Dissecting osteochondritis
Last reviewed: 12.03.2022

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Among the many different diseases of the musculoskeletal system, osteochondritis dissecans is relatively rare, a disease that is a limited form of aseptic necrosis of the subchondral bone plate. Pathology is characterized by the separation of a small cartilage element from the bone and its displacement into the articular cavity.
Osteochondritis dissecans was first described in the 19th century by Dr. Paget, a British surgeon and pathologist. Then the disease was called "hidden necrosis." The pathology acquired the current name of osteochondritis dissecans a little later - at the end of the same 19th century: this term was introduced by the German surgeon Franz Koenig.
The disease most often affects the knee joint, but can develop in other joints, regardless of their size. [1]
Epidemiology
Dissecting osteochondritis occurs in only 1% of cases of joint diseases. Pathology is most often diagnosed in young men (mainly in athletes), but it can also occur in children. The ratio of sick men and women is 2:1. Approximately every fourth patient has a bilateral disease.
Osteochondritis dissecans in 85% of cases affects the internal condyle of the femur - Koenig's disease develops. In 10% of cases, the external condyle suffers, in 5% of the patella (Leven's disease develops). [2]
The overall incidence of pathology is 15-30 cases per hundred thousand of the population. [3]The average age range of patients is 10-20 years. [4]
In childhood, the pathology proceeds more favorably: recovery occurs as a result of drug therapy. Adult patients often require surgery.
Causes of the dissecting osteochondritis
The most common cause of osteochondritis dissecans is trauma, injury, or excessive pressure. With these effects, there is a deterioration in the blood supply to the tissues inside the joint (ischemia). Such processes, in turn, cause gradual necrosis of the bone fragment, which eventually separates.
The exact causes of the disease are unknown. Experts believe that pathology is the result of the influence of several factors at once. So, the most likely cause is trauma, direct or indirect damage to the joint. Additional factors may be:
- hereditary predisposition;
- genetic diseases;
- individual features of anatomy;
- metabolic disorders;
- improper maturation of the skeletal system.
Already existing dissecting osteochondritis can be aggravated by further joint loads. In particular, people who are actively involved in sports such as basketball or football, tennis, weightlifting, biathlon, shot put, gymnastics or wrestling are most affected by the pathology. The risk group also includes persons whose professional activities are associated with the constant performance of the same type of repetitive movements that have an excessive effect on the articular function. [5]
Risk factors
The origin of osteochondritis dissecans is currently not well understood. Among the factors contributing to the emergence and development of the disease, we can distinguish the following:
- local necrotic processes in the subchondral bone plate;
- repetitive joint injuries, including exogenous (bruised injuries) and endogenous (impeachment syndrome that develops with internal rotation of the joint, as well as habitual dislocations, chronic articular instability, chronic injuries);
- disturbed endochondral ossification;
- endocrine diseases;
- genetic predisposition (anatomical defects of the articular structure, congenital anomalies of the subchondral layer, etc.);
- insufficient blood circulation, impaired trophic bone and cartilage tissue, ischemic disorders;
- excessive regular load on the joint.
Many authors suggest familial inheritance, even describing it as a mild form of skeletal dysplasia with concomitant short stature. [6]However, [7] challenging the evidence for familial inheritance, Petrie [8] reported radiographic examination of first-degree relatives and found only 1.2% with acute osteochondritis dissecans.
Pathogenesis
The pathogenetic mechanism for the development of osteochondritis dissecans has not been sufficiently studied to date. There are several theories that are considered by experts as the main ones. However, none of them has been officially confirmed yet. However, let's look at them one by one:
- Inflammatory process.
Some researchers have described inflammatory changes in the histological material of patients with osteochondritis dissecans. A detailed microscopic analysis revealed necrotic, nonspecific, aseptic signs of inflammation, however, in some biomaterials, such changes were still absent. [9]
- Acute traumatic injury.
There have been described cases of osteochondritis dissecans as a consequence of chronic or acute trauma that caused ischemic processes with the formation of free bone and cartilage elements.
- Re-injury.
Repeated microdamages can become a provoking factor of the disease, which is especially typical for children. [10], [11]
- genetic predisposition.
There is evidence of the existence of a hereditary predisposition to the development of articular pathologies. In particular, some patients have anatomical features that contribute to the appearance of this problem. [12]
- ischemic processes.
