Ultrasound signs of pathology of muscle tissue
Last reviewed: 19.10.2021

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Pathology of muscle tissue.
Injury of muscles as a result of compression, shock (concussion). As a result of external compression of the muscle tissue, a muscle contusion occurs on the bone. With longitudinal scanning, the damage area looks like a cavity with uneven contours and echogenic contents. Healing occurs slowly, with the formation of coarse scar tissue and a significant loss of muscle function afterwards. Approximately 20% of patients with this type of trauma have ossifying myositis.
Stretching. The first stage of muscle damage is overexertion. Usually tensile damage less than 5% of all fibers of the cross section of the muscle. Clinically, the patient can not accurately indicate the pain point, complaining of the pain in the muscle with contraction. When transverse scanning on sonograms, micro-ruptures are visualized, which look like multiple cystic areas.
With longitudinal scanning, micro-fractures have an elongated shape. On MR tomograms on T2-weighted images, this manifests itself by thickening the muscle and increasing the intensity of the signal due to peripheral edema. Treatment consists in restriction of movement and anesthesia.
Partial break. Partial rupture also occurs as a result of overexertion. In this case, more than 5% of muscle tissue is damaged, but not all over.
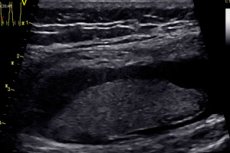
The muscle function is completely absent at the time of injury and returns in part after a while. Unlike stretching, the patient clearly indicates a painful point where, as a rule, there is a swelling. With ultrasound, the integrity of the muscle fibers is clearly seen at the site of the greatest soreness. The damaged area of the muscle tissue is replaced by a hypoechoic hematoma. At the point of rupture, a typical fibrous pattern disappears. When pressure is applied to the sensor, it is possible to visualize the floating ruptured ends of the muscle fibers. The contraction of the muscle allows you to differentiate the damaged muscle from the echogenic hematoma (in the late stage). When studying in dynamics, a hyperechoic granulation tissue and regenerating muscle fibers appear at the site of the rupture. On T2-weighted images, this is manifested by muscle thickening and increased signal intensity due to edema, hemorrhage, perifascial edema, or hemorrhage. Sometimes there is a defect in muscle tissue in the form of a hyperintense band. If there are significant gaps, a surgical restoration of the integrity of the muscle fibers may be required.
Complete rupture. Full muscle rupture is less common than partial ruptures. Muscle ruptures occur at the site of the muscle transition in the tendon. At the clinic, full gaps are similar to partial ones. There is a complete loss of muscle function. The severed proximal end of the muscle contracts and can be palpated. With complete rupture, there is a complete absence of muscle fibers, especially noticeable when compared with the contralateral side.
The muscle shrinks and a bruise forms in its place. In transverse scans, the contracted echogenic muscle is surrounded by a hypoechoic rim. On the frontal sections during the construction of a three-dimensional reconstruction of the pathological zone, one can visualize the gap all along. Treatment consists in surgical restoration of the integrity of the muscle.
Healing of muscle ruptures. Healing of muscle ruptures can take from 3 to 16 months, in proportion to the degree of rupture. Muscles have a good ability to regenerate. Large muscle ruptures are accompanied by both regeneration and scar tissue formation. The goal of therapy is to maintain the regeneration process and suppress scar formation, which reduces regeneration. The role of ultrasound is to measure the rupture and divergence of muscle fibers, as well as to determine the stage of rupture.
The initial changes consist in increasing the echogenicity of muscle tissue in the region of ruptured ends, as well as in increasing the size of this zone, which can be easily traced echographically. In the future, more and more manifested pinnate muscular structure with a reduction in the size of the hematoma. Ultrasound monitoring of the restoration of the muscular structure is very important. With it, you can control the timing of the onset of physical activity. Early recovery of physical activity leads to repeated injuries. A longer restriction of mobility leads to excessive scarring. The task of ultrasound examination also includes evaluation of scar tissue at the site of the rupture. In case of muscle injuries as a result of concussion, the scar has a stellate or irregular shape, whereas with fractures as a result of overstretch, the scar is linear. The risk of repeated trauma increases with a significant size of fibrous tissue, which echographically looks like a local zone of increased echogenicity in the structure of muscle tissue. The strength of the muscle decreases in proportion to the size of the scar tissue. One of the complications after muscle rupture is the formation of muscle cysts. Treatment consists in excision of cysts.
Hematoma. In acute stage, the echogenicity of the hematoma is comparable to the echogenicity of the muscle. After 3 days ehogennost hematoma decreases. Due to lysis, late bruises look almost anehogennymi with the presence of filaments of fibrin.
Sometimes, in an unfavorable course, an abscess may develop that is characterized by the presence of a hypoechoic region with hyperechoic inclusions and pronounced perifocal blood flow.
