Atherosclerosis of extracranial branches of brachiocephalic arteries
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Since atherosclerosis is a systemic disease, it can affect large arterial vessels of various localizations, and atherosclerosis of extracranial parts of brachiocephalic arteries is defined when pathological processes are subjected to extracranial (located outside the skull) parts of the arteries that carry blood to the shoulders, neck and head (brain). [1]
Epidemiology
The prevalence of atherosclerotic lesions of extracranial branches of brachiocephalic arteries is estimated at 42-45% of patients with symptomatic atherosclerosis seeking medical care.
According to clinical statistics, stenotic atherosclerosis of brachiocephalic arteries is the second most frequent after atherosclerotic narrowing of the coronary lumen. Stenotic atherosclerosis of brachiocephalic arteries is associated with up to 30% of cases of acute cerebral circulatory failure, and atherosclerotic lesions of carotid arteries lead to stroke in almost half of patients.
And at least a quarter of cases of ischemic stroke of the vertebrobasilar basin (posterior circulation circle) is due to stenotic or occlusive atherosclerosis of vertebral arteries. [2]
According to statistics, the incidence of atherosclerosis has increased significantly over the past few decades. The male population is affected about 3.5 times more often than women. The main age range of patients with diagnosed lesions of extracranial arteries is from 45 years and older.
Statistics are also known for different countries of the world:
- In the United States, the disease occurs in more than 40% of all cardiovascular lesions (many attribute this to the dietary habits of Americans).
- In Italy, this percentage is significantly lower - just over 6%.
- People in African countries experience the disease even less frequently than in European nations and the United States.
- The highest incidence rates are found in America, Australia, Canada, Great Britain, Finland, and the post-Soviet countries.
- The lowest prevalence of atherosclerosis of extracranial arteries is in the Japanese.
Causes of the atherosclerosis of extracranial brachiocephalic arteries
Atherosclerosis of the extracranial branches of the brachiocephalic arteries - arteries of the head and neck - has the same causes as lesions of the intima (inner layer of the vascular wall) of any arterial vessels. Full details:
The brachiocephalic arteries (from Latin brachium - arm, shoulder + Greek kephale - head) are the brachial or brachiocephalic trunk (truncus brachiocephalicus), as well as large branches of this artery. The brachiocephalic trunk is the second branch coming from the aorta, it goes up from its arch through the upper mediastinum to the level of the upper edge of the right sternoclavicular junction, where it divides into the right common carotid artery (arteria carotis communis) and the right subclavian artery (arteria subclavia). The left subclavian artery branches directly from the aortic arch; both subclavian arteries supply blood to the upper body, upper extremities and head.
The common carotid (or carotid) artery, in turn, is divided into internal carotid artery (arteria carotis interna) and external carotid artery (arteria carotis externa), which account for 80% of blood flow to the brain. And from the subclavian arterial vessels branch the right and left vertebral arteries (arteria vertebralis) - paired brachiocephalic arteries, which have three extracranial segments (preforaminal or prevertebral, foraminal or vertebral and extradural or atlantoaxial) and provide blood supply to the upper part of the spinal cord, trunk, cerebellum and posterior part of the brain. [3]
Risk factors
There are many risk factors for the development of this disease, including: dyslipidemia (elevation of certain fractions of cholesterol and triglycerides in the blood), arterial hypertension, disorders carbohydrate metabolism (hyperglycemia, diabetes mellitus), metabolic syndrome, obesity, hyperhomocysteinemia, poor diet (excess saturated fats in the diet), smoking, sedentary lifestyle, hereditary predisposition. [4]
Also see. - atherosclerosis - Causes and Risk Factors
Pathogenesis
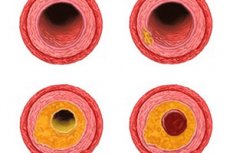
Considering the pathogenesis of atherosclerotic lesions of arterial vessels, experts point to two main components of this pathological process. The first component consists in the formation of cholesterol accumulations in the inner lining of vascular walls in the form of oxidized low-density lipoproteins (LDL) - low-density lipoprotein cholesterol and fibrous tissue cells, which are called atheromatous or atherosclerotic plaques.
