Medical expert of the article
New publications
Melioidosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Melioidosis (or Vitmor's disease) refers to acute infectious diseases of bacterial etiology; often manifests as community-acquired pneumonia or sepsis; high level of mortality. Bacteria are widespread in soil and water in the tropics. They enter the human body by direct contact with a contaminated source, especially during the rainy season.
Epidemiology
Peculiarities of the spread or epidemiology of melioidosis are well studied: the infection is endemic in Southeast Asia. Thus, in Thailand there are 36 cases of melioidosis per 100,000 people. In Australia, this bacterium is picked up in tropical climate zones - in the north of the continent. In many Asian countries, the bacterium B. Pseudomallei is so common that it is found even in laboratory cultures. About 75% of registered cases of melioidosis are detected during the rainy season.
Now melioidosis is increasingly diagnosed in Latin America, some cases (among tourists and immigrants) are noted in the US, Africa, the Middle East.
Ways of B. Pseudomallei infection include direct contact with water and soil and infection through skin lesions (abrasions, cuts, etc.), drinking contaminated water, inhaling dust. Seasonal monsoon showers significantly increase the aerosolization of bacteria, as a result of which they also get through the upper respiratory tract. Several cases of human-to-human transmission have been reported.

Causes of the melioidosis
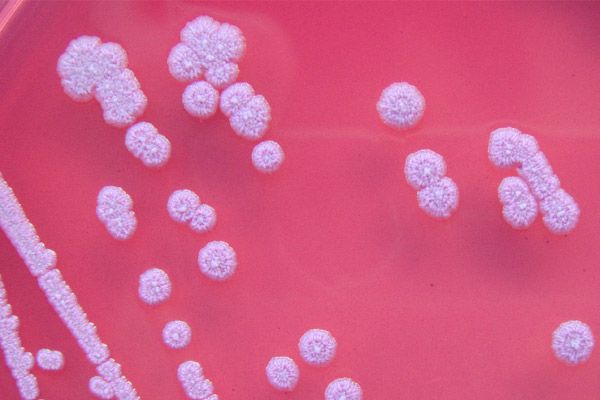
The causes of melioidosis are the infection of a human Burkholderia pseudomalli (Burkholderia pseudomallei) bacterium, which is classed as a Proteobacteria, a class of Betaproteobacteria.
The causative agent of melioidosis is a pathogenic gram-negative bacterium, a rod-shaped aerobic. This bacterium intracellular, due to the presence of filament (filamentary flagellum) is sufficiently mobile.
Burkholderia pseudomallei is saprotroph, that is, it lives in waterlogged soil and water, where it receives nutrients from rotting organic matter. Bacteria can infect many animals (including agricultural and domestic animals) and birds, and their feces further contaminate soil and water. Not so long ago, this proteobacteria were found in dolphins and sea lions in the oceanarium of the Hong Kong Ocean Park.
Pathogenesis
The pathogenesis of this infectious disease is associated with the destruction of bacterial B. Pseudomallei tissue macrophages and the suppression of phagocyte-produced immune C-proteins, in particular, beta-globulin C3b. And thus, bacteria can neutralize the attacking (lysis) membrane complex and, moreover, destroy membranes of endocytic phagolysosomes that are formed to neutralize antigens.
In addition, B. Pseudomallei is able to polymerize the structural protein actin and spread from cell to cell to form giant multinucleate cells. Hematogenous and lymphogenous pathogen melioidosis falls into various organs and leads to the development of inflammation and necrosis.
Microbiologists note that the bacterium Burkholderia pseudomallei is a "random pathogen", because it does not need other organisms for reproduction and replication of RNA, and for a bacterium, human infection is an "evolutionary dead end".
Physicians have identified the main risk factors for melioidosis: diabetes, chronic renal failure, high alcohol consumption, liver diseases (cirrhosis), thalassemia, chronic lung diseases, HIV and other immunosuppressive conditions.
Symptoms of the melioidosis
The incubation period of melioidosis varies depending on the number of bacteria in the body and the route of infection and can range from a few hours to 14-28 days. Much faster the first signs of the disease is manifested in the presence of risk factors (listed above).
The disease has an incredibly diverse list of clinical manifestations, including such symptoms of melioidosis as: fever, chills, cough, shortness of breath, headache, drowsiness, chest and abdominal pain, weight loss, seizures, enlarged spleen and liver, bladder inflammation, prostate gland, joints, soft tissues, regional lymph nodes, etc.
Forms
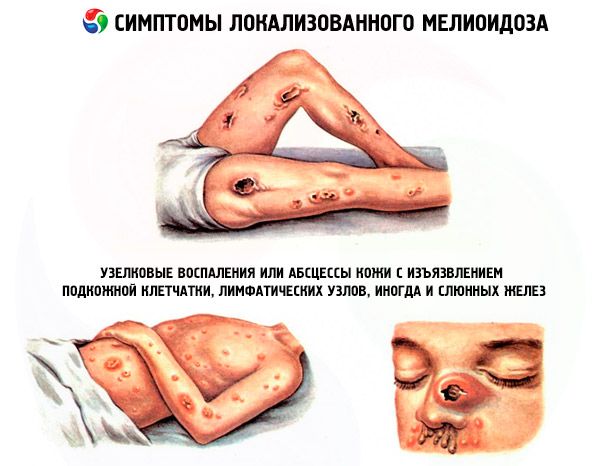
Infectionists distinguish such types of meliosis (more precisely, the clinical forms of its manifestation): localized, pulmonary, septic. There is also acute, subacute, chronic, recurrent and latent (latent) forms of the disease.
