Medical expert of the article
New publications
Adrenal adenoma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
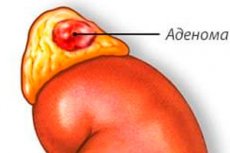
Adrenal adenoma is a benign tumor that develops in the adrenal glands, paired organs located above the kidneys.
The adrenal glands, located above the kidneys, produce hormones. They are composed of both medullary and cortical tissue. The adrenal medullary tissue, which makes up approximately 15% of the adrenal mass, responds to circulating dopamine during stressful situations by producing and releasing catecholamines as part of the sympathetic response to stress. [1] The adrenal cortex can be divided into distinct areas known as the medullary zone, bundle zone, and reticular zone. Each zone is responsible for the production of certain hormones, namely mineralocorticoids, glucocorticoids and androgens respectively.
Androgen-producing adenomas are extremely rare and are more commonly combined with adrenocortical carcinoma. [2], [3] Excess cortisol production can be categorized according to the amount of hormone produced and the associated symptoms. Adenomas producing cortisol associated with systemic symptoms are considered typical manifestations of Cushing's syndrome. On the other hand, adenomas that produce cortisol in smaller amounts, without overt signs of hypercortisolism, are called mild autonomous cortisol secretion tumors (MACS).
Here is more information on causes, symptoms, diagnosis, treatment and prognosis separately:
Reasons:
- The causes of adrenal adenomas can vary, but the exact causes often remain unknown. In some cases, adrenal adenomas may be associated with genetic mutations or hereditary factors.
- It is important to note that in some cases, an adrenal adenoma can be functional, meaning it produces excess hormones, leading to the development of related symptoms and diseases.
Symptoms:
- Symptoms of adrenal adenoma may depend on the type of hormones it produces and the excessive amount of hormones. For example, symptoms may include high blood pressure (hypertension), excess weight, muscle weakness, decreased bone mass (osteoporosis), menstrual irregularities in women, increased facial and body hair (hirsutism), and others.
Diagnosis:
- Diagnosis of adrenal adenoma may include various methods such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and blood tests to determine hormone levels.
- Accurate diagnosis determines the type of tumor and its functional activity.
Treatment:
- Treatment for adrenal adenomas may include surgical removal of the tumor (adenomectomy), especially if the tumor is large, functional, or causing severe symptoms. Surgery may be performed using laparoscopic techniques, which usually allows for a shorter recovery period.
- In some cases, if the tumor is non-functional and does not pose a serious threat, the doctor may decide to simply monitor it.
Prediction:
- The prognosis depends on many factors, including the size and type of tumor, the presence of symptoms, the success of surgery, and other factors. In most cases, if an adrenal adenoma is detected early and successfully removed, the prognosis is usually favorable.
- However, it is important to monitor your condition after treatment and check in with your doctor regularly to look for recurrences or other problems.
Epidemiology
The increasing use of computed tomography (CT) has led to an increase in the reported incidence of adrenal adenoma. The reported prevalence of adrenal incidentaloma varies depending on the criteria used. Based on CT scans, studies have reported the prevalence of adrenal incidentalomas to range from 0.35% to 1.9%. However, a series of autopsies showed a slightly higher prevalence of 2.3%. [4]
Adrenal adenomas account for approximately 54% to 75% of adrenal incidentalomas. [5] Although most studies indicate a higher prevalence of adrenal adenoma in females than in males, [6], [7] there are a few male predominant cases, especially in a large Korean study. [8] The mean age of diagnosis is 57 years, with reported cases covering a wide age range from 16 to 83 years.
