Hypertensive heart failure
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hypertensive heart failure (HFH) is a form of heart failure that develops as a result of chronic hypertension, which is high blood pressure. Hypertension is a condition in which the pressure in the arteries remains elevated over a long period of time. The constant exposure of the heart to high pressure can overload it and impair its contractile function, which in turn causes the development of heart failure.
The GSN is characterized by the following features:
- Enlarged heart: In hypertension, the heart can become enlarged and thicker (hypertrophy). This occurs as an adaptive response to increased workload, but over time the thickened heart walls may become less efficient at contracting.
- Deterioration of contractile function: Hypertension can lead to a decrease in the heart's ability to contract and pump blood efficiently. This deterioration in contractile function can cause blood to stagnate in organs and tissues.
- Congestion: HCV can cause blood to stagnate in the lungs and other organs. This can be manifested by swelling, shortness of breath, fatigue, and other symptoms.
- Increased risk of heart complications: HSAs increase the risk of heart complications such as myocardial infarction (heart attack), arrhythmias, and other cardiovascular problems.
Symptoms of HF may include shortness of breath, fatigue, swelling (usually in the legs), increased fatigue with physical activity, and other signs of heart failure. Treatment for GSH includes controlling blood pressure with medication, managing symptoms and body fluid levels, and regular follow-up with your doctor. It is important to follow your doctor's recommendations and maintain a healthy lifestyle to manage and prevent progression of GSH.
Pathogenesis
The pathogenesis of hypertensive heart failure (HHF) involves a complex set of mechanisms and changes that occur in the heart and blood vessels against the background of long-term hypertension (high blood pressure). Here are the main aspects of the pathogenesis of HFH:
- Myocardial hypertrophy: Under the influence of constantly increased pressure on the ventricular walls of the heart (hypertension), the heart muscle (myocardium) begins to increase in size and thicken. This phenomenon is called myocardial hypertrophy and is an adaptive response to increased workload. However, over time, hypertrophy can lead to impaired myocardial structure and function.
- Deterioration of contractile function: Myocardial hypertrophy can lead to a deterioration in the heart's ability to contract and pump blood efficiently. The heart becomes less able to maintain normal blood flow and provide oxygen and nutrient-rich blood to organs and tissues.
- Congestion: Decreased contractile function of the heart can cause blood to pool in the lungs and other organs. Blood stasis can cause shortness of breath, swelling, enlarged liver, and other symptoms.
- Increased strain on the heart: Hypertension places a constant strain on the heart, as it must overcome increased pressure to pump blood. Over time, this can lead to wear and tear on the heart muscle and deterioration of its performance.
- Vascular remodeling: Hypertension also affects vascular structure and function. High blood pressure can cause damage to the vascular wall, which impairs blood pressure regulation and increases the workload on the heart.
- Other risk factors: Hypertension may increase the risk of atherosclerosis (cholesterol deposits) in the blood vessels, which further impairs blood flow and can lead to cardiac complications.
As GSH progresses, the heart becomes less able to perform its function effectively, which can lead to the development of cardiac symptoms and complications. Timely diagnosis and treatment of hypertension is important to prevent the development of CHD and improve prognosis.
Symptoms of the hypertensive heart failure
Symptoms of hypertensive heart failure can vary depending on the degree and severity of the disease. Some common symptoms include:
- Dyspnea(respiratory failure): Dyspnea may be one of the earliest and most characteristic symptoms of GSH. Patients may have difficulty breathing, especially with physical activity and at night (nocturnal dyspnea) when they go to bed.
- Edema(swelling of the legs and/or abdomen): Increased pressure in the capillaries can cause fluid to leak into surrounding tissues, resulting in swelling, most commonly in the lower legs and feet. In more severe cases, abdominal edema may develop.
- Fatigue and weakness: Patients with GSH may feel tired and weak, especially when performing physical activities.
- Increasedfatigue: Increased cardiac workload and decreased cardiac efficiency may cause increased fatigue in patients.
- Increased heartbeat (tachycardia): The heart's attempt to compensate for insufficiency may result in increased heart rate.
- Heart pain (angina): Some patients may experience heart pain or pressure pain (angina), especially with physical activity.
- Loss of appetite and nausea: Patients may experience loss of appetite, nausea, or vomiting, which is associated with decreased blood flow in the gastrointestinal tract.
