Neurinoma of the brain and spinal cord
Last reviewed: 07.06.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A benign tumor process, neurinoma of the brain and spinal cord, originates from lemmocytes. These are so-called Schwann structures, auxiliary nerve cells formed along the course of the axons of peripheral nerves. Another name for the tumor is schwannoma. It is characterized by slow but steady growth, sometimes reaching quite large sizes (more than 1-2 kg). It can appear in patients of any age, significantly impairing the quality of life. [1]
Epidemiology
Neurinoma of the brain and spinal cord occurs in approximately 1.5% of all tumor processes. The incidence increases with age. The greatest number of patients with diagnosed neurinomas are between 45 and 65 years of age.
Men get the disease at about the same rate as women. For every ten neurinomas of the brain, there is one with spinal cord involvement.
Most primary neurinomas occur without a clear and distinct cause.
The percentage of ossification of such tumor processes is small, but is not completely excluded. The preferred method of treatment is surgical. [2]
Causes of the neurinomas of the brain and spinal cord
Scientists have not yet identified clear causes of neurinoma formation in the brain and spinal cord. A number of theories point to immune disorders and hereditary predisposition.
A large percentage of probability belongs to genetic predisposition: there are already many cases when neurinoma of the brain and spinal cord was literally "inherited". If one of the parents has an aggravated heredity or has a neurinoma, in 50% of cases the children will also have this disease.
The second possible cause is considered to be a weak immune system, which can be caused by almost any factor, such as:
- Unfavorable ecology, gassiness, intoxication;
- Stresses;
- Hypodynamia;
- Trauma and overload.
Eventually any of the causes mentioned can lead to the formation of a neurinoma. [3]
Risk factors
Major risk factors include:
- Ages over 35-45 years old and up to 65 years old.
- History of neurofibromatosis type 2 (for bilateral neurinomas).
- An unfavorable hereditary history.
Belonging to any of the risk groups is a signal that a person should be particularly attentive to his or her own health. It is important to visit doctors regularly and perform the necessary diagnostic measures to detect neurinoma of the brain and spinal cord at an early stage of development.
Pathogenesis
Each type of neurinoma has its own characteristics, including pathogenetic, etiologic, and clinical features. Let us consider the most common types of such neoplasms:
- Neurinoma of the spinal column (cervical, thoracic or lumbar) according to the generally accepted classification belongs to the extracerebral series, takes its development from the spinal roots and exerts pressure from the outside on the spinal cord. As the tumor focus grows, the clinical picture expands and worsens, the pain increases.
- A cerebral neurinoma is a neoplasm affecting the cranial nerves within the skull. The trigeminal and auditory nerves are predominantly affected. In the vast majority of cases, the lesion is unilateral. Neurinoma of the auditory nerve is characterized by rapidly increasing compression of the surrounding structures of the brain: the cochlear part of the nerve, the withdrawing and facial nerves may be affected.
To date, the pathogenetic mechanism of the development of neurinoma of the brain and spinal cord remains incompletely understood. The process is associated with pathological overgrowth of schwann cells, which is the reason for the second name of the disease - schwannoma. According to some reports, the pathology has to do with mutation of genes of chromosome 22. Such genes are responsible for encoding the synthesis of a protein that inhibits cell growth in the myelin sheath. Failure in the synthesis of this protein leads to excessive growth of schwann cells.
With neurinoma of the brain and spinal cord is associated with such pathology as neurofibromatosis, in which there is an increased propensity to develop benign neoplasms in various organs and structures. The disease is transmitted by autosomal dominant inheritance. [4]
Symptoms of the neurinomas of the brain and spinal cord
Neurinoma of the brain and spinal cord may not make itself known for a long time, only after some time, manifested by individual signs, to which it is important to pay attention in time:
- Pain by type of radicular syndrome, with partial paralysis, sensory disturbance;
- Disorder of the digestive system, pelvic organs (depending on the location of neurinoma), erectile dysfunction;
- Heart malfunctions;
- Decreased quality of life due to deterioration of motor function, difficulty in walking and performing normal daily tasks.
The first signs also depend on the localization of the disease process and may be as follows:
- Dizziness, headache;
- Pain in the back (neck, chest, lumbar or sacrum, with irradiation to the extremities, shoulders, shoulder blades);
- Numbness in the extremities, paresis and paralysis;
- Motor impairment;
- Tinnitus, visual impairment.
The initial clinical picture does not appear until some time - often several years - after the development of neurinoma of the brain and spinal cord. [5]
Spinal neurinoma is characterized by:
- Knee syndrome (pain along the spinal column, sometimes - flaccid paralysis and sensory disturbances in the area of innervation).
- Autonomic disorders (pelvic dysfunction, digestive disorders, cardiac disorders).
- Spinal cord compression syndrome (Broun-Sekar syndrome, manifested by spastic paresis, flaccid paralysis at the level of neurinoma, loss of sensation on the affected side, loss of temperature and pain sensitivity on the opposite side).
- Uncomfortable sensation in the interscapular region, pain, loss of sensation.
