Medical expert of the article
New publications
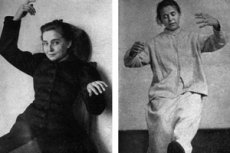
Catatonic excitement
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
One of the manifestations of acute psychosis is agitation - excessive and inadequate motor activity, expressed to varying degrees: from excessive fussiness and verbosity to destructive impulsive actions. In this case, the patient has a pronounced disturbance of affect. Catatonic agitation is a type of hyperkinetic acute psychosis with specific manifestations: motor restlessness is characterized by chaos, lack of purposefulness, stereotypical, sometimes fanciful, movements, meaningless and incoherent speech. In severe cases of catatonic agitation, speech is absent. Characteristic is sudden and unmotivated rage directed at others, autoaggression, when the patient poses a real danger to himself and others.
Any manifestation of catatonia - both stupor and excitement - is considered an indicator of the severity of a mental disorder.
Epidemiology
Statistics on the incidence of catatonia are unknown, as this condition develops in completely different diseases. Research data varies greatly.
It is only known that in psychiatric hospitals there are one or two patients with catatonic syndrome for every 10 patients. Among schizophrenics, catatonic symptoms are observed less frequently than in every tenth patient. Although catatonia is associated with schizophrenia, this syndrome is three times more common in autistics, and 9-10 times more common in mood disorders. [ 1 ]
Causes Catatonic excitement
Catatonic agitation is one of the manifestations of the syndrome, the name of which comes from the ancient Greek word catatonia, meaning a tense, stressed state. Currently, it is not considered an independent disease, since the development of the syndrome is observed in various mental disorders, neurological and physical (somatic) diseases, intoxications and brain injuries. It is believed that the symptoms of catatonia indicate the severity of the patient's condition.
For a long time it was associated mainly with schizophrenia. Modern psychiatry recognizes that the development of the syndrome is possible and even more likely with other mental disorders. It has already been established that catatonic excitement occurs much more often in cases of affective disorders, especially mania, and is a consequence of the neurotoxic effect of certain substances: psychotropic drugs - neuroleptics, anticonvulsants and dopaminergic agents, benzodiazepines; drugs of other groups - glucocorticosteroids, the antibiotic ciprofloxacin, less often - others. Catatonia is often manifested by drug intoxication with opiates, cocaine, amphetamines; poisoning with carbon monoxide or exhaust gas. The new ICD-11 classifier assigns separate codes to the most common cases of catatonia: caused by mental pathologies, psychoactive substances, including drugs, and secondary catatonia in severe forms of neurological and physical diseases.
Risk factors
Risk factors for the development of catatonic agitation are listed in the diseases and conditions in which the development of catatonic syndrome was observed, the so-called "catatonic spectrum". This does not mean that the symptoms of catatonia cannot manifest themselves in other cases; quite rarely, their causes remain unidentified, and then the patient is diagnosed with idiopathic catatonia.
Mental disorders in which catatonic agitation most often develops include: mood disorders (especially manic), schizophrenic and autistic spectrum disorders; mental status disorders after trauma and childbirth; hysteria. Catatonic agitation is also typical for children with mental retardation and developmental disorders. [ 2 ]
The spectrum of neurological diseases in which this symptom complex develops includes uncontrolled tics (Tourette's syndrome), epilepsy, consequences of encephalitis, stroke, traumatic brain injury, neoplasms and other lesions of cerebral structures (basal nuclei, thalamus, frontal and parietal zones of the cerebral cortex).
