Acute odontogenic osteomyelitis
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Acute inflammatory process of purulent-necrotic nature in the bone tissues of the jaws, which develops due to infection of the teeth or surrounding tissues (so-called odontogenic infection), is defined as acute odontogenic osteomyelitis. [1]
Epidemiology
The overall incidence of osteomyelitis in adults is approximately 90 cases per 100,000 people per year. Acute odontogenic osteomyelitis of the facial skeleton is currently detected rarely, but an estimate of its prevalence in adults is not available in the specialized literature. But acute odontogenic osteomyelitis in children, according to some data, is detected in one case per 5 thousand pediatric dental patients.
Causes of the acute odontogenic osteomyelitis.
Odontogenic osteomyelitis of the jaw is caused by the spread of a polymicrobial opportunistic infection (obligate oral microbiota), the primary cause of intraosseous inflammation.
Its causative agents are anaerobic gram-positive cocci of the Streptococcus milleri and Peptostreptococcus groups. Streptococcus mitis, Streptococcus sanguinis, Streptococcus salivarius and Streptococcus anginosus, gram-negative bacilli Bacteroides (Prevotella) and Fusobacterium nuckatum, which cause diseases of teeth and peri-dental structures - periodontium and periodontium.
In fact, such bone inflammation develops as a maxillofacial complication of untreated tooth decay (especially dental caries); infection of the root canal of a tooth with the development of pulpitis (inflammation of the tissue filling the cavity of the tooth); periodontitis chronic form; pericoronitis (developing during eruption of teeth, especially third molars - wisdom teeth); chronic periodontitis. Direct infection of the alveolus of the extracted tooth with the development of alveolitis, and then its complication in the form of inflammation of the bone tissue of the jaw is not excluded.
As a rule, the acute stage of odontogenic osteomyelitis lasts for two weeks after the onset of the disease. Although, as noted by experts, the division of osteomyelitis of any origin on the acute or chronic is based not on the duration of the disease, but on the data of histology. And acute is considered osteomyelitis, which does not reach the stage of separation of areas of osteonecrosis - sequestrations from the intact bone and the appearance of purulent fistulas. [2]
Risk factors
Risk factors for the development of acute odontogenic osteomyelitis are conditions with weakened immunity, including acquired immunodeficiency syndrome, chemotherapy and radiation therapy, as well as diabetes; peripheral vascular disease (with impaired regional or local perfusion); autoimmune diseases, a decrease in the level of leukocytes in the blood in the form of agranulocytosis.
There is an increased risk of purulent-necrotic inflammation of the bone tissues of the maxillofacial region in patients with syphilis, leukemia, sickle cell anemia, long-term use of corticosteroids, as well as in the elderly, smokers and alcohol abusers. [3]
Pathogenesis
The acute form of odontogenic osteomyelitis begins with the spread of bacteria from the initial focus to neighboring bone structures - the cortical layer and cancellous bone of the jaws.
The pathogenesis of the disease is due to the response to bacterial invasion of the cancellous bone substance (trabecular bone tissue), the onset of which is associated with the activation of the main mediator of bone tissue inflammation - the proinflammatory cytokine RANKL (ligand of nuclear factor kappa-B receptor-activator), which belongs to the TNF (tumor necrosis factor) superfamily. This transmembrane protein produced by macrophages, in turn, signals to multinucleated bone cells of myeloid origin - osteoclasts, which are considered a component of the mononuclear phagocyte system (part of the immune system). As a result of increased resorptive activity of osteoclasts (increased secretion of hydrogen ions, collagenase and cathepsin K enzymes, as well as hydrolytic enzymes), bone tissue destruction - pathological osteolysis (osteonecrosis) - occurs.
In addition, the inflammatory reaction leads to the formation of purulent exudate that accumulates in the intertrabecular spaces of the bone, which increases pressure and leads to venous stasis and ischemia. Pus may also spread to the subosteal layer, separating it from the bone surface and thereby exacerbating bone ischemia, leading to bone necrosis. [4]
Symptoms of the acute odontogenic osteomyelitis.