The second component is the development of inflammatory response of immunocompetent cells of arterial walls (macrophages, monocytes and T-lymphocytes) to the expression of intercellular adhesion molecules by endothelial cells and damage of vascular intima cells.
The consequence of cholesterol plaques formation is their fibrosis - inflammatory fibroproliferative process, which causes not only thickening of the arterial wall, but also its thickening (reduction of elasticity), because at the next stage of atherogenesis both the affected area of the vessel and the plaque itself undergo calcification (atherocalcinosis). [5]
An important role is played by endothelial damage (increase in its permeability) due to the impact of turbulent blood flow on "critical" areas of brachiocephalic arteries - at their bifurcations and bends.
But the main thing is that, protruding into the lumen of the vessel, plaques narrow it and can even completely block it, causing problems with blood supply. And depending on this, such types of atherosclerotic lesions are distinguished as stenotic atherosclerosis of brachiocephalic arteries (because the narrowing of the vessel lumen is called stenosis) and occlusive or obliterative atherosclerosis of brachiocephalic arteries (occlusion - complete blockage of the vessel lumen), in which blood flow can be blocked. [6]
Symptoms of the atherosclerosis of extracranial brachiocephalic arteries
In most cases, atherosclerosis develops imperceptibly, and its first signs and subsequent symptomatology of atherosclerotic lesions of extracranial sections of the brachial arteries are manifested at a certain degree of narrowing of their lumen.
Thus, the initial atherosclerosis of the brachiocephalic arteries (extracranial brachiocephalic atherosclerosis) is a preclinical asymptomatic stage of the disease, but in some cases there may be sensations of noise in the head and headaches of a nagging nature.
The narrowing of the vascular lumen can be hemodynamically insignificant (not affecting blood flow - hemodynamics) and hemodynamically significant. In the first case hemodynamically insignificant atherosclerosis of brachiocephalic arteries is asymptomatic and is defined by specialists as non-stenotic atherosclerosis of brachiocephalic arteries.
In the second case, it is possible to reduce the lumen of the artery by 50-75%, and this is stenotic atherosclerosis of the brachiocephalic arteries. For example, stenosis of the brachiocephalic trunk leads to the appearance of syncopal episodes - transient loss of consciousness. Atherosclerosis of the carotid arteries causes symptoms such as weakness and dizziness, intense headaches, facial numbness, transient visual or hearing impairment. More information in the material - carotid artery stenosis
Significant stenosis (50% or more) of the proximal segment of the subclavian artery secondary to atherosclerosis causes ischemic problems and leads to the so-called subclavian steal syndrome, which is manifested by pre-syncope and fainting, circulatory disturbances in the hands and arms (the affected hand may be cooler to the touch than the contralateral hand, and the pulse in it may be weaker), impaired coordination of movements, double vision, tinnitus and unilateral hearing loss.
In cases of stenosing atherosclerosis of the vertebral artery, which is more often affected by the prevertebral segment of the vessel, there are vestibulo-ocular symptoms characteristic of vestibulo-atactic syndrome: dizziness, loss of balance headaches, appearance of flies before the eyes.
As the cerebral blood supply deteriorates, vertebrobasilar syndrome or vertebrobasilar insufficiency develops, which is characterized by increased fatigue, sleep and vestibular disorders, short-term syncopal episodes, visual and speech disorders, memory decline in the form of anterograde amnesia. [7]
Stages
Atherosclerotic changes occur in arterial elastic and musculoelastic vessels, depending on the stage: dolipidic, lipoidotic, liposclerotic, atheromatous, and atherocalcinotic.
The dolipid stage is characterized by focal changes in the vascular intima. Such changes occur in the areas of branching or bending of arteries. Microscopic damage to the endothelial layer appears, structures at the level of cells and fibers are affected. There is a violation of the permeability of endothelial cells, intercellular ducts are dilated, caveolae and flattened microthrombi are formed. Fibrinous-serous edema of the inner vasculature is formed.
