Medical expert of the article
New publications
Cranioplasty
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Cranioplasty is an operation to repair the skull damaged due to decompression interventions, depressed fractures, penetrating wounds and other traumatic and pathological processes.
Cranioplasty was first described in the 16th century: it was a method of replacing a bony cranial defect with a gold plate. Over time, the technique evolved, and gold was first replaced with celluloid and aluminum, then with platinum, silver and vitallium (cobalt-chromium alloy), tantalum, stainless steel and polyethylene. At present, the development of cranioplasty technologies continues: the choice of materials and techniques for performing the operation are being improved. [1]
Indications for the procedure
The main indication for cranioplasty is the presence of a defect in the skull. There are no restrictions on the boundaries of the lesion for which surgical intervention is indicated. For each specific case, the location of the defective area, cosmetic and aesthetic factors, the psychological state of the victim, the presence and features of combined neurological disorders are taken into account.
Depending on the timing of the intervention, cranioplasty can be primary, primary delayed (about 7 weeks after injury), and delayed (more than 3 months). Primary cranioplasty is preferred because it can be performed concurrently with intervention for the immediate brain injury or trauma. Often, cranioplasty is performed in conjunction with skin grafting, dura mater.
Reconstructive skin repair surgery is performed by excising scar tissue, relocating and replacing skin areas. If it is an extensive lesion, preliminary subcutaneous expansion implantation may be required.
If bony and cranial defects are combined with damage to the dura mater, plastic reconstructive cranioplasty is performed using autografts, allografts and xenografts. Parts of periosteum and aponeurosis are used as autografts, and synthetic membranes are more often the xenografts of choice. [2]
Preparation
When a patient is admitted to a neurosurgical or neuroresuscitation unit, the doctor performs a thorough clinical and neurological examination, using the Glasgow Coma Scale if necessary (speech, reaction to pain, eye opening in acute craniocerebral injuries are evaluated). Depending on the indications, the specialist finds out the mechanism of appearance of the skull defect, the extent of the lesion, the distribution. The use of computer visualization methods helps to better understand the pathophysiological features of the defect, identify primary and secondary brain damage, and preliminarily assess the specifics of cranioplasty. [3]
X-ray diagnostic method is used to assess damage to bony structures, penetrating wounds, detection of intracranial radiographic foreign bodies. However, CT scanning is preferred in this situation. CT scans are used to determine:
- Presence, location, and volume of hemorrhages;
- The presence and spread of cerebral edema;
- The presence, location, and structure of brain matter lesions;
- Possible displacement of the medial structures of the brain;
- The state of the liquor system and the cisterns, sulci and slits of the brain;
- Condition of the bones of the skull vault and skull base, types of fractures;
- The condition and internal contents of the sinuses;
- Soft tissue condition.
Repeat CT scans are ordered if neurologic problems worsen or intracranial pressure rises.
Magnetic resonance imaging is preferred when it comes to damage to brain structures adjacent to the bones of the skull vault and skull base. MRI can detect acute hypoxic or ischemic brain lesions, subacute and chronic hemorrhages, and differentiate between different types of cerebral edema.
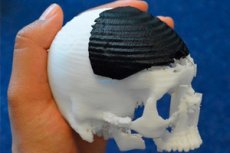
Modeling of the missing parts of the cranium is based on information obtained during preoperative diagnostic studies - in particular, computed tomography, craniography. The implant can be made by liquid monomer photopolymerization, using laser stereolithography (if the cranioplasty operation is not an emergency). This method is especially recommended if there is complex or multiple bone damage. The manufactured implants are finalized and "adjusted" directly during the cranioplasty process.
Technique of the cranioplasty
Before admission to the operating room, the patient is removed from the bandage, blood pressure is measured and examined. Position on the operating table: lying down, using a special cervical roll.
Cranioplasty is performed under endotracheal anesthesia or infiltration regional anesthesia with premedication with ataralgesia or neuroleptanalgesia and 0.5% novocaine hydrochloride (40 ml).
The cranioplasty operation itself begins with excision of the sheath-cerebral scar with minimal traumatization of the underlying brain tissue. The surgeon dissects the area of fusion of the scar with the boundaries of the bone defect. If allografts or autografts are used, or if hydroxyapatite compositions are used, the edges of the defective areas must be exposed. This will ensure optimal fusion of the implant with the cranial bones.
During cranioplastic modeling, the neurosurgeon tries to reproduce the shape of the missing segment as closely as possible. The formed element should not have protruding edges or sharp edges. Its installation is carried out clearly to the adjacent bones. [4]
It is important to take into account that when the temporal region is damaged, the muscle of the same name gradually atrophies. Therefore, even a complete coincidence of the inserted temporal bone element will not prevent the formation of a cosmetic flaw caused by soft tissue deformation. This problem can be solved by subsequent soft tissue contour plasty: in the area of atrophied muscles, the implant is made slightly thicker so that it protrudes above the surface of the cranial vault, with a soft transition of the place of adhesion of the inserted element to the bone.