The theory of involvement of ischemia or deterioration of vascular trophism in the affected area has existed for a long time. Many cases indicated a deficiency of the vascular network, weak arterial branching in the area of pathology. [13], [14]
Currently, osteochondritis dissecans is considered as an acquired lesion of the subchondral bone, characterized by varying degrees of resorption and sequestration of bone tissue with possible involvement of the articular cartilage through detachment, not associated with an acute osteochondral fracture of normal cartilage. [15]
Symptoms of the dissecting osteochondritis
Clinical symptoms in osteochondritis dissecans are nonspecific and may differ from patient to patient. Patients of childhood and adolescence often complain of diffuse pain in the affected joint: intermittent, sometimes intermittent, acute, accompanied by blocking of movement in the joint and its swelling.
With the instability of the separated element, instability, blocking and crunching are noted. On examination, attention is drawn to the limitation of the load on the affected joint. Palpation is accompanied by pain. A long-term disease can be manifested by atrophic changes in the leading muscles.
The first signs of osteochondritis dissecans in adults and children are practically the same: usually it is a slight aching soreness or discomfort, which is aggravated by motor activity and joint load. As the pathology progresses, the pain syndrome increases, the joint becomes swollen, and palpation pains appear.
After detachment of the necrotic fragment, there are complaints of regular crunching and the appearance of motor "jamming", which is explained by the appearance of interference during the movement of the joint surfaces. There may be blockages - the so-called articular "jamming", which is manifested by acute pain and the inability to carry out the intended movement.
Pathology can grow and worsen over several years - 2, 3, and sometimes ten or more. The main symptoms may be:
- pain (aching or sharp); 80% of patients typically experience mild pain for an average of 14 months and mild to mild lameness after physical activity [16]
- edema;
- motor crunching;
- limitation of motor ability;
- articular blockage;
- increasing lameness (with damage to the joints of the lower extremities);
- muscle atrophic processes.
Osteochondritis dissecans in children
The causes of osteochondritis dissecans in childhood are also not clear. However, the prognosis in young children is more optimistic than in adults.
The disease is more often recorded in boys 10-15 years old, but the disease can also affect 5-9-year-old babies. In most cases, as they grow older, the disturbance smoothes out.
The main symptoms of a problem in a child:
- causeless pain (usually in the knee), aggravated by motor load;
- swelling and blockage of the joint.
These signs require urgent diagnosis - in particular, radiography, MRI, CT.
The favorable course of osteochondritis dissecans is not a reason not to treat. To begin with, the doctor advises the patient to completely exclude physical activity on the affected limb. If the disease affects the lower limbs, the child is prescribed crutches, with which he walks for several months (usually up to six months). Additionally, physiotherapy and exercise therapy are connected.
If no improvement has occurred within the specified time, then only in this case is surgical intervention prescribed:
- arthroscopic mosaic chondroplasty;
- revascularizing osteoperforation.
Stages
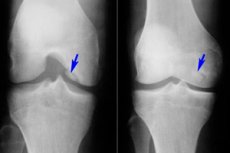
According to the information obtained in the course of X-ray studies, the following stages of the pathological process in osteochondritis dissecans are determined:
- Formation of a necrotic focus.
- Irreversible phase of the restriction of the necrotic area, dissection.
- Incomplete separation of a necrotic-limited element.
- Complete separation of the osteochondral element.
In addition to the above classification, stages are distinguished, depending on the endoscopic picture of osteochondritis dissecans:
- Intactness of hyaline cartilage, palpation reveals softness and swelling.
- The cartilage is separated and torn along the periphery of the necrotic focus.
- The necrotic-altered element is partially separated.
- A niche-shaped crater is formed in the affected area, there are free intra-articular elements.
Koenig's disease is divided into the following stages:
- The cartilage softens, while its integrity is not violated.
- Part of the cartilage is separated, stability is noted.
- The cartilage becomes necrotic and the continuity is broken.
- A free element is formed, localized in the formed defect, or behind it.
Forms
The pathology of osteochondritis dissecans is divided into adult and juvenile (developing in children and adolescents).