- Decreased urine output: GSH can lead to deterioration of kidney function, which can cause decreased urine output and body fluid levels.
- Insomnia and Anxiety: Patients may experience insomnia and anxiety, especially in association with shortness of breath and discomfort.
All of these symptoms can worsen over time and with additional medical problems. HFH requires careful observation, treatment, and blood pressure monitoring. If you suspect hypertensive heart failure or are experiencing similar symptoms, be sure to see your doctor for diagnosis and treatment.
Stages
Hypertensive heart failure can go through several stages, and their evaluation helps to determine the severity and nature of the disease, which is important for choosing the right treatment strategy and managing this condition. The following stages of hypertensive heart failure are commonly recognized:
- Stage I (Class I): In this stage, patients may have hypertension but do not yet show symptoms of heart failure. Heart function usually remains normal, and patients may have no problems with physical activity. However, high blood pressure may increase the risk of developing heart failure in the future.
- Stage II (Class II): In this stage, patients may begin to show the first symptoms of heart failure, such as shortness of breath and fatigue with physical activity. Heart function may still remain relatively normal at rest, but becomes less effective with exercise.
- Stage III (Class III): In this stage, the symptoms of heart failure become more obvious and bothersome. Patients may experience shortness of breath, even at rest, and fatigue with minor physical exertion. Heart function decreases and blood flow becomes less efficient.
- Stage IV (Class IV): In this stage, the symptoms of heart failure become very severe. Patients may experience shortness of breath and fatigue even at rest. Heart function is severely compromised and not enough blood reaches the tissues and organs, which can lead to serious complications.
Complications and consequences
Hypertensive heart failure (HFH) can lead to a variety of complications that can be dangerous to your health and require additional treatment and management. Some of the major complications of HFH include:
- Acute Heart Failure: Under the influence of developing HFH, the heart may not be able to pump blood and this may lead to acute heart failure, which may require hospitalization and intensive treatment.
- Arrhythmias: Changes in the structure of the heart and its electrical activity can cause arrhythmias such as atrial fibrillation and other irregular heart rhythms.
- Myocardial infarction (heart attack): Hypertensive heart failure increases the risk of myocardial infarction, especially in the presence of vascular atherosclerosis.
- Swelling: Blood stagnation in the lungs and other tissues can cause swelling, which can lead to difficulty breathing, reduced quality of life, and complications.
- Organ damage: GSH can have a negative impact on various organs and systems such as the kidneys, liver and others, which can lead to their dysfunction.
- Coronary heart disease: Increased stress on the heart and blood vessels increases the risk of coronary heart disease, which can include angina and angina.
- Cardiac valvular abnormalities: GSH can cause changes in the structure and function of the heart valves, which can lead to valvular abnormalities.
- Thrombosis and embolisms: Increased risk of thrombosis (blood clots) and embolisms (clots breaking off and traveling) can lead to heart attacks and strokes.
- Renal disease: GSH may cause deterioration of renal function and lead to chronic renal failure.
- Psychological and emotional problems: Long-term illnesses can cause stress, depression and anxiety in patients.
Diagnostics of the hypertensive heart failure
Diagnosis of HFH requires a comprehensive approach, including clinical evaluation, laboratory and instrumental investigations. Here are the main methods of diagnosing hypertensive heart failure:
- Physicalexamination and history taking: The doctor examines the patient and discusses his or her symptoms and medical history. It is important to learn about the presence of high blood pressure and other chronic conditions.
- Blood pressure measurement: The main sign of hypertensive heart failure is a persistent increase in blood pressure. The doctor measures the patient's blood pressure and monitors its dynamics.
- Laboratory tests: Blood tests may include measuring levels of sodium, potassium, creatinine, and other substances to assess kidney function and electrolyte balance. In addition, measuring levels of markers of heart muscle damage (e.g., troponin) may help detect heart failure.
- Electrocardiography (ECG): An ECG records the electrical activity of the heart and can detect arrhythmias, conduction abnormalities, and signs of thickening of the heart walls.
- Echocardiography (cardiac ultrasound): Echocardiography uses ultrasound waves to visualize the structures and function of the heart. Ultrasound can be used to assess the size and thickness of the heart walls, ventricular function, and to detect signs of diastolic dysfunction (impaired relaxation of the heart).
