Medical expert of the article
New publications
Condylomatosis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
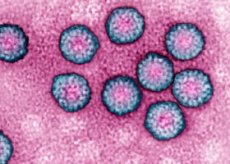
The common viral disease condylomatosis is caused by the papillomavirus infection. It can be classified as a sexually transmitted disease.
In the last decade, condylomatosis has become increasingly common: when diagnosed, it can be mistaken for another disease, so specialists assign a special role to differential diagnosis and prevention of this pathology.
Causes of condylomatosis
There are a large number of different varieties of papillomavirus, of which No. 6 and No. 4 are capable of causing condylomatosis.
The papillomavirus can be spread by contact. Most often, infection occurs sexually, including through oral or other contact with the genitals. However, contrary to some beliefs, infection through the use of a common toilet (toilet) is not possible.
Most patients with papillomavirus may not have clear manifestations of condylomatosis, but, meanwhile, they can be spreaders of the infection. Even a treated disease is not a guarantee that the sick person will stop spreading the virus. For this reason, all patients in adulthood should be considered as probable sources of spreading the virus.
If the patient has the virus but does not show any symptoms of the disease, the corresponding symptoms may appear within a month or a year. Unfortunately, as a result, it is not possible to accurately calculate the moment of infection.
The papillomavirus can enter the body even when using a condom during sexual intercourse. Of course, the chance of getting infected using a condom is much lower than without it. However, it still exists.
There are also known factors that facilitate the penetration of the virus into the body. These include:
- chronic diseases that have caused a weakening of the body's defenses;
- the use of certain medications, in particular chemotherapeutic drugs, as well as agents that suppress the immune system;
- deficiency of retinol and folic acid in the body;
- smoking;
- immunodeficiency states.
 [ 7 ]
[ 7 ]
Symptoms of condylomatosis
In men, condylomatosis is most often found in the area of the coronal groove of the penis, near the external opening of the urethra, on the inner layer of the preputial sac, or around the circumference of the anus.
Condylomatosis in women can be found in the area of the external genitalia, in the perineum and near the anus. If you are overweight, condylomas can be located in the folds of skin between the groin area and the thigh, as well as in the armpits, in the umbilical area, and along the lower part of the mammary glands.
Both men and women are almost equally susceptible to the disease. Condylomatosis is very rarely detected in childhood and old age.
The duration of the incubation period can vary from several weeks to several months (most often about 2 or 3 months).
The disease begins with the appearance of small, single, papillary villous growths that resemble pinkish nodules. Over time, the growths merge into groups, becoming similar to a chicken comb or a cauliflower inflorescence, located on a thin base (stem). Single growths are found only in some patients. In most cases, combined growths are observed, which sometimes merge, acquiring significant sizes. Often, this variant of the disease occurs in patients with obvious excess weight, or during pregnancy.
The growths eventually become bright red with a bluish tint, with signs of maceration and erosive elements. They can be painful to the touch and sometimes bleed. Serous-purulent discharge accumulates in the spaces between the nodules, which sooner or later begin to decompose and emit an unpleasant odor.
Neglected condylomas tend to become malignant, so timely diagnosis is an important step in the fight against the disease.
Diagnosis of condylomatosis
Condylomatosis has quite characteristic clinical symptoms, so a diagnosis can often be made based only on the results of an external examination, including an examination of the genitals.
In order to detect the growth of condylomas in the rectum, a consultation with a proctologist may be required, with a digital examination. Such an examination is carried out if the patient has condyloma nodules in the anal area.
In some cases, anoscopy may be used – an examination of the inner surface of the rectum using a special device.
In patients with acquired immunodeficiency, condyloma nodules can grow to significant sizes, forming accumulations that look like cauliflower inflorescences (Buschke-Loewenstein symptom). Such growths can at any time degenerate into squamous cell carcinoma. In order to exclude this degeneration, a histological analysis of the elements of the nodular growths is carried out.
If the doctor suspects the growths are malignant, the patient undergoes a rectoscopy. This procedure allows for an assessment of the intestinal walls to a depth of at least 30 cm from the anus.
