Medical expert of the article
New publications
Chronic synovitis
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
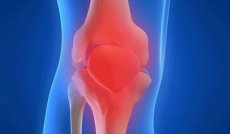
Chronic synovitis is one of the forms of the disease, which is characterized by an inflammatory process in the synovial membrane of the joints. Let's consider the main causes of the disease, symptoms, diagnostic methods, as well as methods of treatment, prevention and prognosis for recovery.
Chronic synovitis is diagnosed very rarely. Due to inflammation in the synovial membrane of the joint, effusion accumulates. Most often, this pathology occurs in the knee, ankle, wrist and carpal joints. The disease develops in one joint, but if it develops into polyarthritis, then both joints are affected.
The chronic form entails pathological changes in the joint capsule and blood composition. It is problematic to diagnose the disease at an early stage. To confirm chronic inflammation, a puncture is taken from the patient for examination, biochemical and a number of other studies are carried out. If therapy is not started in time, this increases the risk of sprains, dislocation or subluxation of the joint. In addition, the disease causes very unpleasant sensations when trying to bend an arm or leg in a joint that is inflamed, and external deformation also occurs.
Causes of chronic synovitis
The causes of chronic synovitis are varied and are divided into the following groups:
- Aseptic synovitis includes traumatic, neurological and endocrine disorder-related inflammatory processes.
- Infectious inflammation of the joints occurs due to the influence of pathogenic microorganisms (staphylococci, pneumococci, streptococci), which enter from the environment (through wounds, lymphogenous or hematogenous routes from infectious foci of the body).
- Allergic synovitis – occurs due to the action of allergens (infectious and non-infectious). The effect is directed at the tissues of the synovial membrane that are sensitive to irritants.
Let's look at the most common forms of synovitis and the reasons for their occurrence:
- Traumatic
Reaction to intra-articular injury. As a result of injury, effusion occurs in the synovial membrane. The disease can also appear without any apparent reason, as a result of irritation of the synovial membrane, due to a torn meniscus, instability of the joint, and other reasons.
- Acute traumatic
With this form of pathology, changes in the shape of the joint are observed within a few hours or days after the injury. There is an elevated temperature, limited movement, and pain during palpation. The patient suffers from general weakness and malaise. An untreated form of acute inflammation recurs, causing serious complications.
- Purulent
Causes a severe general condition: sharp pain, high temperature. The skin around the joint is smoothed, there is significant hyperemia and pain, movements are difficult. With this form, regional lymphadenitis may develop. With purulent synovitis, the inflammatory process spreads to the fibrous membrane of the joint, causing the development of purulent arthritis and damage to the surrounding tissues. If cartilage, ligamentous apparatus of the joint or bones are involved in the pathological process, this leads to panarthritis.
- Chronic
This form occurs rarely and is characterized by mild symptoms. Patients complain of limited movement in the affected joint, soreness, aching pain, rapid fatigue and tiredness when walking. Exudate accumulates in the joint cavity, which leads to hydrarthrosis (joint dropsy), with prolonged development, stretching and loosening of the ligaments occurs. Due to this, dislocation and subluxation may occur. Chronic synovitis is divided into serous-fibrinoid, vilous-hemorrhagic and vilous.
- Chronic villous synovitis
It is characterized by sclerotic and hypertrophied villi that become pinched off and form rice bodies and chondromous bodies.
Chronic forms of synovitis, regardless of the cause of their occurrence, are characterized by an increase in pathological changes, disruption of lymph and blood circulation in the joint capsule and its fibrous degeneration.
Symptoms of chronic synovitis
Symptoms of chronic synovitis are very similar to those of arthrosis. The disease causes visual changes in the shape of the joint, difficulty in movement and painful sensations. At the initial stage, the pathology causes swelling, which does not resolve due to constant irritation of the synovial capsule. Due to the inability of the joint elements to perform their functions, they begin to deteriorate. The patient develops a vascular network on the surface of the skin and constant painful sensations.
Acute synovitis is characterized by constantly increasing symptoms. The first sign of inflammation is an increase in the affected area in volume and the formation of swelling. The fluid inside the joint deforms its contours, which significantly complicates movement. Another pronounced symptom of the disease is inflammation of the internal membranes and pain syndrome. The pain is of medium intensity, but not sharp.
If the disease takes a purulent form, the symptoms are clearly expressed. The patient suffers from severe weakness, chills and malaise. Redness of the skin is observed in the area of the affected joint, and sharp pain occurs when trying to move.
Chronic synovitis of the knee joint
Chronic synovitis of the knee joint is an inflammatory disease affecting the synovial cavity of the knee. According to the time of the pathology, two forms are distinguished - acute and chronic, each of them has pronounced symptoms.
With chronic synovitis, painful sensations occur only during the period of exacerbation of the disease, and pathogenic exudate accumulates gradually. If the disease is secondary in nature, then this is reactive synovitis of the knee joint. This form is considered the most dangerous, since immediate treatment is required, but additional medication can significantly worsen the patient's condition. As a rule, it occurs against the background of allergic reactions or diseases such as gonarthrosis.
- Serous and serous-fibrinous – occurs due to prolonged and intense action of an irritant in the joint. The exudate has a yellow tint with characteristic fibrin flakes.
- Purulent – formed due to the impact of various microorganisms that penetrate the joint cavity. The danger of purulent synovitis is that the effusion can spread to other tissues and organs through the blood. This is why patients are often diagnosed with delirium, high temperature and general malaise.
