Fatal insomnia
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Fatal insomnia is a rare and incurable neurological disorder characterized by a gradual loss of the ability to fall asleep and maintain a normal sleep pattern. It is undoubtedly one of the most severe and incurable sleep disorders.
Here are the main characteristics of fatal insomnia:
- Gradual sleep disturbance: Patients with fatal insomnia begin to have sleep problems that gradually worsen. They may experience insomnia, stay awake at night, or stay awake for more than a few minutes a night.
- Psychiatric and Neurological Symptoms: As the disease progresses, patients may experience various psychiatric and neurological symptoms such as anxiety, depression, panic attacks, aggressive behavior, hallucinations, and others.
- Physical deterioration: Gradually increasing physical deterioration, including weight loss, muscle weakness and difficulty in coordinating movements.
- Cognitive decline: Patients may also experience problems with memory, concentration, and cognitive abilities.
- Untreatable insomnia: This sleep disorder does not respond to traditional treatments for insomnia, including sleeping pills.
Fatal insomnia is associated with changes in brain structure and abnormalities in a protein known as prion, which plays a role in sleep regulation. It is an inherited disorder and a mutation in the PRNP gene is thought to be the cause.
Causes of the fatal insomnia
Its cause is linked to a mutation in the PRNP (prion protein) gene, which plays a key role in the regulation of sleep and other neurological processes.
This mutation results in the formation of an abnormal form of prion protein (prion protein), which begins to accumulate in the brain and interfere with its normal function. When this abnormal protein accumulates, it causes a loss of the ability to fall asleep and maintain normal sleep. This leads to gradual physical and neurological deterioration.
Fatal insomnia is inherited in families with a mutation in the PRNP gene. If one parent carries this mutation, there is a 50% risk of passing it on to offspring. The disease usually presents in middle age, although there is variation in the age of onset of symptoms depending on the specific mutation.
It is important to note that this is a very rare condition and most people do not inherit the PRNP gene mutation and therefore are not at risk of developing this sleep disorder.
Pathogenesis
Pathogenesis is associated with a mutation in the PRNP gene, which encodes a prion protein (prion protein). Fatal insomnia is a prion disease, and the pathologic mechanism of this disease is a change in the conformation (shape) of the prion protein.
The main stages of pathogenesis:
- PRNP gene mutation: The disease begins with the presence of a mutation in the PRNP gene. This mutation can be inherited or arise by a new (sporadic) mutation.
- Abnormal prion protein: A mutation in the PRNP gene results in the synthesis of an abnormal form of prion protein. This abnormal protein is called PrPSc (prion protein form).
- PrPSc accumulation: PrPSc begins to accumulate in the brain. This process causes the normal prions (PrPC) in the brain to change their conformation and become PrPSc.
- Search for a transparent form of the protein: An important feature of PrPSc is its ability to force normal prions to adopt an abnormal conformation. This process leads to further proliferation of PrPSc in the brain and its accumulation in nerve tissues.
- Neurodegeneration: The accumulation of PrPSc in the nervous tissues of the brain leads to neurodegeneration and neuronal death. This is accompanied by the appearance of characteristic neurological symptoms such as insomnia, loss of coordination, psychiatric disorders, etc.
- Disease progression: Progression of the disease leads to physical and neurological deterioration of the patient. Fatal insomnia is incurable, and patients usually die within months or years after the onset of symptoms.
Pathogenesis is associated with a change in the conformation of the prion protein, which leads to progressive degeneration of nerve tissue and is accompanied by severe neurologic symptoms.
Symptoms of the fatal insomnia
Fatal insomnia (or fatal insomnia) is a rare and severe neurodegenerative disorder that presents with characteristic neurological symptoms. Symptoms may include the following:
- Insomnia: Gradual loss of the ability to fall asleep and maintain a normal sleep pattern is a major symptom. Patients suffer from excessive insomnia and cannot get proper rest.
- Emotional and Mental Disorders: Over time, patients may develop mental and emotional disorders such as depression, anxiety, irritability, and emotional instability.
- Loss of coordination: Patients may experience loss of coordination of movement, clumsiness, and balance problems, which can lead to falls and injuries.
- Hallucinations and delusions: In some cases, patients may develop hallucinations (visions or auditory hallucinations) and delusions.
- Speech difficulties: Gradually deteriorating ability to speak and understand speech can be a problem.
- Memory loss and psychiatric disorder: Patients may experience memory loss and psychiatric disorder, resulting in overall cognitive impairment.
- Decreased ability to perform everyday tasks: Progressive deterioration of neurological function makes it more difficult for patients to perform routine tasks and self-care.
- Weight loss: Loss of appetite and digestive problems can lead to weight loss.
Symptoms become more severe over time, and this deadly disease usually results in the patient's disability and death within months or years of the onset of symptoms.
Stages
Fatal insomnia goes through several stages before reaching its final and severe form. The main stages of fatal insomnia include:
- Prodromal stage: This is the initial stage, which can last months or even years. Patients begin to experience insomnia, anxiety, and emotional changes. Mental instability may manifest in this stage.
