few procedures.
- A clove of garlic is cut into two parts and used to rub a dry wart 2-3 times a day (before going to bed).
Garlic ( Allium sativum ) components have been shown to have antiviral activity and inhibit cell proliferation of virally infected cells.[ 22 ] In one placebo-controlled study, application of chloroform extracts of garlic resulted in complete disappearance of skin warts without recurrence after 3–4 months.[ 23 ]
- Prepare a garlic ointment. Grind garlic cloves into a paste, mix 1 teaspoon of this paste with the same amount of melted lard and 4 teaspoons of natural apple cider vinegar. Apply the mixture to the wart before going to bed, covering it with a bandage. Repeat the procedure daily until the growth falls off.
- Make a compress from grated unpeeled potatoes every day before bed for several weeks.
Herbal treatment
The most common plant that can rid a person of a dry wart is celandine. Its juice has an excellent cleansing effect. If you treat the growth with the yellow juice of the plant twice a day, then after a while the wart will fall off on its own. The duration of treatment depends on the size and depth of growth, so it can be from one week to 1-1.5 months.
Another effective plant is wormwood. Three tablespoons of dry crushed wormwood are poured with 500 ml of boiling water, and infused in a thermos for two hours. Use for compresses, which are repeated every day until the wart falls off.
In addition to the above methods, treatment with aloe is also successfully used. First, dissolve 1 teaspoon of baking soda in 200 ml of warm water. Moisten a small piece of cotton wool with the solution and apply it to the dry wart for 20 minutes. Then remove the cotton wool, and apply a small cut of an aloe leaf to the growth (with the cut on the wart), fix it with a plaster. Repeat the treatment daily until the neoplasm disappears.
Homeopathy
Dry warts are successfully treated with homeopathic remedies. In homeopathy, such neoplasms are considered a sign of impaired immune function, so the action of drugs is aimed at correcting immunity. As a result of such treatment, the body independently gets rid of pathological growths, without side effects and the risk of overdose.
The following homeopathic remedies are recognized as the most effective and reliable:
- Antimonium crudum - this remedy successfully fights various compactions and hyperkeratosis. Use potencies from 5 to 15 CH, 5 globules twice a day.
- Nitricum acidum can complement the treatment with the above preparation if a dry wart begins to bleed, becomes covered with cracks, and is accompanied by unpleasant stabbing sensations. Apply 1 tube of a standard dose, potency 7 or 9 CH daily.
- Causticum is prescribed for periungual and facial warts, in a potency of 7 CH 1-2 times a day.
- Dulcamara helps to get rid of warts on the wrist, as well as growths that occur in patients prone to obesity and excessive sweating. The recommended dose is 5 globules, potency 5 or 7 CH twice daily.
When using alternative treatments, it is important to remember that many warts will resolve spontaneously, with or without treatment.[ 24 ]
Surgical treatment
Any surgeon will offer his patient several methods of removing a dry wart. We are talking about the following procedures:
- The electrocoagulation method is suitable for getting rid of different types of warts. The procedure is performed under local anesthesia, using a special coagulator. Using high-frequency current and a metal loop instrument, the doctor carefully cuts off the growth, simultaneously coagulating the vessels, which helps to avoid bleeding. After cutting off the wart, a dense crust forms on the skin: it falls off in about a week. The scar after removal is not very pronounced, which, however, depends on the depth of wart growth. Using electrocoagulation followed by application of cidofovir gel, clearance was 100% with a relapse of 27%. [ 25 ]
- Surgical excision is used to remove large and deep warts. In essence, it is a regular mini-operation, using local anesthesia. The surgeon excises the wart with a scalpel and then applies stitches (they are removed after about 7-8 days). The wart removed in this way is usually sent for histological analysis.
- Laser removal involves the use of a laser beam that facilitates the evaporation and coagulation of epithelial cells. Local anesthesia is used during the procedure, and the removal itself is quick and painless. No stitches are required: after the manipulation, a small light dent remains on the skin, which smooths out and acquires a natural color after 2-3 weeks. No randomized controlled studies have been published on the effectiveness of the CO2 laser.
- The cryodestruction method involves deep freezing of the wart using liquid nitrogen. The most commonly used cryogen is liquid nitrogen with a temperature of -196° C. The effect of the procedure may not be immediately noticeable: the wart turns into a crust approximately one week after exposure, and falls off after another two weeks. In order for the removal to proceed without complications, it is important to strictly follow all the recommendations given by the attending physician. [ 26 ] Aggressive cryotherapy (10 seconds) is significantly more effective (cure rate 52%) than mild cryotherapy (short-term freezing) (cure rate 31%).
- Infrared coagulation. Direct application of infrared contact coagulators has been reported to be a cheaper, safer and more convenient alternative to CO2 laser treatment. The instrument allows for tissue necrosis control without tissue adhesion and results in remissions with a recurrence rate of 10.8%. [ 27 ] Compared to electrocoagulation, infrared coagulation produces similar results. [ 28 ]
- Photodynamic therapy. Instead of using endogenous target absorbers (i.e. water for the CO2 laser and oxyhemoglobin for the 585 nm pulsed dye laser), photodynamic therapy uses light of a wavelength absorbed by specific photosensitizing molecules that are exogenously introduced into the target tissue.[ 29 ] One widely used agent is 5-aminolaevulinic acid (ALA), which is a prodrug that stimulates porphyrin accumulation in tissue.[ 30 ] The porphyrins then act as a photosensitizing agent. When illuminated, the porphyrins induce a photooxidation cascade that damages the involved cells. ALA is applied topically as an ointment or cream and preferentially accumulates at the lesion site.
Prevention
You can reduce the likelihood of developing dry warts in the following ways:
- take care of your health, lead a healthy lifestyle;
- strengthen your immune system, eat right, toughen up, be physically active, avoid stressful situations;
- get rid of unhealthy habits, fully rest and recover;
- observe hygiene rules, avoid using other people's things;
- in places such as public baths and swimming pools, you should always have a change of shoes, towels, napkins, etc. with you;
- Any cuts or abrasions on the skin should always be treated with disinfectants, such as alcohol-containing lotions, chlorhexidine, etc.
You should be careful when choosing shoes and clothes. It is best to choose models made of natural materials, in accordance with the size and season.
Any skin problems should be treated by a doctor: self-medication can have negative consequences.
Forecast
When studying the effectiveness of treatment, it is necessary to take into account the spontaneous regression of warts. A dry wart can disappear on its own in some cases, without any external intervention. However, waiting for self-healing can take a long time, so in most cases doctors advise removing such growths. The prognosis is usually favorable, in about 20% of cases, a relapse of dry warts can be observed: as a rule, this is due to the presence of the papillomavirus in the body and the weakness of its own immune defense.