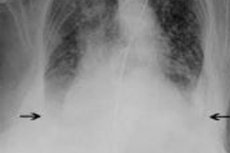
- Chest X-ray: X-rays can help detect signs of lung congestion and heart enlargement.
- MRI (magnetic resonance imaging) and CT (computed tomography) of the heart: These techniques can provide more detailed information about the structure and function of the heart, as well as the condition of the surrounding tissues.
- Cardiac tests: Exercise tests and 24-hour electrocardiogram monitoring can be used to assess cardiac function during physical activity and to monitor blood pressure throughout the day.
Diagnosis of DBS includes not only identifying the presence of this condition, but also assessing its severity and possible complications. Based on the diagnostic results, the doctor will prescribe appropriate treatment and recommendations for the patient.
Treatment of the hypertensive heart failure
Treatment of hypertensive heart failure is aimed at managing blood pressure and easing the strain on the heart. Here are the main aspects of treatment:
- Blood pressure control: The primary goal of treatment of hypertensive heart failure is to lower blood pressure to levels that do not place excessive strain on the heart. This is usually accomplished with antihypertensive medications such as angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, diuretics, and others.
- Treatment of underlying hypertension: It is important to treat the arterial hypertension itself, as it is the underlying cause of hypertensive heart failure. The doctor will choose the most appropriate medication or combination of medications depending on the specific indications and the patient's condition.
- Limit salt: Limiting salt intake in your diet can help reduce swelling and fluid levels in your body, which makes it easier for your heart to function.
- Fluid balancecontrol: It is important to monitor fluid balance to avoid excessive fluid retention in the body. In some cases, it may be necessary to limit fluid intake.
- Supportive therapy: Your doctor may prescribe medications, such as diuretics, to reduce swelling and make it easier for your heart to function. Medications that improve the contractility of the heart muscle may also be prescribed.
- Lifestyle changes: Patients are advised to adopt a healthy lifestyle, including proper nutrition, moderate physical activity, adherence to activity level recommendations, and stress management.
- Regular monitoring and doctor visits: Patients with hypertensive heart failure should see a doctor regularly to monitor the condition, adjust treatment and prevent complications.
Treatment of hypertensive heart failure requires an individualized approach, and the physician will prescribe the most appropriate medications and recommendations depending on the patient's specific clinical situation.
Forecast
The prognosis of hypertensive heart failure (HF) can vary significantly depending on several factors, including the severity of the disease, the effectiveness of treatment, adherence to lifestyle and dietary recommendations, and the presence of other diseases and risk factors. It is important to note that adherence to physician recommendations and management of high blood pressure play a critical role in the prognosis of HF.
The main points that affect the prediction of GOS include:
- Severity of GSH: GSH can be mild, moderate or severe depending on how much the heart is unable to cope due to high blood pressure. A mild form may have a better prognosis than a severe form.
- Blood pressure control: Effective blood pressure control with medication and lifestyle changes can significantly improve the prognosis of HCPs. Uncontrolled high blood pressure can worsen heart health and lead to complications.
- Adherence to treatment and recommendations: It is important that patients with GSH adhere to their doctor's recommendations, take prescribed medications, follow a salt- and fluid-restricted diet, and lead an active lifestyle by adhering to physical activity recommendations.
- Co-morbidities: The presence of other medical problems such as diabetes, obesity, kidney or lung disease may worsen the prognosis of GSN.
- Age and gender: Prognosis may vary depending on the age and gender of the patient.
- Complications: The presence of complications such as arrhythmias, myocardial infarction or thrombosis may worsen the prognosis.
- Effectiveness of treatment: If treatment of GSH does not produce the expected results or does not effectively control blood pressure, the prognosis may be adversely affected.
In general, early diagnosis, strict adherence to treatment and lifestyle modifications, and regular medical follow-up can help improve the prognosis of GSH and prevent its progression. However, it is important to consult with a physician to better assess prognosis and develop a treatment plan appropriate to the patient's specific needs.
Literature used
- Shlyakhto, E. V. Cardiology: national guide / ed. By E. V. Shlyakhto. - 2nd ed., revision and addendum - Moscow: GEOTAR-Media, 2021
- Cardiology according to Hurst. Volumes 1, 2, 3. 2023

