Medical expert of the article
New publications
Cavernous sinus thrombosis.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
If a vascular blockage by a thrombus occurs in the cavernous sinus area, located on the sides of the sella turcica, then we speak of cavernous sinus thrombosis. The pathology develops as a result of an inflammatory reaction - for example, with various infections. Cavernous sinus thrombosis is considered a rare disorder, and at the same time quite dangerous, since there is a significant risk of inflammation spreading to the area of brain structures. The disease is accompanied by a violation of blood circulation in the brain, and if medical care is not provided, the patient may die. [ 1 ]
Early recognition of cavernous sinus thrombosis, which often presents with fever, headache, visual disturbances such as periorbital edema, and ophthalmoplegia, is critical for a good outcome. Despite modern treatment with antibiotics and anticoagulants, the risk of long-term sequelae such as vision loss, diplopia, and stroke remains significant. [ 2 ], [ 3 ]
Epidemiology
Cavernous sinus thrombosis, as a pathology, has been known for quite a long time. The disease was described by several scientists of different times: in the 18th century, it was done by the Irish surgeon-anatomist William Dease, and in the 19th century, by the Scottish doctor, Professor Andrew Duncan.
The disease is considered rare: among adult patients, the prevalence is about 3-4 cases per million population, and among pediatric patients (children and adolescents) - about 7 cases per million.
Cavernous sinus thrombosis is most common among people aged 20-40 years, more often among women. [ 4 ]
Fatal outcomes occur in 5-25% of cases of the disease. [ 5 ]
Causes cavernous sinus thrombosis.
Cavernous sinus thrombosis always develops as a consequence of some other pathological process. In the origin of the disease, the primary source may be several disorders at the same time. Some experts believe that cavernous sinus thrombosis can also occur independently, but many scientists are confident that there is a provoking cause in all cases, it is just not always possible to determine it. [ 6 ]
A variety of infectious organisms may cause cavernous sinus thrombosis, although most are bacterial. Staphylococcus aureus may account for two-thirds of cases, and methicillin resistance should be considered. Other common organisms include Streptococcus species (approximately 20% of cases), pneumococci (5%), gram-negative species such as Proteus, Hemophilus, Pseudomonas, Fusobacterium, Bacteroides, and gram-positive species such as Corynebacterium and Actinomyces. Some of these (Bacteroides, Actinomyces, Fusobacterium) are anaerobic. Fungal infection in cavernous sinus thrombosis is less common but may include aspergillosis (most common), zygomycosis (eg, mucormycosis), or coccidioidomycosis in immunocompromised individuals. Rare factors that cause cavernous sinus thrombosis may include parasites such as toxoplasmosis, malaria, and trichinosis, as well as viral causes such as herpes simplex, cytomegalovirus, measles, and hepatitis.
Most often, the disease is associated with the following underlying causes:
- Infectious and inflammatory reactions – in particular, infectious lesions of the upper respiratory tract and organs of vision (orbital phlegmon, furuncle, retrobulbar abscess, various forms of otitis, sinusitis, meningoencephalitis, mastoiditis). In some cases, the "culprit" is acute respiratory viral infection, fungal infection, general blood poisoning.
- Non-infectious diseases of the central nervous system, which are accompanied by local damage to brain tissue and venous sinuses - in particular, after neurosurgical operations, traumatic brain injury, tumor processes (including metastatic).
- Hemodynamic disorders, venous system lesions – for example, severe dehydration, cardiac failure, antiphospholipid syndrome, prolonged catheterization with thrombus formation in the central venous vessel, thrombophlebitis of the head.
- Connective tissue pathologies (systemic lupus erythematosus, “dry” syndrome, systemic vasculitis).
- Hormonal imbalance, including that associated with long-term use of oral contraceptives, pregnancy, etc.
- Thrombophilia caused by congenital mutations or changes in the content of coagulation factor V, C and S-protein substances, prothrombin and antithrombin, homocysteine, as well as a deficiency of plasminogen or factor XIII. [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Risk factors
The following factors contribute to the development of cavernous sinus thrombosis:
- autoimmune processes in the body (systemic lupus erythematosus, rheumatoid arthritis, etc.);
- hereditary tendency to form blood clots in blood vessels;
- diabetes mellitus, especially its late stages;
- tumor formations of various etiologies in the sinusoidal zone of the brain;
- infectious and inflammatory pathologies in the face and head area (periodontitis, sinusitis, otitis, mesotympanitis, etc.);
- cardiovascular diseases (heart rhythm disorders, coronary heart disease, heart attacks);
- traumatic brain injuries that involve sinus entrapment. [ 11 ]
Pathogenesis
The development of cavernous sinus thrombosis is due to the anatomical features of the venous cerebral mechanism: the veins of the brain do not have a muscular wall and a valve system. In addition, cerebral veins are characterized by "branching". There are numerous anastomoses, and one venous vessel is capable of passing blood through itself, coming from several arterial pools.