On MP-tomograms, the intensity of the signal from the hematoma depends on its prescription. Intensity of the hematoma signal varies: from hyperintensive in the first day to hypointense - in the second; returns again to hyperintense by the end of the first week and lasts up to three weeks; then a month later it becomes hypo-intensive again. Such changes arise due to the conversion of hemoglobin to oxyhemoglobin, then to deoxyhoglobin, methemoglobin, and hemosiderin with ferritin. Acute hematoma (1-4 days) has a medium and low intensity signal on T1 and T2-weighted images. Subacute hematomas (4-7 days) are hypertensive on T1 - weighted images, like fat. Therefore, using fat-suppression scanning programs, it is easy to differentiate fat from blood.
It should be remembered that due to the podkravlivaniya hematoma may be observed heterogeneity of the signal intensity. On T2-weighted images subacute hematomas are hypointensive. In old hematomas (days 14-21), due to the conversion of iron from methemoglobin to hemosiderin and ferritin, the walls have a low intensity on T1 and T2-weighted images and appear on MP-tomograms as a hypo-intensive "halo" around the hematoma.
Myositis. It is an inflammation of the muscle tissue that can result from trauma, infection or a systemic disease. In viral infections, myositis is manifested by myalgia. Inflamed muscle is sharply painful, enlarged in size, dense to the touch. Muscle fibers become hyperechoic and in comparison with the contralateral side. Fibrous interlayers, stretched by inflammatory exudates, become hypoechoic. With ultrasound angiography, there is an increase in the vascularization of the inflamed muscle. Perifocal can be marked with lymphadenopathy. In the future, an abscess can form - then the process is called pyogenic myositis. A typical picture: a cavity in the center of the muscle tissue with the presence of non-uniform contents. Clinical signs: pain, fever, leukocytosis, increased ESR.
Atrophy of the muscle. Muscular atrophy arises from a variety of causes. Chronic dysfunction of the joint, denervation, myopathy - the most common causes leading to atrophy. It manifests itself in a decrease in the volume of muscle tissue, when compared with the contralateral side. With ultrasound, the increase in echogenicity occurs due to fat infiltration. On MR tomograms, fatty infiltration of muscle tissue is also clearly visible on T1-weighted images.
Muscle Fascia ruptures. With overstretching, there are ruptures of the muscular fascia. For some muscle groups, this type of damage is very specific. For example, muscular-aponeurotic lesions between the gastrocnemius and soleus, soleus and the muscle of the long flexor of the big toe. The fracture zone is filled with a linear hematoma along the aponeurosis. A characteristic ultrasound is a violation of the orientation of the fibrous fatty interlayers in longitudinal scanning. This type of rupture is very often accompanied by venous thrombosis.
Herniated muscles. Fascial defects are manifested in the form of local protrusions of muscle tissue. Chronic contraction of the muscle most often leads to the formation of hernia, less common post-traumatic and postoperative hernia. In ultrasound examination, a fascial defect and hernial protrusion of the muscle can be detected. Often such hernias are detected at the site of perforation of the muscle with a vascular-neural bundle. For example, on the outer surface of the lower part of the knee joint at the site of the exit of the peroneal nerve.
Hernias of the white abdominal line, inguinal, femoral can be detected. The pressure of the sensor on the skin in the study of hernias should be minimal.
Thickening of muscular fascia. Thickening of the muscular fascia can also affect muscle function. "Split Shin" is a disease in which there is pain in the muscles of the anterior region of the shin after excessive physical exertion.
"Knee runner". The friction syndrome that occurs in the orotibial tract is another pathology of the fascial vagina, the so-called "runner's knee". Clinically it is accompanied by pain in the lateral part of the knee joint at the site of the passage of the fibers of the orotibial tract through the lateral condyle of the thigh. Running with obstacles or over rough terrain leads to the development of this syndrome. It manifests itself in the thickening of the fibers of the fascia or orotibial tract, reducing their echogenicity immediately after running. In a calm state, these manifestations can subside.
Fractures of the plantar fascia. Runners for long distances, marathon runners often suffer from pain in the feet. Heel pain occurs with fasciitis, in which heel spurs are often found. The fascia thickens in the place of attachment to the calcaneal tubercle.
This process, as a rule, is two-sided, so comparison with the contralateral side does not give a result. Tears appear in the middle of the fascia and look like a hypoechogenic defect. It is necessary to differentiate the ruptures from plantar fibromatosis.
The latter appears as a spindle-shaped thickening of the fascia with preservation of the fibrous structure. Plantar fibromatosis may occur in patients with Dupuytren's contracture, Peyronie's disease, superficial fibromatosis.
Useful links
Muscles https://en.wikipedia.org/wiki/%D0%9C%D1%8B%D1%88%D1%86%D1%8B