In cerebral neurinoma, symptoms such as these are predominant:
- Increased intracranial pressure;
- Mental, intellectual disabilities;
- Ataxia;
- Muscle twitches;
- Muscle tone disorders in the extremities;
- Cardiac and respiratory failure;
- Visual disturbance.
Auditory nerve neurinoma is noted:
- Ear noise, ringing on the affected side;
- Gradual deterioration of hearing function;
- Atrophy of the masticatory muscles, tooth-like pain;
- Salivary gland dysfunction, loss of taste perception, loss of sensation of half of the face, strabismus, double vision;
- Dizziness, vestibular disorders.
Spinal cord radicular neurinoma.
Nerve root tumor processes are mostly benign, they develop from nerve tissue or nerve sheath cells. Such neurinomas more often affect the thoracic spine, but can be found in other parts of the spine. Such foci slowly increase, more often have a small size, gradually fill the bony canal of the spinal cord root and begin to press on nearby structures. This entails the appearance of intense spinal pain, similar to an attack of sciatica. When the pathological process penetrates into the spinal canal, paresis develops, the function of digestive and pelvic organs is disturbed.
The complexity of the problem once again proves that back pain is an important signal that should not be ignored. It is necessary to contact specialists in time to find out the cause of the pain syndrome.
Complications and consequences
Neurinoma of the brain and spinal cord is a benign neoplasm that often causes unilateral paresis and paralysis, unilateral hearing impairment, temperature and pain sensitivity disorders, impaired mental functioning and balance.
In the absence of timely surgical intervention, neurinoma compresses nearby structures of the brain and spinal cord, which can provoke the development of life-threatening conditions. Even with slow tumor growth, disability and even death are possible. Malignization of a previously benign mass is not excluded.
The most common complications of neurinoma of the brain and spinal cord are:
- Loss of limb function (similar to post-stroke effects);
- Loss of vision or hearing (unilateral and bilateral);
- Headaches and spinal pain, up to and including the inability to perform daily activities;
- Personality and behavioral changes;
- Seizures caused by irritation of brain structures;
- Cerebral coma (final complication of tumor intracerebral processes).
Treatment and rehabilitation measures are necessary in any case, given that neuroma can affect the nerves that control vital functions of the body. Proper recovery based on timely treatment helps the patient to return to his or her usual way of life. [6]
Diagnostics of the neurinomas of the brain and spinal cord
Which diagnostic tests are suitable for detecting neurinoma of the brain and spinal cord is decided by a neurosurgeon or neurologist individually for each specific case. In general, diagnosis begins with the exclusion of pathologies that are similar in clinical manifestations. It is obligatory to perform physical examination, listen to the patient's complaints.
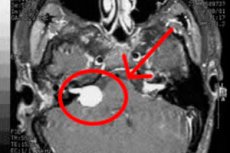
Instrumental diagnosis is usually represented by the following measures:
- In case of intracranial neurinoma, the patient is referred to MRI or CT scan of the brain. Computed tomography in this situation is much less informative - primarily because it does not visualize small neoplasms with sizes less than 20 mm. If the patient cannot undergo MRI, a contrast-enhanced CT scan may be administered as an alternative.
- An MRI or CT scan of the spinal column can help identify neurinoma or other neoplasms pressing on spinal structures and nerve endings.
- Audiometry is appropriate as part of complex diagnostic measures to detect auditory neuroma. The procedure provides information about the degree of loss of auditory function and the causes of the pathology.
- Ultrasound or MRI is considered informative when the tumor process is localized in the area of peripheral nerves. Ultrasound visualizes the thickening of the protective neurilemma, while MRI helps to determine the exact location of the nidus, its structure and the extent of nerve damage.
- Electroneuromyography evaluates the transport of electrical impulses along the nerve fiber, which makes it possible to assess the degree of disturbance in the nerve structure.
- Biopsy with further cytologic analysis is associated with surgical intervention and allows to determine the malignancy or benignity of neurinoma.
Tests are prescribed as part of the patient's preparation for hospitalization and surgery. The patient takes blood for general and biochemical analysis, as well as a general urinalysis. If indicated, it is possible to prescribe other types of laboratory tests at the discretion of the doctor. [7]
Differential diagnosis
Differential diagnosis of neurinoma of the brain and spinal cord should be carried out with other tumor processes (including metastatic), as well as with abscesses, lymphoma of the central nervous system, inflammatory and demyelinating pathologies.
Magnetic resonance imaging with contrast enhancement is mandatory. If indicated, other diagnostic methods are also used:
- Electroencephalography;
- Radiographs;
- Ultrasound examination of the pelvic and abdominal organs, as well as peripheral lymph nodes;
- Skeletal bone scintigraphy.
If a primary pathologic focus is detected, a complete diagnosis is carried out.
Treatment of the neurinomas of the brain and spinal cord
Three treatment tactics are commonly used for neurinoma of the brain and spinal cord: observation of the neoplasm, surgery, and radiation therapy. The choice of treatment direction is left to the attending physician.