The veins of the brain are superficial and deep, they flow into the sinuses of the dura mater. In this case, the superficial network flows mainly into the superior sagittal sinus, and the deep one - into the great vein of the brain and the straight sinus.
Cavernous sinus thrombosis develops by two mechanisms, which determine the clinical picture of the lesion. According to the first mechanism, cerebral venous vessels are blocked, which leads to cerebral edema and disruption of venous blood flow. The second stage is an increase in intracranial pressure as a result of blockage of large venous sinuses. In a healthy person, cerebrospinal fluid passes from the cerebral ventricles through the subarachnoid space of the lower and upper lateral surfaces of the cerebral hemispheres, is absorbed in the arachnoid plexuses and flows to the superior sagittal sinus. With cavernous sinus thrombosis, venous pressure increases: as a result, the flow of cerebrospinal fluid is upset, and an increase in intracranial pressure occurs. [ 12 ]
Symptoms cavernous sinus thrombosis.
The degree of manifestation of the clinical picture in cavernous sinus thrombosis varies, depending on the underlying cause of the pathology, the rate of increase in circulatory disorders, and the age and general health of the patient. [ 13 ]
In most patients, the first "alarm bell" is a headache: sharp or increasing, focal or diffuse, aching or periodic, sometimes with nausea (to the point of vomiting). The infectious form of thrombosis is accompanied by an increase in headache in the lying position (for example, at night), an increase in body temperature and other signs of intoxication.
The pathological picture of the eye is manifested by swelling, pain when pressing on the periorbital area, general painful sensations in the eyeball. Conjunctival edema, exophthalmos of varying intensity (usually bilateral) are noted. Patients complain of sudden blurred vision. [ 14 ] In some cases, venous cords in the upper eyelid can be palpated. The main external signs are: redness or cyanosis of the skin, swelling in the forehead and temples, cheeks and nasolabial triangle. A characteristic symptom is swelling of the mastoid process of the temporal bone.
General well-being may be impaired, from tinnitus to a comatose state. Some patients experience psychomotor agitation, which is especially characteristic of patients with heart attacks and strokes. Later, a focal neurological picture appears, represented by motor-sensitive aphasia, paresis and paralysis, convulsive attacks. [ 15 ], [ 16 ] Meningeal manifestations are observed less frequently.
The local neurological picture consists of drooping of the upper eyelid, limited motor control of the eyeball, and deterioration of superficial sensitivity in the area of innervation of the damaged nerves. In some cases, strabismus is observed.
Stages
In its course, cavernous sinus thrombosis goes through the stage of direct (first) and secondary (indirect) signs.
Early signs include:
- sudden deterioration of vision, even to the point of loss;
- protrusion of the eyeball forward, with subsequent displacement;
- swelling of the optic nerve and eyelids;
- intense pain in the neck, limited movement in this area;
- severe headache. [ 17 ], [ 18 ]
- Indirect signs may be the following:
- nausea to the point of vomiting;
- high body temperature;
- involuntary muscle twitching, mainly in the upper limbs and face;
- disturbances in thought processes, confusion. [ 19 ]
When indirect signs appear, there is a risk of developing a pre-comatose and comatose state. Therefore, at the second stage, it is extremely important to provide the patient with emergency medical care.
Forms
Pathogenetically, a distinction is made between aseptic (non-infectious) thrombosis of the cavernous sinus and infectious (septic) thrombosis. [ 20 ]
The aseptic form is encountered somewhat more frequently in clinical practice and is caused by:
- traumatic brain injury;
- complications during surgical (neurosurgical) interventions;
- tumor processes in the brain;
- obstruction of the internal jugular vein;
- complications of spinal and epidural anesthesia;
- hormonal imbalance;
- cardiac insufficiency, arrhythmia, heart defects;
- nephrotic syndrome; [ 21 ]
- severe dehydration;
- diseases of the blood coagulation mechanism;
- thrombophilia;
- liver diseases (cirrhosis), etc.
The infectious form, in turn, can be microbial, viral, fungal. Such pathology can be provoked by such disorders:
- intracranial abscesses;
- microbial, viral, fungal infections;
- parasitic diseases.