Classification, depending on the localization of the pathological process:
- Dissecting osteochondritis of the knee is a limited subchondral aseptic necrosis of the articular bone surface. The prevalence of the disease is 18-30 cases per hundred thousand patients. The predominantly loaded cartilaginous area is affected, which becomes the lateral segment of the medial condyle of the femur, near the intercondylar notch (internal or external condyle, patella). Dissecting osteochondritis of the patella has the most unfavorable prognosis, since it is difficult to treat. Dissecting osteochondritis of the medial condyle of the femur is also called Koenig's disease. [17], [18]
- Dissecting osteochondritis of the talus occurs in children aged 9-16 years and is an osteochondropathy of the talus, with aseptic necrosis and damage to the articular cartilage. Other names for the pathology are Diaz's disease, or osteochondritis dissecans of the ankle joint. The etiology of the disease is unknown. In the absence of treatment, gross defects of the articular cartilage are formed. [19]
- Dissecting osteochondritis of the shoulder joint is a lesion of the head of the condyle of the humerus in the central or anterior-outer sections. The disease is rare, found mainly in adolescents; otherwise it is called Panner's disease. Even less often, cases of damage to the head of the radius, olecranon and fossa are found. [20]
- Dissecting osteochondritis of the hip joint affects the head of the femur. The disease may have minimal clinical and radiographic manifestations for a long time, but over time, changes in the configuration of the articular surfaces become pronounced, movements in the joint become painful or blocked. Most often, pathology begins its development in childhood.
Complications and consequences
The most unfavorable complication of osteochondritis dissecans is the development of deforming arthrosis with motor blocking of the joint and violation of the axis of the affected limb.
The altered mechanical and biological component, due to aseptic necrosis of the bone plate and the appearance of free intra-articular elements, leads to the formation of deforming arthrosis with damage to hyaline cartilage. This complication is typical for dissecting osteochondritis of the knee joint, femur and tibia. The first signs of aggravation of the pathological process: increased pain, lameness (especially when walking down the stairs). There are articular blockages, a feeling of a foreign body inside the joint.
The progression of the pathology leads to the following consequences:
- the development of contracture and the appearance of crepitus;
- curvature of the articular contours due to disorders in the bone tissue and loss of cartilage, as well as muscle hypotrophy;
- narrowing of the joint space;
- the appearance of bone growths along the edges of the gap.
In the later stages of the disease, the patient loses the ability to fully straighten the limb in the affected joint, as a result, the limb (especially the lower one) is deformed. Radiographically, deformation and sclerosis of the articular surfaces, subchondral necrosis, significant narrowing of the joint space, extensive bone growths, and free intraarticular fragments are noted.
Diagnostics of the dissecting osteochondritis
Diagnostic measures begin with a survey and examination of the patient. Dissecting osteochondritis is characterized by complaints of pain, blockage in the joint, crunches and clicks, and limited motor volume. The patient may indicate previously transferred metabolic-dystrophic pathologies, injuries, intra-articular administration of medications.
During the examination, the doctor notes:
- articular blockage or severe motor limitation;
- clicking, crepitus.
Palpation is determined by joint pain and deformities.
Laboratory tests are prescribed as part of a general and differential examination of the body:
- general clinical blood test with the determination of the leukocyte formula;
- determination of ESR;
- fibrinogen;
- antistreptolysin O;
- serum uric acid level;
- C-reactive protein (quantitative method);
- rheumatoid factor;
- antinuclear factor on HEp-2 cells;
- the level of antibodies to the extracted nuclear antigen.
Laboratory diagnostics is necessary to exclude arthritis, systemic autoimmune diseases, rheumatoid arthritis, Sjögren's syndrome, etc.
Instrumental diagnostics is represented, first of all, by magnetic resonance imaging. It has been experimentally proven that MRI is the most preferred method for diagnosing osteochondritis dissecans, as it allows assessing the size of the focus and the condition of the cartilage and subchondral plate, determining the extent of bone marrow edema (signal intensity increases), detecting a free element in the joint, and tracing the dynamics of the pathological process. In addition, MRI helps to examine the condition of other articular structures: menisci, ligaments, synovial folds, etc. [21]
Ultrasound diagnostics and other research methods do not provide complete information about the disease. Plain radiography and computed tomography are uninformative in the initial stages of osteochondritis dissecans (2-4 weeks). These methods can only be used to clarify some points after an MRI.