Absolutely all patients with condylomatosis should be tested for HIV infection and RW (syphilis).
As a rule, the diagnosis is established based on the results of cytology and histology of the removed elements of condylomatous growths. In addition, enzyme immunoassay allows detecting antibodies to the papillomavirus in the blood. The removal of viral cell DNA from pathological tissue elements using the PCR diagnostic method may be prescribed.
You may also need to consult a venereologist or other specialist.
 [ 8 ]
[ 8 ]
What tests are needed?
Who to contact?
Treatment of condylomatosis
As a treatment for condylomatosis, diathermocoagulation is prescribed at the base of the growths, freezing with liquid nitrogen (the procedure lasts about 30 seconds, after which a disinfectant and drying agent is applied). If necessary, the procedure can be repeated.
One of the frequently used methods of treatment is the treatment of growths with an alcohol-containing solution of podophyllin (once a day for about 4 days). Podophyllin blocks the transport of intracellular nucleotides, thereby slowing down the reproduction of the virus in epithelial cells.
Resorcinol has cauterizing properties, in the form of a 50% solution or powder.
The following remedy also has a good effect: xeroform 5 g, resorcinol 5 g, tebrofen ointment 5% 10 g. Application of the mixture is combined with treatment of the affected area with novarsenol for 20-30 days.
A positive effect is observed from the introduction of interferon (one thousand units per 1 ml of water for injection) into the area of the base of the growths, as well as from lubrication with 5% fluorouracil.
If the growths are localized inside the urethra, fluorouracil is prescribed. It is allowed to use 1% bonafton, 0.5% colchamine, 5% tebrofen, 3% oxolinic ointment 2 to 3 times a day for 15-25 days.
In some cases, Feresol, a cauterizing bactericidal drug, is applied to the surface of the growths (in the base area). If necessary, the treatment is also carried out a week after the scab has fallen off.
A good effect is observed from applying the following combination of agents: 0.2 g prospiridine, 1 ml saline, 1 ml 0.1% adrenaline, 8 ml dimexide. This method of treatment can be used to treat condylomatosis during pregnancy.
The choice of treatment method largely depends on the stage of the disease. In some cases, the doctor has to resort to complex treatment, combining radical methods of removing growths with their subsequent medicinal destruction.
More information of the treatment
Prevention of condylomatosis
Specific prevention of condylomatosis consists of using the quadrivalent vaccine Gardasil, but this vaccine is effective only against some types of papillomavirus. This vaccine is in the development stage and can be further improved, creating protection in the body against other types of the virus. However, positive aspects are already observed when using this preventive vaccine, which allows us to hope for even greater effectiveness in the future.
Non-specific prevention should be based on maintaining hygiene of the skin and mucous membranes, especially around the urogenital area. All diseases of the external genitalia should be treated promptly and fully, abstaining from sexual contact until complete recovery.
Of great importance is the general strengthening of the immune system, proper nutrition, and giving up bad habits.
It is important to undergo regular medical check-ups and visit a doctor periodically, even if there are currently no clinical manifestations of any disease.
Prognosis of condylomatosis
Timely diagnosis and treatment of the disease play a major role in the positive prognosis of condylomatosis. Malignancy can be an extremely unpleasant consequence of condylomas in advanced stages. There is evidence of the degeneration of growths into warty malignant tumors, squamous cell carcinoma.
Patients with condylomatosis should be subject to dispensary control. The doctor monitors the general condition of patients, their response to the therapy, and dynamic indicators of recovery. Constant control by the doctor is also necessary to prevent relapse of the disease and to prevent malignant degeneration of growths.
Unfortunately, even after radical removal of the foci of the disease, the possibility of recurrence of condylomas remains. For this reason, methods of preventing relapses should be used constantly: for this, antiviral and immunomodulatory agents are used as prescribed by a doctor.
Condylomatosis is a disease that poses a certain danger to the body, so it is very important not to ignore the disease, but to pay as much attention to it as possible and follow all the doctor’s recommendations.