Organ pathologies and conditions that trigger the pathogenesis of catatonic agitation are varied. Almost any somatic disease occurring in a severe form can lead to complications - disorders of neurochemical processes in the structures of the brain, leading to increased activity of excitatory neurotransmitters. The list of diseases of the catatonic spectrum includes acute and chronic cerebral circulatory disorders, endocrinopathies and autoimmune processes leading to metabolic disorders, vitamin deficiencies, in particular cyanocobalamin, mineral substances, for example, sodium deficiency, surpluses of adrenaline, thyroid hormones, calcium. Risk factors that increase the likelihood of developing psychomotor agitation include severe viral and bacterial infections, complications of decompensated diabetes mellitus (ketoacidosis), severe renal and hepatic failure, any conditions leading to hypoxia, heat stroke. [ 3 ]
Pathogenesis
There are many theories regarding the mechanism of development of catatonic excitation, but all of them are still in the realm of speculation. It is obvious that excitatory neurotransmitters are activated and inhibitory ones are suppressed, which leads to the development of specific psychomotor symptoms. Motor disorders are attempted to be explained by disturbances in neurotransmitter exchange in the basal nuclei, in particular, by suppression of the activity of γ-aminobutyric acid. This assumption is based on the pronounced effectiveness of drugs of the benzodiazepine group, which increase the activity of this mediator. Hypothetically, hyperactivity of the glutamatergic system may also underlie catatonic excitation.
The ineffectiveness of neuroleptics in the state of catatonic agitation gave rise to the hypothesis that it is caused by a massive blockade of the dopaminergic system. These drugs, which block dopamine receptors, successfully stop psychomotor agitation of other genesis, however, in cases of catatonia they can worsen the patient's condition, which is explained by a double effect - the effect of the drug is superimposed on an acute dopamine deficiency caused by metabolic disorders. [ 4 ]
The catatonic excitement that occurs after discontinuation of clozapine, which blocks cholinergic and serotonin receptors, is thought to be due to a surge in the activity of these systems.
In patients with chronic catatonia with mutism, tomograms showed bilateral disturbances in neurotransmitter metabolism in the thalamic zone and frontal lobes of the brain.
Catatonic agitation is not considered separately. In the syndrome of the same name, it usually alternates with a state of stupor.
Symptoms Catatonic excitement
Catatonic agitation, according to the observations of outstanding Soviet psychiatrists A. V. Snezhnevsky, O. V. Kerbikov and many other authors, develops in stages. One type turns into another, more complex one.
The first signs appear as a confused and pathetic excitement. During this period, the patient performs many very expressive actions that can be characterized as reactions to external stimuli, and they do not make sense, but the objects are used for their intended purpose. For example, patients open and close doors and windows, but situationally this action is devoid of reason; postage stamps are glued, but not to envelopes, but to the wall or to their forehead. At this stage, the patient practically does not close his mouth, his statements are meaningless, torn, enthusiastically pathetic. Patients often sing or heartfeltly recite poetry, the actions resemble a "one-man show" that greatly overacts. At the same time, the patient himself is noticeably confused, as if he cannot remember or figure something out. He can examine and feel objects that fall into his field of vision, throw them or snatch them from the hands of others.
Then the excitement increases and symptoms of hebephrenia join in – grimacing, unmotivated joy, childishness, silly, ridiculous behavior, causeless laughter, dancing. Impulsive actions and exaltation are possible. At this stage, the patient is still conscious, but he can already show sudden and strong rage. [ 5 ]
As the symptoms increase, a period of impulsive actions begins, which are very aggressive in nature, dangerous for the patient himself, since his aggression is often directed at himself. He can grab objects nearby, throw them at windows, at standing people, snatch objects from the hands of others, try to run somewhere, hit someone. The patient's speech consists of shouts, he often repeats phrases or individual words after others, their actions, gestures and poses. At this point, the patient also poses a serious danger to others. He can start breaking mirrors, glass in windows or doors, grab and throw improvised objects at others, jump from a high floor, etc. [ 6 ]
Then comes the most severe phase – silent excitement (the highest degree of impulsivity), when the patient silently and furiously commits destructive, senseless actions, and furiously resists attempts at verbal and physical influence to stop him. The rhythmicity of the patient's movements is characteristic, reminiscent of choreic hyperkinesis or St. Vitus's dance.
