Medical expert of the article
New publications
Atherosclerosis of the renal arteries
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Medium and large arteries of the brain, heart and many vital organs, as well as lower extremities are subject to atherosclerotic lesions. Atherosclerosis of renal arteries, as well as other visceral arterial vessels, is associated with thickening of their walls and narrowing of the lumen. According to ICD-10, the code of this disease (in the class of diseases of the circulatory system) is I70.1. [1]
Epidemiology
According to clinical statistics, renal artery atherosclerosis accounts for 90% of all cases among renovascular lesions. The age of the majority of patients is over 60 years.
The prevalence of familial hypercholesterolemia is estimated at one case per 250-300 people.
Atherosclerosis-associated renal artery stenosis (with 60% or more reduction of the vessel lumen) is detected in 15% of patients. [2]
Causes of the atherosclerosis of the renal arteries
Renal artery atherosclerosis is a renovascular disease whose key causes are related to hyperlipidemia (dyslipoproteinemia or hyperlipoproteinemia) with a disorder of fat metabolism and mechanisms in their transportation. Because of this, cholesterol (cholesterol) levels rise in the blood and hypercholesterolemia develops. [3]
As a rule, the proximal third of the renal artery or its orifice is affected, but the pathology can also affect the perirenal aorta. In advanced cases, segmental and diffuse atherosclerosis of the intrarenal interlobular arteries may be observed.
The fact that 30-50% of patients with atherosclerotic renal artery narrowing have symptomatic coronary, cerebral, or peripheral arterial lesions should also be considered.
Also read - atherosclerosis - Causes and Risk Factors
Risk factors
Risk factors for atherosclerotic lesions of the renal artery walls include: excessive blood levels of cholesterol, low-density lipoprotein (LDL) and triglycerides; high blood pressure (arterial hypertension); smoking; poorly controlled diabetes mellitus; metabolic syndrome and obesity; lack of physical activity and saturated fat intake; and age over 55-60 years.
The risk of renal artery atherosclerosis is increased in familial hypercholesterolemia caused by mutations in: LDLR gene (encoding low-density lipoprotein receptor adaptor protein 1), APOB gene (encoding the major LDL protein - apolipoprotein B), PCSK9 gene (encoding an enzyme of the proprotein convertase family, which is involved in cholesterol homeostasis).
Risk factors include hyperhomocysteinemia - accumulation of the amino acid homocysteine (which is formed during the breakdown of proteins) in the body, especially in case of low thyroid hormone levels and deficiency of folic acid or cyanocobalamin (vitamin B12). [4]
Pathogenesis
The pathogenesis of focal thickening or thickening of arterial walls in atherosclerosis is explained by the formation of atheromatous or atherosclerotic plaques (cholesterol deposits) on the inner lining of the artery (tunica intima) lined by endothelium, which regulates tone, hemostasis, and inflammatory responses throughout the circulation. For more information, see. - arteries
The formation of plaques occurs gradually. Arterial endothelium reacts to various mechanical and molecular stimuli by formation of free radicals and activation of proinflammatory factors, leading to vascular endothelial cell damage and dysfunction.
First, there is a deposition of LDL cholesterol particles oxidized by free radicals on the inner wall of the vessel, which provokes the accumulation of leukocytes and monocytic cells - macrophages.
Further, under the action of cellular and intercellular adhesion molecules attracted to the site of fatty deposits, there is formation of foam cells, which are a type of macrophages in fatty deposits, which absorb low-density lipoproteins by endocytosis (free cholesterol moves into the endoplasmic reticulum of macrophages, is esterified and stored there). At the same time, foam cells forming fatty inclusions of atheromatous plaques in the intima of blood vessels secrete proinflammatory cytokines, chemokines and reactive oxygen species.
As the deposits increase, they can harden, protruding into the lumen of the artery and reducing blood flow. [5]
Symptoms of the atherosclerosis of the renal arteries
The insidiousness of renal artery atherosclerosis is that its initial stage is latent, that is, asymptomatic.
And the symptoms - years later - begin to manifest as persistent arterial hypertension, which is defined as renovascular, vasorenal or nephrogenic (renal) hypertension. That is, patients experience symptoms of high blood pressure (which do not go away after taking medications to lower it).
Next, due to narrowing of the renal arteries, there is a decrease in kidney function - with increased proteins in the urine - proteinuria, with swelling of the ankles or feet due to fluid retention.
