Medical expert of the article
New publications
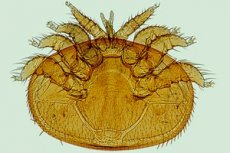
Acariasis
Last reviewed: 12.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Causes acariasis
The generally accepted causes of acariasis are tick bites. Moreover, people are not bitten by adult arthropods, but by their deutonymphs (the larval stage of the tick life cycle, its main parasitic phase).
The main pathogens of acariasis identified to date are representatives of two nomenclature groups of very small (tenths of a millimeter in size) acariform mites: Trombidiformes and Sarcoptiformes.
Some of them are ectoparasites of insects, birds or mammals; some live in symbiosis with their hosts or are commensals, and there are many free-living species. And although the routes of infection are bites that open free access to skin tissue, acariform mites do not need ferritin, which is contained in red blood cells and which blood-sucking parasitiform mites feed on. The food for most acariforms is the decay products of organic matter, that is, they are detritivores.
It is noteworthy that in order to more firmly attach to the host's skin and to allow unhindered "feeding", the larvae of most acariform mites form a special tube (stylostoma) between the chelicerae (oral appendages).
This is what distinguishes them from hematophagous ticks (ixodid, gamasid, argasid), whose bites introduce pathogens of tick-borne encephalitis, borreliosis, vesicular rickettsiosis, coxiellosis, anaplasmosis or babesiosis into the human bloodstream.
The most famous of the acariform mites that affect human skin are the sarcoptera or scabies mite (Sarcoptes scabiei), which parasitizes humans and many families of mammals, and the demodex - a trombidiform mite Demodex folliculorum (subfamily Demodicidae), which is commonly called the eel mite or subcutaneous mite.
Due to the defeat of the sarcoptera, scabies develops, which, in fact, is sarcoptosis acariasis. And the disease provoked by the mite D. folliculorum, dermatologists usually call demodicosis of the skin and very rarely - demodectic acariasis.
Trombidiform mites Pyemotes ventricosus (parasitic on wood-boring insects), Pyemotes herfsi (feeding on the hemolymph of leaf-fly larvae living in oak galls) and triticid mites (Pyemotes tritici), usually breeding during storage of hay, straw, dried legumes and grains, are the causes of acariasis, defined as hay or grain mange.
Two species of mites, Psoroptidia and Suidasia pontifica, belonging to the sarcoptiform group, cause acariasis of the ear.
Acariasis dermatitis is caused by the sarcoptiform mite Glycyphagus domesticus or the chigger mite Trombidium ferox, which parasitizes birds and rodents. Skin lesions caused by the grain mites Tyroglyphus farinae or Glycyphagidae destructor may be called flour itch or tyroglyphosis.
As experts from the European Association of Acarologists note, perhaps the most numerous population of pyroglyphid dermatophagoides – Dermatophagoides farinae, D. microceras and D. pteronyssinus, called dust mites, live in every living space, feeding on the decomposition of dead and exfoliated cells of the stratum corneum of human skin. They lead to the development of acariasis dermatitis, called dermatophagoidosis.
When the route of infection is inhalation, there may be an acariasis allergy. Immunologists have proven the involvement of these mites in the sensitization of the human body and their high cross-allergic reactivity with the mold mite Tyrophagus putreseltiae and mites of the subfamily Glycyphagidae living on seeds and grain products.
Of the blood-sucking parasitiform mites, the gamasid mites Dermanyssus gallinae, parasites of poultry and pigeons, are considered to be involved in the occurrence of such a type of acariasis in humans as dermanissiosis.
Risk factors
Among the risk factors for the development of acariasis, doctors primarily note a decrease in the body's overall resistance.
You can get acariasis: when keeping poultry or working in poultry farming; during work in grain storage facilities and warehouses (where flour and cereals are stored and packaged); during haymaking or harvesting of grain crops.
It should be borne in mind that any pet in an ordinary city apartment is a potential carrier of acariform mites, not to mention rats running around garbage dumps.
And even when there are no animals or birds in the house, there remains such a huge reservoir of pathogens for allergic and dermatological acariasis as dust.
Pathogenesis
If, in the case of transmissible parasitic diseases, blood-sucking parasitiform ticks transmit infections from an infected warm-blooded organism to a healthy one (including humans), then the pathogenesis of acariasis is completely different.
When an acariform tick bites, an enzyme is released that performs two functions at once: it paralyzes the victim (another insect or small vertebrate) and, at the site of the bite, breaks down the substances in its tissues to a state that allows the tick to suck it in and thus satisfy its nutritional needs.
The scabies-causing Sarcoptes scabiei has a special feature: when the female tick bites the skin, it secretes an enzymatic liquid (presumably saliva), which softens the stratum corneum and facilitates the tick's penetration deeper into the skin. Further penetration leads to the formation of a tunnel burrow in the stratum corneum. Here, S. scabiei feeds on tissue fluids and lays eggs, filling the burrow to the very bottom.
Regardless of the type of mite that penetrates human skin (thrombidiform or sarcoptiform), the mechanism for the development of dermatitis is the same: activation of innate local immunity in response to the penetration of foreign proteins (antigens) through the epidermal barrier.