Not all psychiatrists agree with this syndromekinesis. Some believe that the impulsive and even mute stage can occur without a preliminary confused-pathetic phase. Although, perhaps, it simply passed unnoticed. Catatonic excitement can also end at the first or second stage, especially if the patient is given timely medical assistance. It can proceed quite moderately or be very intense, but in any case, the patient does not remain at rest for a second. Periods of excitement at any stage can be replaced by periods of stupor (substupor), when the patient freezes and falls silent. [ 7 ]
Catatonic agitation is an increase in psychomotor activity with clinical manifestations characteristic of catatonia: echo effects - repetition of words and phrases after others (echolalia), facial expressions (echomimia), movements and actions (echopraxia); negativism - active or passive resistance to external influences; passive subordination; waxy flexibility (cataleptic manifestations); various stereotypes - motor, speech, etc.
Catatonic excitement can occur with clouding of consciousness (oneiroid form) or without it (lucid). Hebephrenic, ecstatic excitement can occur in two forms, impulsive and silent - in the oneiroid.
In the prodrome and initial stage of catatonic excitement, distinct symptoms of autonomic disorders are observed - changes in pupil size (alternating miosis and mydriasis) and skeletal muscle tone, arrhythmia and tachycardia. The patient's face becomes pale and suddenly red, sweating - dry skin. Laboratory tests may show hyper/hypoglycemia, slight leukocytosis, azotemia, and during wakefulness. Blood pressure surges are also observed. This complex of somatic symptoms is called compensation syndrome.
In the clinical picture of lethal catatonia, the excitation stage occurs first. Catatonic excitation itself is not classified as malignant catatonia, but it can progress to the final stage – stupor. An alarming symptom is hyperthermia and the following manifestations: a constant and continuous increase in symptoms with an impressive increase in physical capabilities is characteristic, which leads to destructive consequences, rhythmic movements, logorrhea. The patient's arms and legs are icy and wet, the skin on them is bluish. Rapidly yellowing bruises appear on the body at the sites of blows and pressure. At the moment of excitation, the patient's blood pressure and body temperature rise (to hyperpyretic values with cold extremities). When the patient becomes exhausted and blood pressure and temperature begin to decrease, excitation turns into stupor. Without treatment, death occurs. [ 8 ] Postmortem studies do not reveal physiological changes indicating the cause of the patient's death. [ 9 ]
Catatonic agitation in children
Psychotic states in childhood most often manifest themselves in speech-motor disorders similar to catatonic agitation. It is difficult to confidently diagnose schizophrenia in three- to four-year-old children, identifying delusional ideas or hallucinations. Therefore, most studies note that at an early age, catatonic agitation develops with organic brain damage and exogenous psychoses, as well as with severe oligophrenia. Such manifestations as stereotypes, rhythmic repetitive movements and cries, silliness, echo effects, waxy flexibility, mutism are characteristic.
Catatonic syndrome in children, especially at an early age, is most often manifested by excitement. Although there are descriptions of substuporous states and stupor, especially in autistics, when parents note that their children are becoming slower and slower.
At an older age (after 10 years), catatonic excitement in children often precedes rapid degradation and a state of emotional dullness during the development of juvenile malignant schizophrenia. Catatonic disorders are more common than hebephrenia. In their development, they go through a phase of melancholic mood, manic, catatonic excitement, clouded consciousness and an outcome in the final defective phase.
Catatonic agitation in children is most often manifested by impulsive running, aimless movement from one object to another, stereotypical movements, impulsive urges, running away, throwing away or damaging objects. Over time, children's speech regresses and a profound mental defect develops.