In the acute form of odontogenic osteomyelitis, the first signs are manifested by swelling, redness of the mucous membrane and increasing pain in the affected jaw.
Acute odontogenic osteomyelitis of the mandible (mandibular alveolar process) is the most common, while acute odontogenic osteomyelitis of the maxilla) is less common. Experts explain this by the fact that the upper jaw - due to its better blood supply, thinner cortical plates of the compact substance of the maxillary alveolar process and smaller medullary space in the bone tissue - is more resistant to infections.
Also local signs of acute odontogenic osteomyelitis of the jaw include swelling (external edema) on the affected side (arising due to internal inflammatory edema), hyperemia of the gingiva and mucosa of the transitional cheek fold, increased mobility of teeth in the infected area, thickening of the affected part of the alveolar process.
The clinical picture also includes fever and headache or facial pain, general malaise, limitation of jaw mobility with difficulty opening the mouth, the appearance of putrid breath (due to the accumulation of pus). If inflammation localized in the lower jaw causes alteration or compression of the inferior alveolar neurovascular bundle passing in its internal canal, sensory disturbance (numbness) in the zone of innervation of the chin nerve is observed.
A distinction is made between limited (focal) and diffuse types of odontogenic osteomyelitis of acute form. Limited inflammation is characterized by the lesion of a relatively small area of the jaw (down from the alveolar process), the appearance of an infiltrate on the gingival mucosa (painful when pressed), pain is aching, and body temperature does not exceed +37.5 ° C. In osteomyelitis diffuse (often occurring in children), the lesion is more extensive - with a significant size of the inflammatory infiltrate of the soft tissues of the gingiva and the transitional fold, the temperature rises to +39 ° C or more (with chills), severe pain of a pulsating nature, radiating to the eye socket, sinuses, ear lobe, temple or neck. Regional lymph node enlargement is common. [5]
Complications and consequences
Possible complications and consequences of this inflammatory process are manifested:
- With a subgingival abscess;
- With spilled purulent cellular melting-- peri-mandibular phlegmona:
- Odontogenic sinusitis (maxillary sinusitis);
- Chronicity and spread of infection to the deep cervical fascial regions;
- Phlebitis of the facial veins;
- Pathologic fracture of the mandible - due to a significant decrease in bone density.
The threat of meningitis, meningoencephalitis and general blood poisoning cannot be excluded.
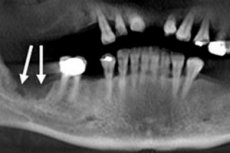
Diagnostics of the acute odontogenic osteomyelitis.
Diagnosis of osteomyelitis begins with a history and examination of the patients teeth and entire oral cavity.
General and biochemical blood tests are taken. A culture of the exudate may be performed to determine bacterial infection.
Instrumental diagnostics include:
Differential diagnosis
A differential diagnosis is necessary with purulent periostitis of the tooth; osteoradionecrosis (osteomyelitis affecting bone after radiation therapy); osteonecrosis of the jaws caused by osteoporosis treatment with bisphosphonates; maxillofacial cyst. [6]
Treatment of the acute odontogenic osteomyelitis.
Medication treatment of osteomyelitis of the jaws is carried out with such broad-spectrum antibiotics as Clindamycin, Metronidazole, Amoxicillin, Flucloxacillin, Lincomycin, as well as antibacterial drugs of the group of cephalosporins.
In addition, the underlying predisposing factors or conditions must be adequately addressed and treated. The causative tooth in acute odontogenic osteomyelitis either undergoes endodontic treatment (treatment of its canal) or extraction; surgical treatment also consists of sanitation of the affected area - removal of necrotic soft and bony tissues. [7]
Prevention
The basis of prevention of this disease is regular care of teeth and oral cavity, plaque removal, as well as timely treatment of dental diseases.
Forecast
With timely detection of the disease, its proper treatment and the absence of complications, the outcome of acute odontogenic osteomyelitis can be considered positive.