Approximately 15% of cases of adrenal incidentalomas have hypersecretion of hormones. The reported prevalence of hypercorticism ranges from 1% to 29%, hyperaldosteronism from 1.5% to 3.3%, and pheochromocytoma from 1.5% to 11%. [9]
Causes of the adrenal adenomas
The causes of adrenal adenoma can vary and may include:
- Genetic predisposition: Certain genetic mutations are associated with both hormonally active and hormonally inactive adrenal adenomas. However, the exact mechanisms underlying their pathogenesis remain unclear. [10] Some cases of adrenal adenoma may be associated with the presence of inherited genetic mutations or a family history of the disease. For example, hereditary adrenal hyperplasia syndromes such as Mendelson syndrome may increase the risk of developing adenoma. [11]
Mutations in the CTNNB1 gene, which provides instructions for beta-catenin production (Wnt/beta-catenin pathway), are associated with the development of larger, non-secreting adenomas of the adrenal cortex. [12]
Mutations associated with cortisol-producing macronodular adrenal nodules include PRKACA (associated with cortisol-producing adenoma), [13], [14] GNAS1 (associated with McCune-Albright syndrome), [15] MENIN (associated with multiple endocrine neoplasia type 1)., ARMC5 (associated with primary bilateral macronodular adrenal hyperplasia), APC (associated with primary bilateral macronodular adrenal hyperplasia), and FH (associated with primary bilateral macronodular adrenal hyperplasia). [16] Micronodular adrenal hyperplasia producing cortisol results from PRKAR1A (associated with primary adrenal pigment nodular disease due to altered Carney complex), PDE11A (associated with isolated micronodular adrenal disease), and PDE8B (also associated with isolated micronodular adrenal disease). [17]
Mutations associated with aldosterone-producing adrenal adenomas include KCNJ5, which accounts for approximately 40% of such cases. [18] In addition, mutations in ATP1A1, ATP2B3, CACNA1D, and CTNNB1 are also associated with this disease.[19]
- Random Mutations: In rare cases, adrenal adenomas can develop due to random mutations in the cells of the adrenal gland.
- Increased hormone secretion: Increased production of certain hormones by the adrenal glands may contribute to the development of an adenoma. For example, the adrenal glands produce hormones such as cortisol, aldosterone, and adrenaline, and increased release of these hormones can set the stage for tumor development.
- Uncontrolled use of hormone medications: Prolonged and uncontrolled use of certain hormone medications, such as glucocorticosteroids, can increase the risk of adrenal adenoma.
- Idiopathic adenoma: In some cases, the cause of adenoma development remains unknown and is referred to as "idiopathic".
Symptoms of the adrenal adenomas
Symptoms of adrenal adenoma can vary depending on its size, functional activity, and other factors. Here are some of the possible symptoms:
- Hypertension (high blood pressure): Due to excessive release of hormones such as aldosterone or catecholamines, adrenal adenoma can cause high blood pressure.
- Weight gain: Some tumors can cause excess fluid accumulation and weight gain.
- Skin hyperpigmentation: Due to excess production of ACTH (adrenocorticotropic hormone) by the adrenal glands, skin pigmentation may develop, especially on mucous membranes and lined areas of the body.
- Glucose and metabolic disorders: Excess production of hormones by the adrenal glands can affect metabolism and cause glucose and insulin resistance.
- Hormonal Disorders: Symptoms may include levels of hormones such as cortisol (corticosteroids), which can lead to Icenko-Cushing's syndrome, or androgens (male sex hormones), which can cause symptoms associated with hyperandrogenism in women.
- Abdominal or back pain: In some cases, adrenal adenoma can cause discomfort or pain in the abdominal or back area.
Complications and consequences
Cushing's syndrome resulting from cortisol-producing adrenal adenoma is associated with a wide range of complications, among which metabolic and cardiovascular disorders are particularly noteworthy. [20] The side effects are primarily attributed to a mechanism of increased insulin resistance caused by hypercorticism, leading to a subsequent increase in abdominal obesity. [21] Over the past few years, these complications have also been reported in adrenal adenomas with MACS. [22], [23] In addition, cortisol overproduction suppresses the hypothalamic-pituitary-thyroid axis and stimulates somatostatin, which reduces T3/T4 hormone levels. [24] The same mechanism of action is also responsible for decreased growth hormone production in these patients. [25]
The most common complication associated with aldosterone-producing adenomas is uncontrolled arterial hypertension. Without proper diagnosis and treatment, primary hyperaldosteronism can lead to sodium and water retention at the nephron level, resulting in complications such as fluid overload, heart failure, atrial fibrillation, and myocardial infarction. [26]
In rare cases, nonfunctioning adrenal adenomas can lead to mass effects. However, it is important to note that most lesions large enough to cause mass effects are usually malignant.
Diagnostics of the adrenal adenomas
Diagnosis of adrenal adenoma involves various methods and tests that help in detecting the presence of tumor, determining its size, nature and location. Here are some of the main methods for diagnosing adrenal adenoma:
- Clinical examination and history taking: The doctor performs a general examination of the patient and asks questions about symptoms that may be associated with adrenal adenoma, such as hypertension (high blood pressure), hyperpigmentation (increased skin pigmentation), excessive hair, and others.
- Blood tests:
- Determination of adrenal hormone levels such as cortisol, aldosterone, and dehydroepiandrosterone (DHEA).
- Determination of adrenocorticotropic hormone (ACTH) levels in the blood.
- Immunodiagnosis: Measurement of urine and/or blood levels of 17-hydroxyprogesterone, which may be elevated in some forms of adrenal adenomas.