Catatonic syndrome is rare in children, so samples usually include a small number of pediatric patients. The authors note that in the premorbid period, there are disorders of drives, and after 4 years - depletion of emotions, monotonous games and catatonic agitation. Akinetic disorders (stupor) are not typical for children. Although the general symptoms in children and adults are almost the same. Small children mainly make monotonous repetitive movements: running in circles, banging their heads on the floor or wall, fiddling with clothes, biting their nails. In older age, symptoms of choreic hyperkinesis, mannerisms, grimacing, negativism and mutism appear. [ 10 ]
In general, there is currently insufficient information about catatonic syndrome in children; there are no clear descriptions of the characteristics of speech motor disorders in terms of age, that is, they are very ambiguous.
Complications and consequences
Catatonic agitation is a sign of a severe course of various disease states that require special measures for care and treatment. It can threaten the health and life of both the patient and the people in direct contact with him. Patients with clouded consciousness are especially dangerous, contact with whom is difficult. Their impulsive actions are almost impossible to predict. [ 11 ]
At the first signs of its development, it is necessary to seek emergency specialized psychiatric help. Patients in a state of catatonic agitation are usually hospitalized.
Diagnostics Catatonic excitement
The team that arrives at the call must assess the stage of catatonic agitation and the degree of aggressiveness of the patient. In addition, it is necessary to try to avoid aggression directed directly at others and oneself. Patients are usually not sociable, so prehospital diagnostics are carried out visually based on clinical manifestations.
Relatives can help clarify the situation and point the way to the search by telling whether the patient has had manifestations of catatonia before, whether he has a psychiatric or neurological disease, addiction, what immediately preceded the appearance of symptoms of catatonic agitation (taking drugs, other psychoactive substances, receiving injuries, the possibility of poisoning, etc.).
In addition to establishing the fact that the patient is in catatonic excitement, the main diagnostics - the type and determination of the cause of the development of this condition is carried out during observation of the patient in the hospital and after performing studies - laboratory and hardware. Clinical and biochemical blood tests are prescribed, the function of the kidneys, liver and thyroid gland, the level of glucose, autoantibodies and CO2, heavy metals in the blood, creatine phosphokinase and narcotic substances in the urine are examined. Blood and urine culture tests may be prescribed, the patient is tested for HIV infection and syphilis. [ 12 ]
An electroencephalogram is used to assess the activity of certain areas of the brain, an electrocardiogram is prescribed to assess the work of the heart, an ultrasound of the internal organs, CT and MRI, and other studies necessary to identify the cause of catatonic agitation may be prescribed.
Differential diagnosis
Differential diagnostics is carried out between the causes that caused the development of the syndrome, which is important for choosing treatment tactics and placing the patient in a psychiatric or somatic department.
First of all, catatonic schizophrenia and autism are excluded, as well as affective disorders in the manic phase. In addition, unipolar disorders are differentiated from intermittent manic and depressive episodes ( bipolar disorder ). Post-stress condition also requires differentiation from mental illnesses, and the severity of the reaction to the stress factor indicates what measures need to be taken. [ 13 ]
Exogenous delirium caused by the ingestion of psychoactive substances and requiring neutralization of their action is differentiated from the condition caused by other reasons - trauma, neuroinfections, epilepsy, tumors. Magnetic resonance imaging allows to exclude or confirm brain tumors, consequences of its traumatic injuries, neurochemical disorders. Laboratory studies - intoxication, hormonal and metabolic disorders.
Differential diagnosis is carried out with epileptic seizures (according to electroencephalography data) and other manifestations of hyperkinetic syndromes in mental disorders.
Catatonic agitation, unlike other types of psychomotor agitation (affective, delusional, hallucinatory, manic), is characterized by the meaninglessness of actions and a complete lack of motivation.
The patient automatically performs unrelated, aimless and disjointed actions. They may be directed at external objects or at the patient himself. It is difficult to determine whether he retains self-awareness or perceives his body as an external object.
Lucid catatonia is differentiated from the oneiroid state. It is difficult to distinguish between the catatonic-hebephrenic phase and hebephrenic excitement, in which the patient also acts affectedly, fools around, displays childishness and emotional lability.