Complications and consequences
Cavernous sinus thrombosis can cause many complications. It is important to remember that the sooner the patient sees a doctor and begins treatment, the less likely it is that adverse effects will occur. Early effects include heart attack, cerebral edema, and focal seizures. [ 22 ] The most common long-term effects include:
- serous inflammation of the arachnoid membrane (arachnoiditis);
- deterioration of vision;
- anisocoria (pupils of different sizes);
- paralysis of the abducens nerve, which is responsible for contraction of the lateral rectus muscle, which is involved in the outward rotation of the eye;
- drooping eyelid;
- cerebrovascular accident, stroke;
- hormonal imbalances from the hypothalamic-pituitary mechanism. [ 23 ]
Cavernous sinus thrombosis in childhood is especially dangerous, as it can cause intellectual disabilities and various nervous disorders. Often, such deviations significantly affect the child’s future quality of life. [ 24 ], [ 25 ]
The mortality rate due to cavernous sinus thrombosis is approximately 20%.
The likelihood of recurrent thrombosis depends on many factors, in particular, on the completeness of the recovery period and on compliance with all medical recommendations. The rehabilitation period is usually long and lasts for several months. After completion of the main course of treatment and the patient's transfer to outpatient treatment, it is important to observe maximum rest, not to burden the body with physical activity, not to overeat, not to smoke [ 26 ] and not to drink alcohol. Medication support at this stage is prescribed by the doctor on an individual basis. [ 27 ]
Diagnostics cavernous sinus thrombosis.
The diagnosis of cavernous sinus thrombosis can be called difficult - primarily due to the lack of specific signs of pathology. Often, differential diagnostics are put first, and the presumptive diagnosis is made by excluding other possible pathologies.
The diagnostic scheme for suspected cavernous sinus thrombosis consists of the following procedures:
- Collection of information about the disease, examination and questioning of the patient. The initial questioning is conducted by a neurologist: he carefully studies the complaints, specifies the time of the appearance of unpleasant symptoms, finds out the presence of other symptoms and concomitant pathologies. After this, he performs physical diagnostics to determine the external signs of the disorder.
- Checking the neurological status. Many patients with cavernous sinus thrombosis experience suppressed pupillary and corneal reflexes, decreased or lost sensitivity in the eyelid area, forward displacement of the eyeball (bulging), paralysis of the eye muscles, and strabismus. The spread of the inflammatory process to the structures of the brain manifests itself in bulbar disorders, central paresis and paralysis, and positive meningeal signs.
- Examination by an ophthalmologist. During the examination, severe conjunctival edema and loss of visual fields in the form of partial blindness (hemianopsia) are sometimes detected. The ophthalmologist determines unclear contours of the optic disc and dilated veins of the fundus. [ 28 ]
Next, the patient takes the following laboratory tests:
- general blood test (cavernous sinus thrombosis is characterized by neutrophilic leukocytosis, increased ESR, low hemoglobin levels, moderate lymphopenia, and less commonly, thrombocytopenia);
- general urine analysis;
- examination of cerebrospinal fluid (in case of cavernous sinus thrombosis, an elevated protein level, the presence of blood cells is observed, less often - the cerebrospinal fluid is unchanged).
Instrumental diagnostics are most often represented by X-rays, [ 29 ] computed tomography and magnetic resonance imaging. [ 30 ]
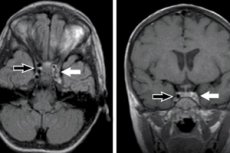
MRI in T1 mode visualizes the thrombus as a zone with the intensity of the brain parenchyma, and in T2 mode - as a hypointense zone. In the subacute course, all modes demonstrate an increase in the magnetic resonance signal in the thrombosed area. [ 31 ]
Cavernous sinus thrombosis appears as a high-density area on CT. Hepodense foci, narrowed cerebral cisterns and ventricles are detected. With the use of contrast imaging, a cavernous sinus thrombus is visible, as well as the “empty delta” symptom, characterized by the absence of contrast accumulation in the occluded area of the venous sinus. [ 32 ], [ 33 ]
Differential diagnosis
If cavernous sinus thrombosis is suspected, differential diagnosis with general and ophthalmological diseases is required, in particular, with the following:
- A septic condition that occurs regardless of the primary focus. The patient is examined for bacteremia.
- Thrombosis of the sigmoid sinus, which becomes a complication of otogenic diseases.
- Thrombophlebitis of the cerebral venous vessels, with typical repeated intultic-like attacks, migration of focal lesions, rapid disappearance of neurological symptoms. Also characteristic are sharp headaches, vomiting, bradycardia, congestion of the optic nerve discs, spinal hypertension with local convulsive attacks.