- Educational Methods:
- Computed tomography (CT) and/or magnetic resonance imaging (MRI) of the abdomen and adrenal glands for tumor imaging and tumor characterization.
- Ultrasound of the abdomen and adrenal glands.
- Biopsy: Sometimes a biopsy of an adrenal adenoma is needed to determine its nature (e.g., malignant or benign). The biopsy may be done by puncture through the skin or by laparoscopy.
- Functional tests: In some cases, special tests, such as adrenal hormone secretion tests, may be performed to determine how the tumor is affecting hormone levels in the body.
Evaluation of adrenal tumors primarily focuses on two key goals: the first goal is to distinguish between benign and malignant masses, while the second goal is to determine whether tumors are hormonally active or nonfunctional. [27]
Once an adrenal mass has been detected, CT or magnetic resonance imaging (MRI) is the preferred imaging modality for evaluation of adrenal adenomas. [28] An adrenal tumor larger than 4.0 cm has a high sensitivity for adrenal carcinoma. [29] In addition, adrenal lesions showing less than 10 Hounsfield units (HU) on noncontrast CT strongly suggest a benign adenoma. [30] Some benign adenomas may have values above 10 HU. In such cases, delayed contrast-enhanced CT may help differentiate benign from malignant lesions. [31], [32]
Absolute contrast washout of more than 60% and relative washout of more than 40% on delayed CT images have been reported to be highly sensitive and specific for the diagnosis of patients with adenomas compared with patients with carcinomas, pheochromocytomas, or metastases. [33], [34] However, a recent study showed that contrast washout has lower sensitivity and specificity for accurately recognizing benign adenomas. [35] MRI can be used to evaluate adrenal neoplasms as an alternative to CT. MRI with chemical shift imaging has demonstrated high sensitivity and specificity in the diagnosis of adrenal adenomas.
Differential diagnosis
Differential diagnosis of adrenal adenoma involves identifying and distinguishing this condition from other possible diseases or conditions that may mimic the symptoms of adrenal adenoma. It is important to consider that adrenal adenomas can be functional (producing excess hormones) and non-functional (not producing excess hormones), which also affects the differential diagnosis process. Here are some of the possible diagnoses and tests that may be included in the differential diagnosis of adrenal adenoma:
- Glucocorticosteroids: High cortisol levels may be associated with adrenal adenoma or Icenko-Cushing's syndrome. Comparison with other causes of elevated cortisol such as Addison's Syndrome (lesion of the adrenal cortex), endogenous depression, steroid medications, etc. May be done for differential diagnosis.
- Aldosterone: Elevated aldosterone may be associated with adrenal adenoma or primary hyperaldosteronism (Conn's syndrome). Blood renin and aldosterone levels and specialized tests may be performed for differential diagnosis.
- Adrenaline and noradrenaline: Pheochromocytoma, an adrenal tumor that produces excessive amounts of adrenaline and noradrenaline, may mimic an adenoma. Methanephrine and catecholamine profiles in urine or blood can be used for differential diagnosis.
- Neuroendocrine tumors: Some neuroendocrine tumors may be localized in nearby tissues and may mimic the symptoms of adrenal adenoma. Studies such as computed tomography (CT) or magnetic resonance imaging (MRI) can be used to detect and localize tumors.
- Metastasis: In rare cases, adrenal adenoma may be the result of cancer metastasizing from other organs. Investigations, such as biopsy or positron emission tomography (PET-CT), can help determine the origin of the tumor.
Treatment of the adrenal adenomas
Treatment for adrenal adenoma depends on several factors, including tumor size, tumor characteristics, and functional activity. It is important to consult your doctor to determine the best treatment plan for your specific case. However, common adrenal adenoma treatments may include the following steps:
- Diagnosis: It is important to accurately diagnose adrenal adenoma. This may include examination with computed tomography (CT) or magnetic resonance imaging (MRI), and blood tests to measure levels of hormones such as cortisol and aldosterone.
- Monitoring: If an adrenal adenoma is not producing excessive hormones or causing symptoms, it may only require regular follow-up with your doctor to monitor its growth and activity.
- Surgical removal (adrenalectomy): If an adrenal adenoma is actively producing excess hormones or has reached a large size, surgery may be necessary. The surgeon removes one or both adrenal glands. This may be open surgery or laparoscopic surgery, depending on the complexity of the case.