After a comprehensive examination, the patient is prescribed a course of treatment in accordance with the identified pathology. It happens that the cause of catatonia remains unknown (idiopathic catatonic agitation).
Who to contact?
Treatment Catatonic excitement
The general tactics of the ambulance team called to a patient with catatonic agitation are reduced to preventive measures to ensure the safety of the patient, those around him and the medical staff. In large cities, a specialized psychiatric team arrives at the call, in small cities and rural areas - more often a linear team.
The main task at the pre-hospital stage is to safely deliver the patient to a psychiatrist for consultation. The approach is symptomatic. Catatonic agitation has a number of specific signs - monotony of movements and statements, their meaninglessness, automatic repetition. Emergency care includes physical restraint of the patient, if necessary - fixation and pharmacotherapy. Moreover, physical effects should be preferred, since pharmacotherapy can "blur" the symptoms and complicate further diagnostics in the emergency room of the hospital. [ 14 ]
Acute catatonic agitation and its severity are detected during attempts to establish initial contact and build trust with the patient, during which the tactics of further actions are determined, which sometimes allows replacing drug assistance or calming the patient down a bit and making it possible. However, medical personnel who arrive at a call to a patient in a state of acute psychosis should not lose "psychiatric vigilance" for a second, since the patient's behavior can change diametrically at any moment.
The nurse's actions in case of catatonic excitement should fully correspond to the doctor's actions. It is necessary to ensure that there are no objects suitable for attack or self-harm in the immediate vicinity of the patient. If the patient is aggressive, it is better to be closer to the door, which should not be locked, and the patient should not be allowed to approach the window. It is advisable to enlist the support of relatives, police officers, orderlies, ambulance drivers, etc.
When providing medication, the nurse gives an intramuscular injection or, if possible, gives an oral medication, making sure that the patient swallows it.
In case of catatonic agitation, it is preferable to use tranquilizers of the benzodiazepine group. The drugs are used in the form of intramuscular injections of a 0.25% solution of lorazepam in a single dose of 2 to 8 ml or a 0.5% solution of diazepam - from 2 to 6 ml. If the patient is cooperative, you can give him the drugs in tablets to swallow: lorazepam from 5 to 20 mg or diazepam from 10 to 30 mg. [ 15 ]
The same drugs are used in low doses for further treatment of catatonia in hospital. Sometimes catatonic manifestations disappear after taking just one dose. [ 16 ]
Patients who do not respond to benzodiazepine drugs are prescribed electroconvulsive therapy.
In the hospital, after a full examination of the patient, further treatment is prescribed based on the diagnosis.
Prevention
Catatonic arousal is caused by various pathological conditions of the body, so preventive measures are general. First of all, it is a responsible attitude to your health, mental and physical: eradication of bad habits, increasing stress resistance and positivism, commitment to an active lifestyle, optimization of the daily diet. This can be done independently, but if it does not work, then there is a wide network of psychotherapeutic assistance, as well as health groups, nutritionists, psychosomatics. Such measures will significantly reduce the risk of both mental and physical illnesses.
People from the risk group, i.e. those suffering from diseases of the catatonic spectrum, need to undergo regular examinations by the attending physician and follow his recommendations for maintaining the state of remission. As practice shows, acute catatonic excitement is removed very quickly, sometimes with one dose of the appropriate drugs, therefore, at the first symptoms of trouble, it is necessary to seek professional help.
Forecast
Overall, most patients who have experienced catatonic agitation have a good prognosis, especially if the underlying cause is eliminated.
The acute clinical stage can be stopped fairly quickly. However, there is a risk of relapses of catatonic episodes and the development of cognitive deficit in the future in patients with chronic diseases - schizophrenia, epilepsy, severe clinical depression. The long-term prognosis depends on the pathology that caused the appearance of catatonia.