Deterioration of blood supply to the kidneys leads to ischemia of its tissues and progressive damage with the appearance of symptoms of chronic renal failure. [6]
Complications and consequences
The main complications and consequences of atherosclerotic lesions of the renal arteries are:
- Life-threatening persistent elevation of BP;
- Atherosclerotic renal artery stenosis; [7]
- Ischemic nephropathy and functional renal failure associated with decreased renal blood flow and insufficient blood supply to the organ;
- Development of atheroembolic kidney disease in patients with severe atherosclerosis - blockage of its arterioles by particles of destroyed atherosclerotic plaques of renal arteries that have entered the bloodstream;
- Progression of systemic atherosclerosis and development of cardiac destabilization syndrome with transition to cardiovascular disease. According to some data, 12-39% of patients with atherosclerotic stenosis of renal arteries are diagnosed with coronary heart disease (progressing within five years by almost 50%).
In addition, when an atherosclerotic plaque breaks down, a blood clot (thrombus) forms that blocks blood flow and can lead to sudden catastrophic thrombosis, and a clot that breaks off can lead to sudden death. [8]
Diagnostics of the atherosclerosis of the renal arteries
Diagnosis begins with a review of the patient's history, including family history and physical examination.
Blood tests for LDL, HDL, LDL-CS, total cholesterol and triglycerides; protein and C-reactive protein; creatinine, urea nitrogen and homocysteine; and renin and aldosterone hormones. Blood and urine tests to assess renal function are also required.
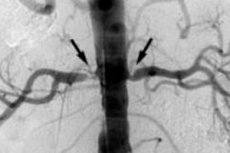
Instrumental diagnostics includes: renal ultrasound, ultrasound Doppler vascular kidney, computed tomographic angiography (CTA), magnetic resonance angiography (MRA). [9]
Differential diagnosis with renal artery thrombosis, fibromuscular dysplasia (hyperplasia) of the vascular wall, diabetic nephropathy is performed.
Read also - renal Artery Stenosis - Diagnosis
Who to contact?
Treatment of the atherosclerosis of the renal arteries
Treatment of hypercholesterolemia is medication, and the main drugs are cholesterol-lowering hypolipidemic agents of various pharmacological groups. [10]
May be assigned:
- Drugs of the group of statins (inhibitors of the enzyme HMG-CoA reductase, providing cholesterol metabolism): simvastatin (Simvacard, Vabadin), Fluvastatin, Lovastatin (Mevacor ), Rosuvastatin and others. However, these agents are contraindicated in case of uncontrolled diabetes and hypothyroidism.
- Drugs that bind bile acids in the intestine: Colestiramine (Colestid, Cholestiramine. Colestipol, etc. Their use may be accompanied by side effects such as heartburn, nausea, vomiting, constipation or diarrhea. They are not prescribed in the presence of blood coagulation disorders, gastroesophageal reflux and peptic ulcer disease, autoimmune cirrhosis of the liver and gallstones.
- Agents inhibiting cholesterol synthesis in the liver: Fenofibrate (Lipantil), Clofibrate (Atromid-C), Bezafibrate, Atorvastatin (Atoris, Tulip), Gemfibrozil (Lopid). It should be borne in mind that fibroic acid preparations may cause abdominal and muscular pain, heart rhythm disturbances and cholelithiasis.
- Selective cholesterol absorption inhibitors Ezetimibe (Ezetrol, Lipobon);
- Niacin - vitamin PP (nicotinic acid).
More information in the articles:
In addition, it is necessary to treat arterial hypertension and diabetes, because these comorbidities accelerate the progression of renal artery atherosclerosis. And be sure to eat properly, details:
Surgical treatment with balloon angioplasty and percutaneous stenting of the affected vessel is used to restore the lumen of the renal artery in case of stenosis. [11]
Prevention
Prevention of renal artery atherosclerosis is to prevent the increase of cholesterol and LDL levels in the blood. And for this purpose it is necessary to:
- To stop smoking;
- Eliminate trans fats from your diet and add fruits and vegetables and healthy fats (found in nuts and seafood);
- To control blood sugar levels;
- Get rid of the extra weight and move more.
Forecast
Atherosclerosis of the renal arteries is a progressive disease, and stenosis of these vessels, which in 80% of cases is associated with atherosclerotic lesions, negatively affects the prognosis in terms of decreased renal function, often reaching a terminal stage.