- Hemorrhagic is another form of chronic synovitis, which refers to benign neoplasms of connective tissues of synovial bags, tendons and joints. Young women most often suffer from this pathology.
Where does it hurt?
Diagnosis of chronic synovitis
Diagnosis of chronic synovitis depends on the form and stage of the disease, the patient's age, the presence of concomitant diseases and other characteristics of the body. If synovitis is suspected, the following studies should be performed: cytology, arthroscopy, biopsy, synovial examination, arthopneumography and others. Diagnostic puncture is always used to confirm inflammation. The obtained materials are examined under a microscope and serological reactions are carried out. This is necessary to determine specific antibodies to a particular pathogen.
In addition to laboratory tests, special attention is paid to collecting anamnesis. The doctor asks the patient about the onset of the disease, symptoms and other features of the pathology. If chronic synovitis has arisen against the background of secondary inflammation, then diagnostics is aimed at identifying the underlying joint disease.
If the diagnosis of chronic synovitis has been confirmed, then first of all it is necessary to ensure complete rest and immobility of the joint. This will prevent further tissue injury. In addition, you can apply cold to eliminate swelling or a tight bandage. Depending on the severity of the disease, the doctor will prescribe treatment. All patients will receive drug therapy, wearing a knee brace or bandage, and in particularly difficult cases, surgery.
What do need to examine?
How to examine?
What tests are needed?
Who to contact?
Treatment of chronic synovitis
Treatment of chronic synovitis is a set of measures aimed at restoring the joint. If the disease is traumatic in nature, then first of all it is necessary to eliminate the damaged anatomical connections and correct the metabolic shifts in the joint. Depending on the severity of the damage and the nature of intra-articular changes, treatment can be conservative and surgical. If there are all indications for surgical intervention, then this is considered as the initial stage of treatment, followed by a long course of drug therapy and restoration of metabolic disorders of the joint.
- Among the primary measures for synovitis, the patient undergoes an early puncture of the joint with the collection of synovium for examination. After this, a splint or bandage is applied to the joint in order to immobilize it for 5-7 days and cold is regularly applied to relieve swelling. However, long-term immobilization is undesirable, as it can lead to complications such as joint stiffness.
- In case of frequently recurring inflammation, patients are prescribed medications to neutralize the factors causing synovitis. Most often prescribed are: Heparin, Indomethacin, Brufen, Glucocorticoids and others. On the 3-4th day of taking medications, the patient is prescribed physical methods of treatment: magnetic therapy, electrophoresis, UHF and others.
- In cases of protracted forms of chronic synovitis, for which conservative treatment has proven ineffective, surgical intervention is indicated. Since, most likely, irreversible changes in the synovial membrane of the joint occur: the formation of hypertrophied villi, sclerosis, or the formation of petrifications.
Surgical treatment of synovitis involves partial, subtotal or total synovectomy. The operation depends on the severity and spread of the inflammatory process. The operation is necessary for irreversible processes in the joints, for example, with the accumulation of calcium salt crystals. During the operation, an incision is made in the joint capsule and it is cleaned of various foreign bodies: deformed meniscus, cartilage fragments or salts. After the operation, a plaster cast is applied to the limb for a couple of days in order to immobilize it. The patient is prescribed antibiotics and anti-inflammatory drugs. But surgical treatment is used only when all possible methods of conservative therapy have proven ineffective.
Prevention of chronic synovitis
Prevention of chronic synovitis is carried out both after drug and surgical treatment. This helps prevent relapses of the disease and reduce the negative impact on the body. Thus, after surgery, the patient has a long period of rehabilitation. If the patient had chronic synovitis of the knee joint, then to restore normal functioning of the limb, a number of simple exercises are prescribed, which are initially performed under the supervision of a doctor.
- Walking – for a quicker recovery, it is recommended to walk at least 3-5 km daily at an average pace. This will speed up the process of joint recovery and improve overall health.
- Bicycle - to perform the exercise, you need to lie on your back, raise your legs up and make rotational movements (as when riding a bicycle).
- Squats - this exercise perfectly strengthens the ligaments and muscles of the joints, especially the knee joints.
- Running – short runs are recommended for patients who have successfully completed the above-described rehabilitation exercises. It is best to run in the morning; to maintain normal joint function, it is enough to run 1-2 km at an average pace every day.
Any general strengthening exercises can be performed only after permission from the attending physician. Such caution is entirely justified, therefore the decision on the need for preventive and restorative physical training is made only by the doctor.
Prevention should include measures to eliminate and prevent inflammatory processes in the joints. To reduce the risk of synovitis, it is necessary to promptly treat infectious diseases, lead a healthy and physically active lifestyle. Avoid joint damage, as this is the best prevention of synovitis. If pain or slight swelling appears after an injury, you should consult a doctor. Since without proper medical care, the injury can take the form of chronic synovitis.
Prognosis of chronic synovitis
The prognosis of chronic synovitis depends entirely on the condition of the body and the effectiveness of the treatment. Often, against the background of complete recovery, joint stiffness occurs. During the treatment of acute purulent synovitis, there is a high risk of sepsis, so the prognosis depends on the chosen treatment. Without timely medical care, the disease becomes chronic and causes a number of serious complications. Synovitis can cause purulent arthritis, periarthritis and phlegmon of soft tissues or panarthritis.
But with early diagnosis and successful treatment, chronic synovitis has a positive prognosis. By following all the recommendations of doctors and taking preventive measures, the patient has every chance of fully restoring the previously damaged joint.


 [
[