As the pathologic process worsens, liposclerosis occurs in the area of lipoprotein layering - growth of new connective tissue. As a result, fibrous elements are formed at this stage: flattened microthrombi are organized on the plaque surface, the intima acquires a characteristic "lumpiness".
The atheromatous stage is accompanied by peritubular decay of fat, collagen and elastin fibers, xanthomas and muscle structures. As a result of these processes, a cavity with atheromatous masses (lipid-protein detritus) is formed, delimited from the vascular lumen by a connective tissue layer. As atheromatous processes worsen, complications arise: intrabasal hemorrhages, damage to the connective tissue covering layer, formation of atheromatous ulcerative lesions. Detritus falls into the lumen of the artery, which can provoke embolism. The ulcerative process itself often becomes the base of thrombosis.
The final stage of atherosclerosis of extracranial arteries is the atherocalcinosis stage, the deposition of calcium salts into atheromatous masses, fibrous tissue, and interstitial colloid.
According to statistics, the basis of atherosclerotic changes - fibrous elements - are present in every sixth case of fatal outcome of people over 20 years of age, and in more than 95% of cases of fatal outcome after 50 years of age. More complex pathologic changes and calcification are diagnosed in men starting at age 30, and in women starting at age 40.
Forms
Atherosclerotic changes appear with an imbalance of the main lipid fractions in the blood. The involvement of cholesterol, previously declared the primary "culprit" of atherosclerosis, is also traceable, but cholesterol harm is clearly exaggerated.
Cholesterol is very important for the human body. It is present in the cell membrane, is involved in the production of hormones. But to pay attention to the level and quality of this substance in the blood is really necessary. In the bloodstream, it binds with protein components, resulting in the formation of lipoproteins - complex proteins.
Cholesterol is conditionally divided into "good" - antiatherogenic, and "bad" - atherogenic. Just the atherogenic variant contributes to the development of atherosclerosis of extracranial and other arteries in the body.
The formation of atherosclerotic layers on the inner surface of blood vessels is a rather slow process. Plaques grow both along and across the arterial lumen. Such features of growth are reflected in the classification of atherosclerotic lesions: it is divided into stenotic and non-stenotic variants.
Non-stenotic atherosclerosis of extracranial brachiocephalic arteries is diagnosed if the vascular lumen is blocked by no more than 50% - in particular, this occurs with longitudinal spread of atherosclerotic layers. Such a problem is not badly amenable to drug correction, provided that the diet and lifestyle are changed. In most cases, it is possible to significantly slow down the progression of pathology.
Atherosclerosis of extracranial brachiocephalic arteries with stenosis is noted when the lumen is blocked by more than half. As a rule, in this case, the plaque increases in the transverse direction. This variant is more dangerous, because it quickly and significantly disrupts blood supply to brain structures and often ends in acute circulatory failure of the brain (stroke).
Important: in case of severe arterial stenosis, blocking more than 70% of the vascular lumen, surgical intervention is required. This is the only way to prevent the development of unfavorable and severe complications.
Atherosclerosis of extracranial arteries is accompanied by increasing insufficiency of cerebral circulation. This condition is conditionally subdivided into several degrees:
- Symptoms are absent, sometimes they are absent even against the background of diagnosed atherosclerosis of extracranial vessels.
- Transient ischemic attack develops: initial signs of atherosclerosis of extracranial sections of brachiocephalic arteries appear in the form of focal neurological deficit with complete disappearance of symptoms within 60 minutes. Temporary disorders of cerebral circulation with complete disappearance of neurological symptoms for less than a day are possible.
- The pathology becomes chronic, general cerebral neurological signs or vertebrobasilar deficit appear. Another possible name for this stage is dyscirculatory encephalopathy.
- A previous, ongoing or complete cerebral circulatory disorder (stroke) with focal symptoms present for more than a day, regardless of the presence or disappearance of neurological insufficiency.