- Orbital pathologies, including orbital phlegmon, retrobulbar hemorrhage, sarcoma and other disorders accompanied by exophthalmos. The presence of infection and neurological signs indicate cavernous sinus thrombosis. With swelling and pain in the eye area, decreased vision, orbital phlegmon can be suspected. Additionally, X-ray diagnostics are performed.
A typical sign of cavernous sinus thrombophlebitis is bilateral exophthalmos with immobility of the eyeballs.
Who to contact?
Treatment cavernous sinus thrombosis.
Treatment procedures for cavernous sinus thrombosis may vary, depending on the patient's age, the intensity of pathological manifestations, and the underlying cause of the disease. If drug therapy is ineffective, surgery is prescribed with subsequent rehabilitation measures. [ 34 ]
The main focus of treatment is to restore the patency of the cavernous sinus. There are known cases of successful use of thrombolysis, but against its background the risk of hemorrhage development increases significantly. Today, anticoagulants are the first line of treatment – for example, low molecular weight heparins. [ 35 ] As experts point out, the use of direct anticoagulants at the acute stage of thrombosis significantly optimizes the prognosis and reduces the percentage of mortality and disability among patients. [ 36 ]
In case of infection-induced thrombosis of the cavernous sinus, antibiotic therapy is prescribed in high doses, using drugs with broad antibacterial activity - in particular, cephalosporins:
- Ceftriaxone in the amount of 2 g per day as an intravenous infusion;
- Meropenem, Ceftazidine 6 g per day as intravenous infusions;
- Vancomycin 2 g per day intravenously.
It is imperative to examine and act on the primary infectious focus: if necessary, resort to surgical assistance (the operation should not precede antibiotic therapy). [ 37 ]
After the acute stage of cavernous sinus thrombosis, indirect oral anticoagulants (Warfarin, Acenocoumarol) are prescribed, with a focus on INR in the range of 2-3. Direct anticoagulants should be used until such indicators of the international normalized ratio are achieved. [ 38 ]
In the aseptic form of pathology, heparin is used in the amount of 2.5-5 thousand units in the form of intravenous or subcutaneous injections. The dosage is gradually increased to 70 thousand units per day. The therapy is continued until positive symptomatic dynamics are achieved.
In addition to the main treatment, measures are taken to prevent the development of complications - for example, seizures or increased intracranial pressure. For this purpose, anticonvulsants are used, artificial ventilation of the lungs is performed (hyperventilation with (+) pressure on exhalation), osmotic diuretics are prescribed. When taking diuretics, it should be taken into account that excessive fluid excretion can negatively affect the rheological properties of the blood, which can aggravate the formation of blood clots. [ 39 ]
In some cases, particularly in cerebral edema, glucocorticoids are used, although their effectiveness remains questionable.
In particularly severe cases of cavernous sinus thrombosis, with compression of brain structures, decompression in the form of hemicraniotomy is performed according to indications. [ 40 ]
Prevention
The main point of cavernous sinus thrombosis prevention is timely treatment of any infectious and inflammatory processes in the body, and especially those that affect the respiratory system. People with frequent respiratory diseases, chronic pathologies of the respiratory system should visit the attending physician for preventive purposes at least once every 6 months.
It is necessary to take measures to strengthen the vascular wall. It is important to eat healthy natural food, drink enough liquid daily, periodically take multivitamins at the discretion of the doctor.
One of the factors that provoke thrombosis is infectious processes in the body. In particular, viral, bacterial and fungal infections can become dangerous. When the disease develops, it is important to undergo timely and complete treatment, following all the doctor's recommendations. In no case should you stop treatment without completing it, and even more so - independently prescribe and cancel medications, change the dosages prescribed by the doctor.
Forecast
The most favorable prognosis is observed in cases of cavernous sinus thrombosis detected at early stages of development, provided that proper and timely treatment is provided. Drug therapy allows stopping the inflammatory process, eliminating the thrombus and restoring normal blood circulation. Late diagnosis requires more serious treatment measures. [ 41 ]
The most common complications of thrombosis are infarctions and cerebral hemorrhages, cerebral edema. Such problems occur in approximately every second patient. Among the rarer complications, one can name epileptic status, pulmonary embolism. As a result of infectious inflammation, abscesses (including liver, lungs, brain), purulent meningitis, inflammatory processes in the lungs sometimes develop. [ 42 ], [ 43 ]
Cavernous sinus thrombosis is also dangerous because the pathological focus is located in close proximity to the structures of the brain. This is why it is important to seek medical help as soon as possible to prevent the spread of the inflammatory reaction to brain tissue and blood vessels. [ 44 ] Timely diagnosis and treatment will help restore health and prevent the development of adverse complications.