The fabricated and modeled implants are placed and fixed along the boundaries of the lesion. Fixation of the element is mandatory, otherwise there is a risk of subsequent displacement.
Modern neurosurgery has access to a range of materials, techniques and methodologies for cranioplasty, allowing cranial lesions of virtually any configuration and size to be concealed, with a satisfactory aesthetic and functional result to follow.
At the end of the operation, drains are inserted into the postoperative wound zone in the interstitial space. They are removed on the 2nd day after the intervention. A bandage is applied.
The duration of operative cranioplasty varies within 3-4 hours. Postoperative stay of the patient in hospital is about 7-10 days. Sutures are removed on the 8th-10th day.
Cranioplasty of a skull defect
Today there is a possibility of using a variety of materials for cranioplasty. These are autografts, allografts, xenografts. Selection of the appropriate material is performed by a doctor, individually for each case. [5], [6]
In modern transplantology, it is considered that the material used must necessarily meet a number of requirements, among which are:
- Biocompatibility;
- Lack of carcinogenicity;
- Sterilization capabilities;
- Plasticity;
- The possibility of combining with stereolithography;
- Possibility of osteointegration - fusion with adjacent bone tissue without formation of connective tissue scars;
- Neuroimaging capability;
- Mechanical resistance;
- Low electrical and thermal conductivity;
- Adequate cost of production;
- Resistance to infection.
To date, there is no graft that meets all of these requirements. The only exception is autologous bone - the patient's native bone tissue. Therefore, it is important to preserve all elements of the bony skull, which allows further reconstructive intervention (reconstruction of the skull). This is often practiced when repairing a depressed fracture.
Cranioplasty of the skull with a titanium plate is reasonable for correction of depressed injuries with the use of bone sutures. A contraindication is considered to be brain bulging through the trepanation window and intensive infection of tissues in the area of injury. [7]
Autografts(from the Greek "autos" - own) are the most preferred. The autograft can be preserved during the primary intervention (decompression trepanation). The removed bone fragments are transplanted into the subcutaneous adipose tissue of the anterior abdominal wall, or into the anterointernal surface of the thigh. If the material was not saved during the primary intervention, or in case of a small bone defect, an autograft is used by splitting bone fragments (splitting the bone of the cranial vault with further implantation into the defective area).
An autoimplant can be made from a part of the rib or iliac bone. Among the disadvantages of this technique are: the appearance of a cosmetic defect in the area of material extraction, difficulties in forming the necessary area of the implant, and a high risk of resorption. However, this method is more recommended in pediatric practice, which is due to the maximum approximation of the chemical and plastic properties of the bone.
Aesthetic cranioplasty using alloimplants (from the Greek "allos" - another - that is, taken from another person) has a number of advantages:
- Uncomplicated processing of the material;
- Low risk of local complications;
- Acceptable aesthetic effect.
Among the disadvantages of this method are legal problems of biomaterial collection, the risk of transmission of specific infection.
Currently, the most common cranioplasty with an artificial bone substitute - so-called xenotransplantation (from the Greek "xenos" alien) - is considered the most common. Among the most popular xenografts are:
- Methyl methacrylates;
- Hydroxyapatite implants;
- Metal implants.
Methyl methacrylate cranioplasty
Methylmethacrylates are used in more than 70% of cranioplasty cases. [8] These implants offer a number of advantages:
- Easy to model;
- Can be easily adjusted to any size;
- Relatively affordable.
However, there are also "minuses": relatively high risks of postoperative complications. Local inflammatory process can develop due to allergenic and toxic effects of the active composition of methyl methacrylates, so they are used with special caution for cranioplasty in persons with a burdened immunoallergic anamnesis. [9], [10]
Cranioplasty with hydroxyapatite
The use of hydroxyapatite implants is possible in the form of pure hydroxyapatite cement if the defect size does not exceed 30 cm². If the size is larger, additional reinforcement with titanium mesh is performed. [11]
Cranioplasty with hydroxyapatite assumes almost complete biocompatibility, implants do not provoke antibody reactions or inflammatory-toxic reactions, they are not carcinogenic and do not affect the immune response. Small bone defects covered with hydroxyapatite are completely resorbed and replaced by bone tissue within a year and a half. If the defect is significant in size, the periphery of the implant is tightly fused with the tissue and partially resorbed, with stability of the central implanted area. [12]
Infectious postoperative complications are extremely rare (less than 3% of cases). Among the disadvantages:
- High production cost;
- Frequent need for additional reinforcement;
- Lack of possibility of cranioplasty with this material in the areas of the skull that carry a functional load.
Today there are hydroxyapatite bioceramic materials, which are manufactured by stereolithography. They are designed to cover large cranial defects and have a macro and microporous structure resembling the structure of human bone. [13]
Cranioplasty with metal and other implants
The use of metal systems in cranioplasty is becoming more and more common. Stainless steel, chromium, titanium and cobalt alloys, and pure titanium are actively used. The last option is the most optimal, as it has high biological compatibility, corrosion resistance, plasticity, and does not interfere with computer or magnetic resonance imaging. [14]
Contour cranioplasty can also be performed with implants produced by 3D technology, in particular by stereolithography. The element required to cover the cranial defect is reproduced layer by layer by depressive curing of liquid photomonomer using photopolymerization.