Complications and consequences
Lesion of extracranial parts of brachiocephalic arteries can cause ischemic optic neuropathy; and the consequence of stenosing atherosclerosis of the extracranial parts of the brachiocephalic arteries - acute cerebral circulatory failure (reduction of oxygenated blood flow to brain tissue), resulting in transient ischemic attacks, microstrokes and ischemic stroke.
Diagnostics of the atherosclerosis of extracranial brachiocephalic arteries
How the diagnosis of extracranial sections of brachiocephalic arteries is carried out, what laboratory tests (tests) are required, read in the publication - atherosclerosis - symptoms and diagnosis
Instrumental diagnosis includes vascular ultrasound, CT angiography, and magnetic resonance angiography of the brachiocephalic arteries.
What echo signs of atherosclerosis of brachiocephalic arteries are detected during ultrasound vascular ultrasound (ultrasound Doppler), read more in the material - deciphering the results of ultrasound Doppler vascular ultrasound. [8]
Differential diagnosis
Differential diagnosis is performed to exclude arterial narrowing in nonspecific aorto-arteritis and gigantocellular arteritis, muscular fibrous dysplasia, collagenosis, compression syndromes, including vertebral artery syndrome in cervical spine osteochondrosis and others.
Atherosclerosis of extracranial arteries with dominant neurasthenic picture should be timely distinguished from common neurotic and neurasthenic, as well as mild reactive states. These pathologies are similar in the dynamics of symptomatology and interrelation with psychogenic factors.
Neurasthenia due to atherosclerosis demonstrates a neurological picture with focal disorders, a slight intellectual and mental impairment. There is a feeling of fatigue, lethargy, so-called cowardice. Pathological phenomena are usually stable.
Mental spectrum disorders are often very similar to the consequences of head injuries and syphilis lesions. Posttraumatic complications can be identified by the age of the patients, the presence of anamnestic information about the head trauma and its severity. The main symptoms of the consequences of cranial injuries: intense vegetative manifestations, instability of blood pressure indices, non-involvement of the intellectual and mental sphere. Important: cases of combination of atherosclerosis of extracranial arteries and cranial trauma are often found.
To differential diagnostic measures to exclude syphilitic lesions of the brain add serologic reactions (blood and liquor), study the specificity of neurological manifestations.
In the course of differentiation of atherosclerotic changes of extracranial arteries and senile psychosis, attention is paid to personality disorders. Thus, vascular psychosis usually occurs against the background of intellectual and dysmnesic failures.
Senile psychosis is accompanied by an increasing aggravation of intellectual disorder. Already at the initial stage of development, a critical disorder with disinhibition of urges is detected. The appearance of psychosis does not depend on the quality of blood circulation in the brain.
Treatment of the atherosclerosis of extracranial brachiocephalic arteries
To treat non-stenosing atherosclerosis, drugs of the hypolipidemic spectrum - statins (Atorvastatin, Rosuvastatin, etc.) and antiaggregants (Aspirin, Clopidogrel) - are used. [9] More information in articles:
In the presence of symptomatic atherosclerosis, Heparin, Warfarin is prescribed (for 4-12 weeks). Then antiplatelet drugs may be used. For more details see. - atherosclerosis - Treatment
Physiotherapeutic treatment involves the patient performing regular exercise as much as possible.
Physiotherapy for atherosclerosis of extracranial arteries is able to improve blood circulation in the brain, optimize metabolism. Most often "to the rescue" comes to the aid of drug electrophoresis with novocaine, platifylline, eufylline, as well as magnesium-potassium procedures.
Patients suffering from insomnia, mood disorders, phobias are shown electrophoresis with novocaine, iodine, seduxen. In neurasthenia with sleep disorders and arrhythmias, magnesium collar is prescribed, but collars with eufylline and platifylline are more suitable for patients with angiospasms. Headaches can be relieved with a calcium collar, and if head pain is combined with hyperexcitability and sleep disturbance, electrophoresis of bromine and iodine is used.