Unilateral adrenalectomy is the treatment of choice for adenomas larger than 4 cm that are suspected to be malignant or any hormonally active adenomas that have biochemical features of Cushing's syndrome or primary hyperaldosteronism. Although adrenalectomy has not been shown to be superior to medical therapy in MACS cases, leading adrenal experts have suggested that adrenalectomy should be considered for younger patients with MACS who have worsening diabetes mellitus, hypertension, or osteoporosis. [36] Discussions and shared decision-making between patients and their health care providers are essential in determining the most appropriate treatment modality.
Medical treatment of hormone-secreting adenomas is usually reserved for patients who are not suitable for surgery due to advanced age, serious comorbidities, or patients who refuse surgical correction. In such cases, the primary goal is to relieve symptoms and block hormone receptors. Mifepristone, a glucocorticoid receptor antagonist, can be used for excessive cortisol secretion. Ketoconazole may also be a potential option because of its direct effects on the adrenal glands. [37] Patients with hyperaldosteronism should be treated with mineralocorticoid receptor antagonists such as spironolactone or eplerenone.
Hormonally inactive adenomas are initially treated by repeat imaging after 3-6 months, followed by annual imaging for 1-2 years. In addition, repeat hormonal evaluations should be performed annually for 5 years. If the mass exceeds 1 cm or becomes hormonally active, adrenalectomy is recommended. [38]
- Drug treatment: In some cases, especially when surgery is not possible or before surgery, medications may be used to lower hormone levels or reduce the size of the tumor.
- Regular follow-up: After successful treatment, it is important to continue regular medical follow-up to monitor hormone levels and monitor for possible recurrences.
- Diet and lifestyle: In some cases, diet and lifestyle changes can help control symptoms and maintain adrenal health.
Postoperative and rehabilitation care
The decision for surgical correction is made after extensive discussion between the patient and the attending physician, taking into account the potential complications of the disease and the risks associated with surgery. In cases where a thorough examination confirms that the adenoma does not produce any hormones, surgical correction is not required. However, in unilateral adenomas with hormonal activity, adrenalectomy is considered the gold standard of treatment. [39], [40]
Due to excessive cortisol production in Cushing's syndrome and MACS, patients experience chronic suppression of the pituitary-pituitary-adrenal (HPA) axis. After adrenalectomy, patients will require the addition of exogenous glucocorticoids during the recovery of the HPA axis, which may take several months. According to the Endocrine Society guidelines, it is recommended that hydrocortisone be started on the first day after surgery, starting with a dose of 10-12 mg/m 2 per day, divided into 2-3 doses throughout the day.[41] Although twice-daily glucocorticoid administration is the standard approach to glucocorticoid replacement therapy, recent studies have shown that glucocorticoid administration 3 times daily may help reduce hypercortisolemia in the morning and hypocortisolemia in the evening. [42] In cases where patients cannot tolerate multiple daily doses, the use of prednisolone at a daily dose of 3 to 5 mg is an alternative option. [43] However, it should be noted that even after postoperative glucocorticoid replacement therapy, many patients may still develop symptoms of adrenal insufficiency.
Forecast
The long-term prognosis for patients with adrenal adenomas is usually favorable. Nonfunctioning adrenal adenomas often do not require treatment. Adrenal adrenal adenomas without excessive hormone production have a risk of becoming hormonally active, estimated at 17%, 29%, and 47% within 1, 2, or 5 years, respectively. [44] However, transformation of adrenal adenoma to adrenocortical carcinoma is extremely rare.
List of authoritative books and studies related to the study of adrenal adenoma
Books:
- "The Adrenal Cortex" (1991) - by Shlomo Melmed.
- "Cushing's Syndrome" (2010) - by Lynnette Nieman.
- "Adrenal Disorders" (2001) - by Bruno Allolio and Wiebke Arlt.
- "Adrenal Tumors" (2008) - by Henning Dralle and Orlo H. Clark.
Research and articles:
- "Adrenocortical Carcinoma: Recent Advances in Basic and Clinical Research" (2018) - by Wengen Chen et al. The article was published in Frontiers in Endocrinology.
- "Clinical and molecular genetics of adrenocortical carcinoma" (2020) - by Tobias Else et al. The article was published in the journal Molecular and Cellular Endocrinology.
- "Cushing's syndrome: pathophysiology, diagnosis, and treatment" (2015) - by Andre Lacroix. The article was published in the journal Seminars in Nuclear Medicine.
Literature
Dedov, I. I. Endocrinology: national guide / ed. By I. I. Dedov, G. A. Melnichenko. I. Dedov, G. A. Melnichenko. - 2nd ed. Moscow: GEOTAR-Media, 2021.

