Medical expert of the article
New publications
Diagnosis of astrocytoma of the brain
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
The problem of timely diagnosis and effective treatment of brain tumors is complicated by the late appeal of patients for help. How many rush to the doctor with a headache, especially if the symptom appeared not so long ago? And when vomiting joins the headache, the tumor often has already managed to increase significantly, especially if it is a malignant neoplasm. With small tumor sizes, there may be no constant symptoms at all.
In the early stages, brain disease may be detected by chance during a tomogram or X-ray examination. But such an examination also requires compelling reasons.
Regardless of whether the patient came to the appointment with complaints or the tumor was discovered during the examination, the doctor will be interested in the existing symptoms. First, the neurological status is assessed. This includes the presence of symptoms such as headaches, nausea, vomiting, dizziness, seizures. The doctor also studies the presence of general cerebral symptoms in the form of rapid fatigue, decreased cognitive abilities, as well as local symptoms that may change depending on the location of the tumor, and conducts a preliminary assessment of the degree of intracranial hypertension (fundus examination).
Clinical examination
During the physical examination, the general somatic status is assessed according to Karnovsky or the ECOG scale [ 1 ]. This is an assessment of a person's ability to lead a normal active life, to take care of themselves without outside help, the need for medical care, which is also used in the management of cancer patients. According to Karnovsky, an indicator of 0-10 indicates that the person is dying or already dead, with 20-40 points the person must be hospitalized, 50-70 points indicate the patient's incapacity for work and the possible need for medical care, 80-100 indicate normal activity with varying severity of disease symptoms.
If the patient is admitted to a medical facility in a serious condition, the consciousness is assessed using the Glasgow scale. Three main signs are assessed: opening of the eyes, speech activity, and motor response. The result is determined by the sum of points. The maximum number of points (15) indicates clear consciousness, 4-8 points are indicators corresponding to a coma, and 3 points indicate the death of the cerebral cortex.
Tests
Conventional tests, which are prescribed rather to assess the general condition of the patient's body and the presence of concomitant diseases, are not indicative of tumors. The changes in the clinical and biochemical blood tests are not specific, but they will serve as a guide when prescribing treatment. Additionally, the following studies may be prescribed (general urine analysis, analysis for HIV antibodies, the Wasserman reaction, determination of hepatitis B and C markers, tumor antigen). Since tumor treatment is usually associated with surgery, which may require a blood transfusion, a blood group and Rh factor analysis are considered mandatory. Molecular diagnostics of gliomas is also increasingly used in routine clinical practice [ 2 ], [ 3 ], [ 4 ]. A pilot project for early screening of brain astrocytomas using MRI scanning has also been launched [ 5 ].
A histological examination of the tumor sample taken during a biopsy is considered mandatory. But the problem is that it is not possible to take such a sample without surgery everywhere. Most often, a small area of the tumor is examined after its removal. Although modern medicine does not have new methods of minimally invasive biopsy at its disposal today (for example, stereotactic biopsy, performed in two ways), which are used based on the results of instrumental studies. [ 6 ]
Instrumental diagnostics
Instrumental diagnostics of brain tumors includes:
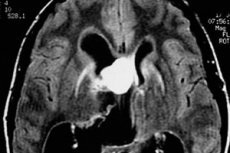
- Magnetic resonance imaging (MRI) or computed tomography (CT) of the brain. Preference is given to MRI, which is performed in 3 projections and 3 modes with and without contrast. If MRI is not possible, computed tomography is performed, including contrast. [ 7 ]
- Additional MRI capabilities:
- Diffusion MRI, which determines quantitative indicators of the diffusion of water molecules in brain tissue, thanks to which it is possible to assess the blood supply to the organ tissues, the presence of cerebral edema, and degenerative processes in it.
- Mo-perfusion of the brain, which allows to evaluate the characteristics of cerebral circulation and differentiate various pathologies. [ 8 ]
- MRI spectroscopy helps to assess metabolic processes in the brain and determines the exact boundaries of the tumor.
- Additional research:
- Positron emission tomography (PET) is an innovative method that allows detecting a tumor almost in its infancy. It can detect tumors of the smallest sizes. It is also used for differential diagnostics of recurrent glial tumors. [ 9 ], [ 10 ]
- Direct or CT angiography is a study of the brain vessels, which is prescribed if preliminary studies have revealed abundant blood supply to the tumor. Angiography also allows determining the extent of damage to the brain vessels.
- X-ray. This is not the most reliable method for diagnosing tumor processes, however, an X-ray of the spine can be a starting point for subsequent CT and MRI if the doctor notices a suspicious area on the image.