- The implant can be made based on a plastic model of the human skull. This is used to shape the required area by hand.
- It is possible to make a mold: first, the missing element is built on slices and contours, then the obtained information is transformed into a volumetric model.
3 D models cannot always be used. For example, in a number of acute brain injuries, cranioplasty surgery must be performed urgently, while the production of a stereolithographic element takes a relatively long time. [15]
Contraindications to the procedure
Cranioplasty is contraindicated:
- In acute combined craniocerebral injuries and cranio-maxillofacial injuries of severe nature;
- In decompensated cardiovascular pathologies;
- In blood diseases, hypercoagulable syndrome;
- Diseases or pathological conditions for which the use of certain medications or medical materials used in cranioplasty is contraindicated.
Among other contraindications: persistent increase in intracranial pressure, infectious processes in the soft tissues of the head, foreign bodies, as well as the general serious condition of the patient (if there are risks that the patient will not survive the operation).
Temporary contraindications are considered active purulent inflammatory processes, pneumonia, urinary infection. In such a situation, it is necessary to eliminate inflammation, after which there are no obstacles to cranioplasty.
Consequences after the procedure
Cranioplasty involves preventing the development of adverse effects caused by damage to the skull. The intervention can not only eliminate cosmetic imperfections, but also reduce the risk of severe neurological complications.
Meanwhile, the cranioplasty operation itself is a serious surgical intervention that requires a special approach and qualifications of neurosurgeons.
Possible complications after the procedure:
- Secondary infection;
- Implant rejection;
- Bleeding.
If the infection safety recommendations have been violated, infectious and inflammatory processes may develop during the first few days after cranioplasty. This development can be prevented by paying due attention to antiseptic treatment, ensuring the sterility of tissues and materials used.
Early postoperative period may be accompanied by accumulation of reactive effusion in the area of the skin-aponeurotic flap. In this situation, puncture and suction of exudate are performed.
Rarely, but rarely, implant displacement can occur if the implant is not properly secured. [16]
If infectious-inflammatory complications develop, the plate may be rejected against the background of the formation of purulent-inflammatory focus. If this happens, a second intervention is performed with removal of the implanted structure and intensive antibiotic therapy.
The likelihood of developing distant sequelae after cranioplasty depends on many factors, such as:
- From the characteristics of the injury (size, severity, combined lesions, etc.);
- The individual characteristics of the patient (age, general health status, past cranial injuries or surgeries, etc.);
- On the course of the early postoperative period, duration of coma, and the presence of seizures;
- On the quality of rehabilitation measures.
As a rule, the milder the injury and the younger the patient, the less often complications form and the less severe the consequences after cranioplasty.
Among the long-term consequences of surgery for severe cranial injuries are chronic progressive conditions accompanied by neurological symptoms (paresis, paralysis, coordination and speech disorders), mental and cognitive disorders, problems with liquor circulation, and failure of internal organs.
The most common psychiatric disorders after cranioplasty are considered to be depression, asthenic and neurotic disorders that require active psychotherapeutic support. Prevention of the development of such consequences lies in the timely detection and treatment of the initial signs of pathology. With the help of special tests, the quality of cognitive functions (attention, thinking activity, memory) is determined, and if necessary, treatment is carried out. In this way, it is possible to prevent the development of dementia, which in the active stage is virtually untreatable (it is only possible to slow the progression and alleviate some symptoms of the disease). [17]
Care after the procedure
After stabilization of vital functions of the organism at the stage of intensive care, early rehabilitation measures are started, the purpose of which is to prevent the development of complications after cranioplasty and prepare the organism for more active recovery measures.
The main rehabilitation is started after the acute postoperative period is over (i.e. At least 14 days after surgery). The start of such activities is determined by the attending physician. Continue rehabilitation measures as long as positive dynamics can be traced.
Rehabilitation is prescribed in courses of approximately 3 weeks. The frequency and number of such courses depend on the patient's condition. The most important results are those obtained during the first 6-12 months after cranioplasty.
In order to adequately assess recovery potential, additional studies are routinely performed:
- Blood tests;
- EKG, Holter monitoring;
- An MRI of the brain;
- Electroencephalography;
- Echocardiography, ultrasound examination of internal organs, ultrasound Doppler;
- Assessment of evoked potentials, electroneuromyography.
If necessary, consultations with a psychotherapist, psychiatrist, speech therapist, etc. Are carried out.
Recommendations for patients undergoing cranioplasty:
- Patients who have undergone cranioplasty surgery often have a range of physical, cognitive, psychological, and psychosocial problems that need to be considered when planning recovery interventions.
- The first time after cranioplasty surgery, the patient is not recommended to travel by airplane, allow significant physical exertion and pressure fluctuations.
If a patient is found to have neurologic deficits, they will need more time to recover. Cranioplasty usually involves long-term follow-up by a team of rehabilitation and neurological specialists, as well as physicians from other specialties.

