Medical expert of the article
New publications
Vaginal aplasia
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Vaginal aplasia is a deviation from the norm of female genital development, which includes a complete or partial absence of the vagina. This anomaly was first identified by the German scientist Mayer, and Rokitansky and Müller supplemented the diagnosis by discovering the absence of the uterus in parallel with this defect.
 [ 1 ]
[ 1 ]
Causes vaginal aplasia
The cause of vaginal aplasia is a congenital defect, often accompanied by defects or absence of anatomically adjacent organs: the uterus, kidneys. There is no clear answer to what provokes the development of such an anomaly. Most often, the occurrence of such cases is isolated and is not associated with heredity. There are also precedents of the existence of this dysfunction in several generations of women of the same family, which gives reason to talk about a genetic predisposition. At the genetic level, they have a normal set of 46 chromosomes with a standard type of the last XX. The formation of the uterus occurs at the embryonic stage at the end of the second month of intrauterine development of the fetus, starting with the Müllerian ducts. The uterus, fallopian tubes and vagina are formed from them. It is assumed that various infectious diseases, especially sexually transmitted diseases (trichomoniasis, papillomavirus infection, genital herpes, etc.), strong and prolonged exposure to chemicals, and improper douching can lead to a defect in the infant's reproductive system.
 [ 5 ]
[ 5 ]
Risk factors
Based on the presumed causes of uterine aplasia, risk factors include:
- chronic inflammation of the genital organs of the expectant mother;
- any diseases, including viral infections, that have resulted in long-term treatment with antibiotics and other medications;
- hormonal imbalances;
- neuropsychiatric disorders.
Pathogenesis
The pathogenesis of the disease has not been fully established to date, but it is obvious that this defect is caused by biological inferiority of the cells involved in the formation of the future sexual organ. The complete absence or deficiency of estrogen receptors in the Müllerian tubules leads to their partial fusion or non-fusion, which is what causes the anomaly. Often, defects in the urinary and musculoskeletal systems prevent the fusion of the walls of the Müllerian ducts.
Symptoms vaginal aplasia
Vaginal aplasia does not affect a woman's appearance in any way. All secondary sexual characteristics correspond to age. Symptoms appear when puberty occurs. They often signal themselves with pain in the pelvic area, heaviness in the lower abdomen, and absence of menstruation. With partial aplasia, heavy bleeding is possible with the inability to insert a tampon. Sometimes urination is accompanied by painful sensations, and defecation is impaired. In some cases, vomiting occurs, and the temperature rises.
Often the first sign indicating the existence of a developmental defect of the reproductive system is the absence of menstruation upon reaching puberty. Some girls experience an unsuccessful attempt at their first sexual intercourse, while others are bothered by severe attacks of periodic pain that do not go away after taking painkillers.
Forms
Vaginal aplasia is divided into complete and partial. In case of partial absence of the vagina, the transverse septum can be complete or incomplete, its walls can have different thickness and be located in different parts of the upper third of the vagina.
By appearance, complete aplasia can be:
- with a full-fledged uterus;
- with uterine aplasia;
- with aplasia of the cervix and the canal connecting the internal and external genital organs.

Aplasia of the uterus and vagina
Aplasia of the uterus and vagina is also called Rokitansky-Küster-Mayer syndrome. In this disease, the uterus is completely absent, but there are normally functioning ovaries. Secondary sexual characteristics are formed without deviations, there is no periodic pain syndrome.
Complications and consequences
The consequences of vaginal aplasia are infertility and the impossibility of a full intimate life without surgical removal of the anomaly. At the same time, this is a big psychological blow for every girl, which she must overcome. Complications can arise when attempting the first sexual intercourse. Not knowing her defect, a girl can get a rupture of the perineum, urethra.
Diagnostics vaginal aplasia
The initial physical examination of the genitals on the examination table does not show any abnormalities in the structure of the external genitalia and confirms the presence of hair on the pubis. In case of aplasia of both the vagina and the uterus, there are some peculiarities in their location. Thus, the surface of the vaginal vestibule may be smoothed from the urethra to the rectum, the hymen may be without a depression in the perineum and have an opening through which aplasia is detected. Palpation of the abdomen reveals a cord instead of the uterus. To clarify the diagnosis, laboratory tests of urine, blood, instrumental and differential examination are prescribed.