Additional methods for assessing the patient's health may include an electrocardiogram, electroencephalogram, ultrasound, organ radiography, broncho- and gastroduodenoscopy (in the presence of concomitant diseases), i.e. we are talking about a full comprehensive examination of the patient, which influences the choice of tumor treatment protocol.
Instrumental examination is recommended to be performed not only at the stage of disease diagnostics, but also in the postoperative period to assess the quality of the operation and prognosis of possible complications. In case of diffuse tumors that do not have a clear localization, as well as in case of deep neoplasms, the doctor acts practically by touch. Subsequent computed tomography, which is the standard of postoperative diagnostics, and the recommended MRI with and without contrast should be performed within the first 3 days after the operation.
Differential diagnosis of astrocytomas
Primary diagnostics of brain astrocytoma is complicated by the fact that the main symptoms of the pathology are also present in tumors of other etiologies, some organic diseases of the brain and even in somatic diseases. Only through a complete and thorough differential diagnostics can the exact cause of the symptoms be determined. [ 11 ]
Benign nodular astrocytoma on MRI most often appears as a homogeneous formation with clear boundaries (heterogeneity can be explained by the presence of calcifications and small cysts). With contrast, such tumors are enhanced in 40% (this is more typical for benign gemstocytic astrocytomas), while with the anaplastic form of astrocytoma, enhancement is always obvious.
Diffuse astrocytomas appear on the image as fuzzy spots without clearly visible boundaries. When such tumors become malignant, their structure changes and characteristic heterogeneity appears.
The difference between pilocytic astrocytoma and its other nodular varieties from glioblastoma and anaplastic astrocytoma can be determined by the following signs: the presence of clear boundaries and contours of the tumor in the first case, relatively slow tumor growth, the absence of cellular polymorphism, granules, a smaller tumor mass, and more or less uniform coloring of the pathological lesion on MRI. [ 12 ]
The main difference between diffuse astrocytomas and local tumors (nodular, focal) is the absence of clear boundaries of the neoplasm. The low degree of malignancy of the neoplasm is indicated by the comparative homogeneity of the internal structures of the tumor, the absence of foci of necrosis.
Anaplastic astrocytoma is a cross between low-grade diffuse astrocytomas and aggressive glioblastomas. It differs from ordinary diffuse astrocytomas in its cellular polymorphism (the presence of cells of various shapes, sizes, and dimensions in the tumor) and mitotic activity, i.e. the number of cells undergoing mitosis. Mitosis is a four-stage process of division of all cells in the body except for germ cells. [ 13 ]
Anaplastic astrocytoma is distinguished from glioblastomas by two factors: the absence of necrotic foci and signs of vascular proliferation. Only glial cells divide. The danger of this tumor is its rapid growth and the difficulty of determining the boundaries of localization. Glioblastoma not only grows extremely quickly (over several weeks and months), but also causes the death of brain cells, changes in the vessels of the head, completely disrupts the functioning of the organ, which leads to the death of the patient even in the case of treatment.
Great hopes in terms of differential diagnostics are placed on MRI of the brain [ 14 ]. Many factors are taken into account:
- frequency (glial tumors are detected in 1/3 of patients, of which almost half are astrocytomas of various localizations),
- the patient's age (children are more often diagnosed with low-malignancy astrocytomas, less often with the anaplastic variant of the tumor; in adults and the elderly, on the contrary, apaplastic astrocytoma and glioblastoma with a high probability of degeneration into cancer are more common),
- localization of the tumor (in children, the cerebellum and brainstem structures are most often affected, less often the tumor develops in the area of the optic nerve and chiasm, in adults, neoplasms usually form in the medulla of the cerebral hemispheres and the cerebral cortex),
- type of spread (for glioblastomas and low-differentiated astrocytomas, the spread of the process to the second hemisphere of the brain is considered characteristic).
- number of foci (multiple foci are typical for malignant tumors with metastases; sometimes glioblastoma manifests itself in this way),
- Internal structure of the tumor:
- 20% of astrocytomas are characterized by the presence of calcifications in the tumor, while tumors from oligodendroglia contain calcifications in almost 90% of cases (better determined by computed tomography)
- For glioblastomas and tumors with metastases, the characteristic feature is heterogeneity of structure, revealed by MRI.
- reaction to contrast (benign astrocytomas do not tend to accumulate contrast, unlike malignant ones),
- Diffusion MRI allows differentiating a tumor process in the brain from an abscess, epidermoid cyst, or stroke based on signal strength (it is weaker in tumors) [ 15 ]. A characteristic wedge-shaped spot is observed in stroke.
A biopsy helps differentiate an infectious process in the brain from a neoplastic (tumor) process, and determine the type of tumor cells. If open surgery is not possible or the tumor is located deep, a minimally invasive stereotactic biopsy is used, which helps, without opening the skull, to say how dangerous the tumor is in terms of malignancy.