Observation-waiting tactics are used when neurinoma is accidentally detected against the background of complete absence of any clinical manifestations and signs of tumor progression. Such a "quiet" state can last for several years. However, during this time it is important to regularly observe the dynamics of neoplasm growth, and in case of deterioration of the situation, to react urgently by performing surgery.
Radiation therapy involves local irradiation of the pathologic focus in case it is not possible to perform a full surgical intervention. This method helps to "put to sleep" the neoplasm, but is accompanied by many side effects - digestive disorders, skin reactions, etc.
Surgical removal of neurinoma of the brain and spinal cord is a complex but radical method that allows further complete elimination of the disease, with minimal risk of recurrence. Surgery is always preferable to other methods of treatment of neurinoma. [8]
Medications
Drug therapy may include the use of the following medications:
- Manitol (Mannitol) is an osmotic diuretic that eliminates brain edema and normalizes intracranial pressure. It is administered intravenously by drip, using a 20% solution, over 10-15 minutes. It can be combined with glucocorticosteroids. During treatment, control of diuresis and water-electrolyte equilibrium is mandatory. The drug is prescribed for a short course, because with prolonged use it itself can lead to secondary hypertension.
- Glucocorticosteroids orally or parenterally (Dexamethasone, Prednisolone) in an individually prescribed dosage. After surgery, the dose is reviewed and gradually reduced.
- Medications that improve cerebral blood circulation (Kavinton - taken orally, after meals, 5-10 mg three times a day, or Nicergoline - 5-10 mg three times a day between meals).
Strong sedatives and neuroleptics, as a rule, do not prescribe, because they in many cases "hide" the deterioration of the patient's condition.
Surgical treatment
Surgical intervention - removal of the neoplasm - is the most common type of treatment for patients with neurinoma of the brain and spinal cord. The choice of surgical access and the extent of surgery is determined by the size of the pathologic focus, the possibility of preserving and restoring brain functions.
The intervention is performed by a neurosurgeon and general anesthesia is used. The main difficulties of surgery in the brain region are the separation of the neoplasm from the nerves and brain stem. Neurinoma of large sizes often "fattens" other nerve fibers, so the removal of these fibers requires a highly skilled approach and simultaneous neurophysiological monitoring, allowing timely detection of one or another nerve.
Complete removal of the neurinoma is possible in 95% of cases. In the remaining 5% of patients, difficulties may arise, for example, if part of the tumor is "fused" with other nerve structures or the brain stem.
Chemotherapy is usually not used after surgery. When the neurinoma is completely removed, radiation therapy and radiosurgery are also not justified. The probability of recurrence is estimated to be about 5%.
The Gamma Knife radiosurgical method involves focal radiation exposure to the pathologic focus. The procedure is used for neurinomas of small size (up to 3 cm) and in the absence of pressure on the brainstem. The main direction of radiosurgery is not in the removal, but in the prevention of subsequent tumor progression. Sometimes it is possible to slightly reduce the size of the mass in this way.
Gamma knife, Cyberknife and linear gas pedal methods involve the use of the principle of introducing a certain amount of ionizing radiation into the neoplasm, which entails destruction of the focus without damaging biological tissues. Not all of these methods are non-invasive. Thus, the use of Gamma Knife requires rigid fixation of the metal frame with screw devices to the cranial bones. In addition, the use of Gamma Knife is not always effective, because sometimes it is not possible to form a uniform dose of radiation, which leads to either incomplete removal of the focus, or to the delivery of high doses to normal areas of the brain. For these reasons, radiation therapy and Cyberknife radiosurgery are more commonly used in treatment practice. [9]
Prevention
Preventive measures are nonspecific, since the exact causes of neurinoma of the brain and spinal cord have not been determined to date. Doctors suggest paying attention to general recommendations:
- Providing the normal healthy sleep and rest needed to regularly restore the functional state of the brain;
- Avoiding alcohol, drugs, smoking, and junk food;
- Development of stress resistance, avoidance of conflicts, stress, and worries;
- Consumption of a sufficient amount of plant food, observance of an adequate water regime;
- Avoiding back and head injuries;
- An active lifestyle, regular walks in the fresh air;
- Absence of physical and mental overload;
- Regular visits to the doctor in the presence of risk factors, in case of suspicious symptoms, as well as for routine preventive diagnostics.
Forecast
The overall prognosis for neurinoma of the brain and spinal cord is considered positive, under the conditions of timely referral to doctors and fulfillment of all medical recommendations. Since the neoplasm develops slowly over a period of time, a prolonged wait-and-see tactic can be employed. However, if the pathological focus is located in a convenient place for surgery, experts recommend removing it if possible, which is usually not accompanied by the appearance of any adverse effects on the body. [10]
If treatment is ignored or if the tumor process is diagnosed late, sensory disturbances, paresis and paralysis, as well as other dangerous conditions may occur. Therefore, it is important to understand that neurinoma of the brain and spinal cord is a rather complex tumor, although benign, and it must be radically and timely treated. Otherwise, the appearance of serious problems with health and quality of life is not excluded, there is also a possibility of malignization of neurinoma.