To optimize hemostasis, galvanization and drug electrophoresis with increasing the size of electrodes up to 300 cm² is indicated. 10% acetylsalicylic acid and 10% potassium orotate with 40% dimexide solution are used. The course of therapy includes about 10 sessions.
The practice of 3-4 sessions of electrophoresis of 0.1% dihydroergotamine with further application of 0.5% stuggerone according to method No. 2 with simultaneous internal administration of these drugs demonstrates a good effect in lesions of extracranial arteries. Calcium electrophoresis on the sinocarotid reflexogenic area, electrosleep procedures with a pulse frequency of 1-20 Hz are often prescribed.
The use of diadynamic current influences on the area of cervical sympathetic nodes is appropriate for patients with high or normal blood pressure, regional cerebral hypertension. The course of therapy includes five bilateral procedures (the first three days - daily, and two more times - every other day).
Therapeutic baths (radon, sodium chloride and carbon dioxide baths) are indicated for low blood pressure. Hydrogen sulphide treatments are more suitable for patients with hypertension.
In addition, patients with atherosclerosis of extracranial arteries are recommended regular and long walks in the fresh air, swimming, air baths, aerotherapy, electrosleep. Therapeutic showers (dust, jet, circulatory, fan), physical therapy, rubdowns, hiking are actively used.
In addition to medications can be used herbal treatment, which consists of oral intake of decoctions and aqueous infusions of medicinal plants such as meadow clover (only its flowers are used), alfalfa (the whole plant is used), flax (its seeds are used), chicory and dandelion (decoction is prepared from dried roots).
Many medicinal herbs have a fairly strong anticholesterol and restorative effect, but their use should not replace drug treatment, especially in the late stages of atherosclerosis of extracranial arteries, when the likelihood of forming complications is particularly high. It is possible to use the following medicinal plants:
- Ginkgo biloba - the leaves of this plant are successfully used in the form of aqueous and alcoholic solutions to cleanse blood vessels, strengthen their walls and improve elasticity. To prepare a tincture, take 50 g of leaves of the plant, pour 500 ml of vodka, insist in a dark place for two weeks. The resulting remedy is filtered and take 15 drops with 50 ml of water three times a day before meals. To brew the leaves with boiling water, take 1 tbsp. L. Raw materials in 250 ml of boiling water, insist for about 20 minutes, filter and drink one large sip between meals.
- Sophora japonica - used in the form of alcohol tincture, which is prepared as follows: 50 g of raw materials poured 500 ml of vodka, kept in a sealed container for 20 days. Then the drug is filtered and take 1 tsp. With 50 ml of water three times a day before meals. Duration of intake - 6 months.
- Common schlemnia - known for its ability to get rid of tinnitus, stabilize blood pressure, cleanse blood vessels. Alcohol tincture is taken 30 drops three times a day before meals, with 50 ml of water, for 5-6 months.
Other plants are known to improve the condition of blood vessels and eliminate negative atherosclerotic manifestations. In particular, we are talking about hawthorn fruit, red clover, blackcurrant rowan, horsetail, yarrow, topinambur, St. John's wort and succession, currant and strawberry leaves. A similar effect has a familiar to us parsley, nettle, chestnut blossom, melissa, motherwort. The above herbs can be used separately or in the form of herbal collections. If the patient is overweight, then to such a collection it is desirable to add the plant chicory and corn stigmas.
Surgical treatment in the form of endovascular stenting or balloon angioplasty of the affected artery is indicated in cases of severe stenotic atherosclerosis with the threat of vessel occlusion.
Surgical intervention for atherosclerosis of the extracranial arteries is of several types:
- Endovascular stenting (introduction into the affected artery of a special dilator - a stent, which pushes back atherosclerotic masses and widens the vascular lumen, normalizing blood flow).
- Open intervention with excision of the affected vascular segment followed by prosthesis.
- Carotid endarterectomy is another open intervention, during which the atherosclerotic focus is removed together with the intima-media complex from the carotid arteries with further suturing.
- Bypass - sewing a segment of the patient's own vein into the damaged artery, bypassing the occluded area (often the vein of the lower leg is used).