Such antigens expressing PRR and PAR-2 receptors of the epidermis are the collagen protein actinidin (a component of the chitinous shell of ticks), the enzymes they secrete (anionic or cysteine proteases), as well as the products of their vital activity.
In response to infection, keratinocytes of the stratum corneum (which are proinflammatory effector cells) produce more protective peptides (β-defensins, cathelicidins and RNase) and proinflammatory cytokines and chemokines. All immune cells present in the dermis are mobilized: mononuclear phagocytes (Langerhans dendritic cells), mast cells and macrophages, B and T cells and plasmacytoids, fibroblasts and natural killers.
Sensitization and acariasis develop in a similar manner when dust mites enter the mucous membrane of the respiratory tract.
Symptoms acariasis
The first signs of acariform mite bites and subsequent acariasis dermatitis appear within 24 hours in almost the same way: hyperemic areas causing intense pruritus (itching sensation). The skin area swells, may be hot to the touch, and sometimes there is a burning, numbness, or tingling sensation.
After some time, the following symptoms of acariasis are visualized on the skin: against the background of redness, often acquiring the character of erythema, small transparent bubbles (vesicles) filled with exudate (serous fluid) are formed; vesicles can transform into pustules - round-shaped cavities with purulent contents, protruding above the surface of the epidermis.
Due to scratching, the elements of the rash are destroyed, the exudate, pouring onto the skin, causes additional irritation and expansion of the inflamed area. Crusts appear, areas of weeping are possible.
The symptoms of sarcoptic acariasis are described in detail in the publication – Scabies.
Bites from the mites Pyemotes ventricosus or Pyemotes tritici, the causative agents of grain scabies, manifest within 10 to 24 hours as itchy, erythematous lesions (including the neck, arms, shoulders, and upper torso) with raised, firm papules topped by a vesicle that then becomes cloudy with purulent exudate. The rash resolves within five to seven days, and in some cases, within two weeks. About 20% of patients develop associated symptoms of fever, runny nose, and wheezing.
For more information on the symptoms that occur when house dust mites enter the respiratory tract, see the article Dust Mite Allergy.
Complications and consequences
The most common complications of skin lesions caused by acariform mites are secondary bacterial infections (staphylococcal and streptococcal), which develop at the site of scratching and lead to purulent inflammation – pyoderma.
And pyoderma can be complicated by the formation of local abscesses that affect the deep layers of the dermis and subcutaneous tissues.
Acariasis associated with dust mites complicates the functioning of the respiratory system, causing chronic pulmonary eosinophilia.
Diagnostics acariasis
The only tests performed if mite dermatitis or sensitization is suspected are tests for IgE levels, i.e. immunoglobulin E in the blood.
Molecular methods for identifying mite species are not available to dermatologists. In addition, many acariform mites, such as the Pyemotes subfamily (0.1-0.2 mm long), are impossible to see with the naked eye, and the chances of finding them at the site of the bite are minimal; in addition, they leave long before the onset of the inflammatory reaction.
Therefore, for diagnostic purposes, it is important to detect the presence of ticks on animals, even if they are not found on the affected person.
Instrumental diagnostics of acariasis caused by some types of mites is possible: skin scrapings are examined under a microscope. Moreover, parasites are most often found at the edges of lesions, in the area of peeling and crusts. Ear mites can be seen with an otoscope.
A dermatologist conducts an examination of the skin, and a pulmonologist conducts an examination of the lungs and bronchi.
Differential diagnosis
The most difficult thing is differential diagnostics, since it is necessary to distinguish acariasis from urticaria and a number of allergic dermatoses, as well as from herpes or erythema multiforme. And to identify an allergy to ticks, special tests are required, which are carried out by an allergist.
Who to contact?
Treatment acariasis
The main goal of treating acariasis is to relieve itching and inflammation, as well as to prevent secondary bacterial infections.
Washing the affected area with soap and water and applying ice packs (for 5-10 minutes every 45-60 minutes) can help reduce itching and redness of the skin.
The main drugs used in the treatment of acariasis dermatitis are symptomatic. It is possible to take antihistamines orally, which, read - Tablets for itchy skin.
To lubricate the rash, use salicylic or menthol alcohol, emulsion with benzyl benzoate, cream or lotion Crotamiton. External agents are represented by: sulfur and zinc ointments, Dermadrine, Dexpanthenol, various ointments with corticosteroids. More details in the publications:
Folk remedies
Folk remedies include: compresses from raw white cabbage leaves, raw grated potatoes, aloe juice, plantain, propolis dissolved in water.
It is recommended to lubricate the rash with calendula or propolis tinctures, concentrated soda solution, mumiyo solution, and lemon juice.
Herbal treatment involves compresses with a decoction of calendula flowers, creeping wheatgrass roots or elecampane - with the addition of a few drops of chamomile, lavender, and tea tree oil.
Prevention
The very high reproductive potential of acariform mites, their microscopic size and high ability to disperse by wind make it difficult to control their populations and prevent acariasis.
Prevention recommended by the World Health Organization for humans: avoiding contaminated areas and places where these arthropods may live, and using repellents and insecticides based on diethyltoluamide.
Forecast
Timely therapy leads to complete cure of skin manifestations of acariasis, the prognosis is favorable. With weakened immunity, acariasis sensitization takes a chronic form.


 [
[