 [ 25 ], [ 26 ], [ 27 ], [ 28 ]
[ 25 ], [ 26 ], [ 27 ], [ 28 ]
Tests
If vaginal aplasia is suspected, the tests are of little information, but are necessary to determine the background against which the defect developed. For this purpose, a urine test is prescribed, as well as a general and detailed blood test. The studies will show the hormonal level, its possible imbalance. Bacteriological and bacterioscopic analysis of a smear and biomaterial will determine the microflora of the genital tract, the presence of inflammation, fungi, bacteria, and possible venereal diseases.
Instrumental diagnostics
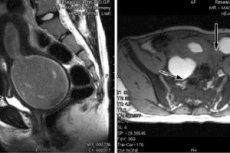
The most important mechanism for establishing the correct diagnosis in case of vaginal aplasia is instrumental diagnostics. Using a probe during examination allows you to identify the vagina behind the hymen, which ends blindly. If such measures are insufficient to establish a diagnosis, laparoscopic diagnostics are used. This is a minimally invasive surgical method of examination, which makes it possible to penetrate the abdominal cavity through small holes with the help of an optical laparoscope and provide an enlarged image of the reproductive organs on the monitor. Non-surgical diagnostic methods - ultrasound examination (US) and magnetic resonance imaging (MRI) of the abdominal organs will show whether there are defects in other reproductive or adjacent organs. There may be no uterus with normal ovaries and fallopian tubes, or it may be underdeveloped, defects in the urinary system are detected.
What do need to examine?
Differential diagnosis
Differential diagnostics is very important for determining the diagnosis and is designed to protect the patient from improper treatment. In girls with uterine aplasia, a compaction is detected at a distance of 2-8 cm from the anus during examination on a gynecological chair and during abdominal palpation, which can be mistaken for a cyst or tumor. Painful sensations can be mistaken for an attack of acute appendicitis, torsion of the ovarian pedicle, or vulvovaginitis.
Who to contact?
Treatment vaginal aplasia
Treatment of vaginal aplasia involves eliminating the congenital anomaly using colpopoiesis – artificial creation of a neovagina. This is not always plastic surgery. There is a bloodless method using a colpoelongator – a special protector. The essence of this method is the gradual stretching of the vaginal vestibule membrane using a special device. The procedure is carried out under the supervision of medical personnel, the pressure on the tissue is adjusted based on the woman’s sensations. The duration of the procedure at the first stages is 20 minutes, gradually increasing to half an hour to forty minutes twice a day. The course of treatment is 15-20 procedures. It can be repeated after 2 months. Most patients achieve tissue stretching up to 10 cm. Drug treatment is not required.
If conservative treatment has failed, surgical intervention is resorted to. The history of such operations dates back to the early 19th century. But without endoscopic devices, operations were accompanied by high trauma and significant complications. There were various technologies: using silver or stainless metal prostheses in the created channel, through the rectum and with the formation of a neovagina from skin flaps, etc. The modern method of colpopoiesis involves a combination of invasive and laparoscopic methods. The operation is performed simultaneously in two places: some surgeons - through the pelvic peritoneum, others - through the perineum, where a channel is formed between the bladder and the rectum. Then the peritoneal wall is sutured to the vestibule of the vagina and its dome is formed.
A month after the operation, a full sexual life can begin. To prevent the walls of the newly formed vagina from sticking together, it is necessary to have regular sexual life or to perform artificial bougienage. In the future, it is necessary to undergo a medical examination once every six months to diagnose cicatricial changes in the vagina in time.
Prevention
There is currently no prevention of vaginal aplasia. It exists at the level of recommendations for pregnant women who want to give birth to healthy offspring - to be very careful in the first trimester of pregnancy, when the genitals are formed at the embryonic level. Alcohol, smoking, various chemical exposures, harmful industries, viral infections - these are factors that can harm the future girl, her psyche, take away the joy of a full sexual life and the joy of motherhood.
Forecast
Modern technologies, invention and use of high-precision diagnostic and surgical equipment give hope to patients and make the prognosis of the disease favorable. In vitro fertilization has made it possible for women with vaginal aplasia to experience the joy of motherhood through surrogacy.

