Medical expert of the article
New publications
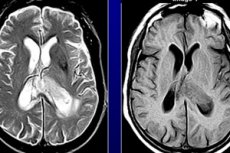
Astrocytoma in children
Last reviewed: 05.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
There is probably nothing more frightening for parents than to learn that their child has cancer or even a benign tumor in the brain that will have to be removed surgically, and this is associated with a certain risk. Brain tumors are not as common as gastritis or bronchial asthma, however, the probability of such a disease in a child really exists, and preventive measures cannot be developed until scientists accurately determine the cause of brain tumors.
Epidemiology
Today, primary brain tumors are the leading cause of cancer death in children and adolescents aged 20 years and younger, now surpassing leukemia, and the third leading cause of cancer death in young adults aged 20 to 39 years. Gliomas are the most common primary tumors of the central nervous system in both children and adults. The World Health Organization (WHO) classifies this heterogeneous group of tumors into four main groups: astrocytomas; oligodendrogliomas; mixed oligoastrocytomas; and ependymal tumors.[ 1 ],[ 2 ]
Causes astrocytomas in a child
When it comes to a child, the number of factors that can presumably cause the development of a tumor process, including astrocytoma in a child, is even narrower. Radiation and exposure to chemicals are more associated with professional activities, so they are not relevant in childhood.
As for viruses, it takes time for the active tumor process they provoke. And we know that children most often have tumors with slow growth. Therefore, it is difficult to explain tumors in children by the influence of viruses.
A more likely factor is hereditary predisposition, but it does not explain why brain astrocytomas are not diagnosed in the prenatal and early postnatal period. It seems that this is an acquired pathology, but what triggers the process in this case?
There is a possibility that the disease may actually be congenital, but at an early age it is not possible to detect its symptoms. Rarely occurring malignant tumors are detected postmortem during autopsy, and benign tumors develop slowly, so their symptoms are detected later, when the child has grown up.
Many doctors today are inclined to believe that negative intrauterine factors during embryogenesis can provoke tumor formation to the same extent as mutagenic factors, especially when it comes to their combined effects.
Symptoms astrocytomas in a child
The first signs of the disease may go unnoticed or be attributed to other diseases due to their non-specificity. A child's decreased activity, rapid fatigue, poor appetite, and hence low weight, symptoms of dyspepsia do not always indicate a brain tumor. There are many childhood diseases with a similar clinical picture.
It is a different matter if we are talking about a delay in psychomotor development, which is controlled by the brain. But even here, tumors are not among the first causes. There are many other factors that can affect brain development in the prenatal period and after the birth of the child, which will lead to disturbances in psychophysical development. So the child can be observed for a long time, without suspecting the true picture of the disorder.
A more specific manifestation of the disease is considered to be hypertensive-hydrocephalic syndrome (HHS). Although it is not always associated with tumors. Suspicion should be aroused by: a head that is not large for the age, pronounced cranial sutures that do not ossify for a long time, a large bulging tense fontanel. Bad symptoms are considered to be sleep disturbances in a small child, monotonous crying with the head thrown back, dilation of the venous network in the forehead, temples and bridge of the nose.
Doctors also highlight some specific manifestations of HGS: Graefe's symptom (the setting sun symptom or a wide white stripe between the iris and the upper eyelid when the child lowers his eyes down) and the rising sun symptom (covering almost half of the iris with the lower eyelid).
The Graefe symptom itself does not always indicate pathology. It is often observed in infants up to 6 months. You should suspect something is wrong if this symptom is accompanied by other deviations: profuse regurgitation, strong excitability, tremor, deviation of the visual axes, which is easily noticed by the asymmetrical arrangement of the corneas (strabismus). These are all manifestations of hydrocephalic syndrome associated with increased intracranial pressure.
In newborns who cannot yet complain of headaches, pathology can be suspected based on the baby's behavior: poor breastfeeding, crying for no reason, moaning, weak grasping and swallowing reflexes, decreased muscle tone ("seal paws"), significant head growth (from 1 cm per month).
Older children may be capricious or report headaches, nausea, they may often vomit, feel dizzy, and have decreased visual acuity [ 3 ]. Complaints about difficulty lowering the eyes or raising the head are not uncommon.
The onset of headaches can be noticed by pale skin, weakness and apathy, and at the same time the child begins to be irritated by loud sounds, bright light, noise, etc. Sometimes children begin to walk on tiptoes, some have epileptic seizures. Almost always, a brain tumor leaves its mark on the child's mental development. If the tumor appeared early, the baby will initially lag behind in development, with a later development of the process, a deterioration in memory and cognitive abilities, and the loss of some skills are noted. [ 4 ]
Treatment astrocytomas in a child
It is clear that such symptoms cannot be ignored, even if they are not associated with a tumor process. In children, benign tumors are most often detected, so parents are faced with a difficult choice: leave everything as is or risk a risky neurosurgery or chemotherapy. [ 5 ]
While the relatives are deciding, the tumor is gradually growing, affecting the child's development and can make him disabled, affecting both the intellectual, emotional and motor spheres depending on its location. The child can go blind or lose hearing, and if the tumor is large, fall into a coma and die. Doctors consider it necessary to remove both rare malignant and benign tumors at an early age, and the sooner the better.