Surgical treatment options are indicated if the narrowing of the arterial vessel lumen is 75% or more, and if stroke or recurrent transient attacks develop.
The method of surgery is selected individually for each patient, taking into account his age, the stage of the pathological process, the presence of concomitant chronic diseases. The need for surgical intervention can be avoided if you start preventive measures to prevent the development of atherosclerosis of extracranial arteries in advance. [10]
What diet for atherosclerosis of the brachiocephalic arteries is necessary, read:
Prevention
In addition to general recommendations regarding smoking cessation, normalization of body weight and increased physical activity, measures to prevent atherosclerosis of any localization include proper nutrition.
Atherosclerosis of extracranial arteries develops gradually, over many years: this is the insidiousness of the pathology, which remains undetected for a long time.
Scientists report that the formation of atherosclerotic changes starts already in childhood. Lipid traces on the inner vascular wall are found in almost all children over the age of 10. As for the first symptoms of lesions of extracranial arteries, they occur much later:
- Men - mostly after the age of 40;
- Women - after 50 or more years of age.
Many experts point out that, in general, the first signs appear at a young age, it's just that most people do not pay proper attention to them. We are talking about such symptoms as:
- Rapid fatigue;
- Excessive nervous excitement;
- An unexplained drop in performance;
- Sleep disorders (often - nocturnal insomnia and daytime sleepiness);
- Dizziness, noise and pain in the head.
As atherosclerotic changes form, the walls of extracranial arteries thicken, blood circulation and blood supply to the brain deteriorate. This entails the start of metabolic disorders, increasing organ dysfunction.
Given the peculiarities of the development of atherosclerosis of extracranial arteries, its prolonged veiled course, you should not ignore the measures of early prevention of the disease. Such measures are simple and consist of a healthy lifestyle, proper nutrition, avoidance of stress.
Medical experts are sure that you can start fighting the disease at any age. For this purpose, the following principles should be observed:
- Change of lifestyle and some behavioral patterns. It is recommended to reduce the intake of saturated fats, cholesterol-containing foods, while increasing the intake of dietary fiber. In addition, it is important to control body weight, maintain physical activity and completely stop smoking.
- Timely treatment of diseases affecting the cardiovascular system. This item also includes supporting the functioning of organs such as the liver and kidneys (prevention of relevant diseases).
- Taking cholesterol-lowering drugs (prophylactic use of statins, fibrates, means based on nicotinic acid, bile acid sequestrants, policosanol, omega-polyunsaturated fatty acids, etc., as indicated).
All people after 40 years of age should carefully monitor the lipid spectrum and blood sugar, regularly visit a cardiologist and neurologist. Early diagnostic measures and fulfillment of all medical prescriptions can prevent and slow down the progression of atherosclerosis of extracranial arteries, as well as avoid dangerous consequences of the disease.
To date, scientists are intensively studying the possibility of creating an anti-atherosclerotic vaccine - a drug that suppresses the development and progression of atherosclerotic process. Specialists have already studied the effect of vaccination on rodents: it turned out to be greater than 68% (compared to unvaccinated rodents). The final result of the research is not yet available, the work on the vaccine is still in progress.
Forecast
Considering the consequences possible in atherosclerosis of extracranial branches of brachiocephalic arteries, the prognosis of this disease is in direct dependence on the stage of atherogenesis and risk factors for its development.
In case of unfavorable development of events, the disease is complicated by the development of stroke and dementia, resulting in disability or death.
To improve forecasts, it is recommended that:
- Follow the doctor's advice;
- Reconsider the basic principles of nutrition and lifestyle, eliminate bad habits;
- Maintain physical activity, take frequent walks, adjust the work and rest regime;
- Take all medications prescribed by your doctor carefully.
In many cases, provided timely treatment, the development of atherosclerotic changes can be slowed down. Patients who ignore medical recommendations, in most cases, in the future receive various complications: atherosclerosis of extracranial arteries ends, in particular, with stroke.