Manifestations of localized (local) meliosis : ulcers, nodular inflammation or abscesses of the skin with ulceration of subcutaneous tissue, lymph nodes, and sometimes salivary glands. The first signs are fever and muscle pain in the affected area. In this case, subacute infection (usually focal) can affect almost any system of organs and be a source for subsequent bacteremia.
Symptoms of melioidosis of the most common pulmonary form are all signs of purulent bronchopneumonia, up to pulmonary abscesses and purulent pleural effusion. Characteristic manifestations include fever with fever, headache and pain in the chest, coughing (unproductive or with phlegm), loss of appetite, muscle soreness.
In septic form - systemic infection in the blood - a life-threatening clinical picture of sepsis and septicotemia develops, often causing concomitant pneumonia and abscesses of the liver and spleen. Infection can spread to bones, joints, skin, soft tissues. With this form of the disease, the infection quickly leads to the terminal stage, which ends with septic shock and death within 7-10 days after the onset of symptoms.
Despite the fact that the acute forms are most typical for this disease, there are many cases of latent infection, which proceeds asymptomatically, with reactivation within a year. And with latent melioidosis, symptoms can appear several years after infection, usually in combination with a change in the immune status. Researchers believe that B. Pseudomallei bacteria can persist for a long time in macrophages in an inactive state.
Complications and consequences
The consequences and complications of melioidosis vary depending on the severity of the lesion, as well as timely treatment. In the case of acute severe melioidosis, lethality ranges from 30 to 47%; in cases of belated treatment of septicemia, mortality exceeds 90% (with septic shock - about 95%). According to Nature Reviews Microbiology, with adequate medical care, mortality is much lower, for example, the death rate of patients with B. Pseudomallei in Australia is 19%.
Diagnostics of the melioidosis
In domestic practice, the diagnosis of septic forms of melioidosis is considered "problem-free" if it turns out that the patient was in endemic regions.
According to foreign epidemiologists, the diagnosis of meliosis is difficult due to nonspecific symptoms and requires laboratory tests for the presence of Burkholderia pseudomallei in the body. To do this, patients are taken blood tests, sputum, urine or pus.
The blood test for acute forms of melioidosis can be negative, but this does not exclude the disease. A common cause of difficulties in establishing the correct diagnosis is the practical lack of approved diagnostic reagents for immunological or molecular diagnostic tests for the presence of B. Pseudomallei.
As the Journal of Medical Microbiology writes, even in cases where melioidosis is endemic, difficulties arise in laboratory diagnostics, and the causative agent of this disease can be mistakenly identified as Chromobacterium violaceum, Burkholderia cepacia or Pseudomonas aeruginosa (Pseudomonas aeruginosa).
To determine the bacterium, instrumental diagnostics can not, but it is used to assess the condition of the affected organs: chest X-ray, ultrasound or CT of visceral organs is performed.
Differential diagnosis
Differential diagnostics of the pulmonary form of melioidosis is very important, because it can look like both soft bronchitis and severe pneumonia.
Who to contact?
Treatment of the melioidosis
To date, the only effective treatment for melioidosis is a long course of antibacterial drugs. The initial treatment consists in intravenous administration of antibiotics within 14 days.
The causative agent of melioidosis shows resistance to many antibiotics, in particular, macrolides and preparations of the group of aminoglycosides, tetracyclines and fluoroquinolones.
At the initial stage of the disease, the choice drugs are the antibiotic of cephalosporins Ceftazidime (Zaceph, Orzid, Kefadim, Sudocef and other trade names) and beta-lactam antibiotic Meropenem (Meronem, Imipenem).
Without antibiotics, the septic form of melioidosis in 9 cases out of 10 ends lethal. The use of antibacterial drugs reduces the number of deaths in uncomplicated cases by 9 times, and cases of bacteremia or severe sepsis - by only 10%.
Typically, the body responds to appropriate antibiotic therapy rather slowly: on average, fever can last up to 6-8 days.
As noted by epidemiologists, 10-20% of patients in endemic regions have relapses (due to repeated infection or initially multifocal form of the disease), therefore treatment of melioidosis must necessarily include eradication therapy, the purpose of which is to completely destroy B. Pseudomallei in the body.
To do this, with the next 8 weeks orally, Trimethoprim and Sulfamethoxazole (or a combination of them, Co-trimoxazole) are taken orally. Less effective are Doxycycline (Vibramycin, Doxacin) and the combined beta-lactam antibiotic Amoxiclav (amoxicillin + clavulanic acid).
Prevention
Currently, specific prevention of melioidosis is not possible, since there are no vaccines against B. Pseudomallei yet.
Since the transmission of infection from person to person is an emergency (and is in doubt among specialists), the main way is to avoid contact with soil and standing water in endemic regions. So, in the countries of South-East Asia people working in rice fields are warned about a dangerous infection and are recommended to work in rubber boots and gloves (so that the bacterium does not penetrate the body through small skin damage).
If there is any damage to the skin, it is necessary to cover them with a waterproof bandage and avoid contact with dirt or water in the areas where the disease is present.
It is necessary to wash your hands only in clean water and boil any water used for drinking and cooking. Vegetables and fruits are also recommended to wash with boiled water. It is established that the pathogenic bacterium that causes melioidosis dies when water is heated above + 74 ° C for 10 minutes.
For the prevention of B. Pseudomallei, disinfectants could be used, but as it turned out, the bacterium does not react to phenolic drugs and perfectly tolerates the usual bactericidal concentrations of chlorine ...
Forecast
Melioidosis is an infectious disease, often leading to fatal consequences, so doctors define its prognosis as unfavorable. But antibiotics can save you from death.
The latest issue of the journal Nature Microbiology reports data: 165,000 cases of this disease are recorded worldwide every year.
 [42],
[42],