- Intermediate stage: Symptoms worsen and patients begin to experience more severe problems with sleep and motor coordination. Emotional and mental disorders may become more pronounced.
- Terminal Stage: In this stage, the symptoms of fatal insomnia become most severe. Patients experience complete insomnia, hallucinations, loss of coordination, and prolonged periods of wakefulness. Loss of cognitive abilities and general decline in health make this stage particularly severe.
- Death: Fatal insomnia eventually leads to the death of the patient, most often from complications related to complete lack of sleep and inability to maintain vital bodily functions.
These stages may vary slightly from patient to patient, and the rate of disease progression may vary.
Forms
Fatal insomnia (or sometimes called Fatal Insomnia Syndrome) has two main forms: sporadic and hereditary. Here is more information about each:
-
Sporadic fatal insomnia:
- This is a rarer form of fatal insomnia.
- Usually occurs in people with no family history of the disease.
- Appears randomly and has no known genetic link.
- Can occur at any age, but more often begins in adulthood.
-
Hereditary fatal insomnia:
- This form is more common and has a genetic basis.
- It is inherited and its cause is associated with a mutation in the PRNP gene.
- Symptoms begin to appear in middle age, but may appear at a younger or older age.
- This form of fatal insomnia is more often associated with familial cases of the disease.
Both forms result in progressive loss of the ability to fall asleep and maintain sleep, eventually leading to physical and mental impairment and then death.
Diagnostics of the fatal insomnia
Diagnosis can be complicated and requires doctors, including neurologists and geneticists, to work together. Here are some steps and methods that can be used in diagnosing this rare disease:
- Clinical History: The physician will gather a detailed medical and family history to identify signs and symptoms and to determine family history of the disease, if available.
- Physical Examination: The physician will perform a physical examination of the patient to identify physical signs and symptoms.
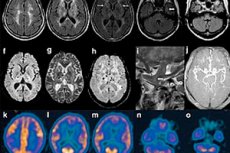
- Neuroimaging: Neuroimaging studies such as magnetic resonance imaging (MRI) and computed tomography (CT) scans may be performed to rule out other neurologic diseases and assess brain health.
- Electroencephalography (EEG): EEG can be used to study the electrical activity of the brain and identify unusual patterns.
- Genetic testing: To confirm a diagnosis of fatal insomnia, genetic testing may be performed to detect mutations in the PRNP gene.
- Liquoral puncture: Examination of the liquor taken by liquoral puncture may show characteristic changes.
- Brain biopsy: An examination of brain tissue may be performed after the patient's death to definitively confirm the diagnosis.
Diagnosis requires a high degree of suspicion and extensive testing to rule out other possible causes of symptoms.
Treatment of the fatal insomnia
There is currently no known treatment for fatal insomnia, and this rare neurodegenerative disease is considered incurable. Because the disease is associated with mutations in the PRNP gene and results in progressive loss of sleep and coordination, the treatment approach is limited to maintaining the patient's comfort and improving their quality of life. Here are some measures that can be taken:
- Symptomatic treatment: Treatment is aimed at managing symptoms. This may include the administration of sedatives and anxiolytics to reduce anxiety and insomnia.
- Support and care: Patients require ongoing medical support and care. Monitoring the condition and providing care for physical degeneration can help to alleviate suffering.
- Psychological support: Psychological support and counseling can be helpful for patients and their families, as the disease has a serious psychological and emotional impact.
- Clinical trials: Research and clinical trials can provide opportunities to find new treatments and therapies.
Forecast
The prognosis of fatal insomnia is usually unfavorable. It is a rare and incurable neurodegenerative disease that results in progressive loss of sleep and motor coordination. Patients eventually face serious physical and psychological problems, and the disease usually leads to death within months or years after the onset of symptoms.
The disease is difficult to treat and there are no ways to prevent its progression. Because fatal insomnia is a rare condition, research and development of new treatments is ongoing, but there are currently no known effective drugs or treatments that can stop the progression of the condition or cure it.
List of authoritative books on somnology
- "Principles and Practice of Sleep Medicine" by Meir H. Kryger, Thomas Roth, William C. Dement (2021)
- "Sleep Disorders and Sleep Promotion in Nursing Practice" - by Nancy Redeker (2020)
- "Why We Sleep: Unlocking the Power of Sleep and Dreams" - by Matthew Walker (2017)
- "Sleep Disorders and Insomnia: A Clinician's Guide to Diagnosis and Treatment" - by Peretz Lavie, Sonia Ancoli-Israel (2018)
- "Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects" - by Sudhansu Chokroverty (2017)
Literature used
- Fatal family insomnia. Rosenfeld I.I. Journal: Modern School of Russia. Issues of modernization. Number: 5 (36) Year: 2021 Pages: 208-209
- Somnology and Sleep Medicine. National manual in memory of A.M. Vein and Y.I. Levin / Ed. By M.G. Poluektov. M.G. Poluektov. Moscow: "Medforum". 2016.
- Fundamentals of somnology: physiology and neurochemistry of the sleep-wake cycle. Kovalzon Vladimir Matveyevich. Laboratory of Knowledge. 2014.