Differential diagnosis
|
Pathology |
Main differences from osteochondritis dissecans |
|
Deforming osteoarthritis |
Osteophytes and ossified areas of ligaments often look like intra-articular free elements. However, they are usually irregular in shape and have sharp edges. There is also no condyle defect. |
|
Chondromatosis |
There is no characteristic crater in the epiphysis of the tibia or femur. Chondromic bodies are bean-shaped, their number reaches or even exceeds 10. |
|
Lipoarthritis (Goff's disease) |
There is a structural change in the infapatellar or suprapatellar lipid body that thickens and may cause pinching signs. X-ray and magnetic resonance methods allow for differential diagnosis. |
|
Fracture inside the joint |
The intra-articular separated element of traumatic origin has an irregular shape, uneven outlines. There is no characteristic crater. |
|
Erroneous interpretation without articular pathology |
In some cases, inexperienced specialists take the sesamoid bone of the tendon of the gastrocnemius muscles for an intra-articular detached fragment. For a characteristic crater of the lateral condyle of the femur, subcartilaginous enlightenment is sometimes taken - one of the variants of the normal anatomical structure of the joint. |
Treatment of the dissecting osteochondritis
Treatment is aimed at improving the trophism of bone and cartilage elements and fixing the separated parts. With the help of arthroscopy, the localization and extent of damage are visualized, the degree of detachment is determined. If initially the effectiveness of conservative treatment is questioned, surgical intervention is prescribed.
Dissecting osteochondritis, which is accompanied by characteristic symptoms, but does not have a clear detachment of the osteochondral element, is treated using the osteochondroperforative method, using Kirschner wires.
Conservative treatment is applicable only in the initial stages of the development of osteochondritis dissecans. Physiotherapeutic treatment is practiced against the background of unloading the affected joint for up to one and a half years. During this time, the patient is completely forbidden to play sports. For walking, the patient uses crutches, with the exception of the load on the affected limb. After the pain subsides, physiotherapy exercises are prescribed, which involve non-strength exercises, to prevent muscle atrophy. [22]
Medications
If an intra-articular inflammatory process is detected, antibiotic therapy is prescribed. The most likely use is Cefazolien or Gentamicin. Vancomycin is suitable for detecting Methicillin-resistant Staphylococcus aureus.
Non-steroidal anti-inflammatory drugs are used for pain relief. If the patient has contraindications to taking such drugs (ulcer, gastric bleeding), then Paracetamol becomes the drug of choice. For severe pain, opioid analgesics may be indicated.
|
Antibiotics |
|
|
Cefazolin |
The average daily dosage is 1-4 g, in the form of intravenous or intramuscular injections. The drug is not used for hypersensitivity to cephalosporin and beta-lactam antibiotics. |
|
Gentamicin |
The standard daily dosage of the drug is 3 mg / kg body weight intramuscularly or intravenously in 2-3 injections. The duration of therapy is 7 days. The drug has ototoxicity. |
|
Vancomycin |
It is prescribed individually, taking into account therapeutic indications. Enter intravenously drip. Rapid administration can provoke a number of side effects, including anaphylactic shock, shortness of breath, heart failure. |
|
Opioid painkillers |
|
|
Tramadol |
A single dose of the drug (intravenous or oral) is 50-100 mg. The maximum possible daily amount of the drug is 400 mg. The term of treatment is 1-3 days. |
|
Trimeperidine |
It is administered intramuscularly, intravenously in the form of a 1% solution, in an amount of 1 ml per day. Duration of application - 1-3 days. |
|
Non-steroidal anti-inflammatory drugs |
|
|
Ketoprofen |
It is taken orally at 200-300 mg per day for 2-3 doses, or injected intramuscularly at 100 mg 1-2 times a day. Possible side effects: dyspepsia, gastritis, skin rashes. |
|
Ketorolac |
A single dose of the drug is 10 mg. The maximum daily dosage is 40 mg. The duration of the course cannot exceed 5 days. It is also possible intramuscular or intravenous administration in minimally effective doses. Possible side effects: abdominal pain, diarrhea, stomatitis, cholestasis, headache. |
|
Paracetamol |
Assign 0.5-1 g up to 4 times a day, for 3-5 days. The drug is well tolerated and rarely causes side effects. Exception: allergic to paracetamol. |
Physiotherapy treatment
Physiotherapy is more often used at the stage of rehabilitation after surgery for osteochondritis dissecans. Preference is given to the following procedures:
- local effect of cryotherapy (course treatment includes up to 10 procedures);
- UV therapy (course duration - 10 days, one procedure daily);
- magnetotherapy (course treatment includes five to ten sessions);
- UHF-therapy (7-10 sessions);
- laser therapy (for 1 week daily).
To improve blood circulation in the affected joint and to prevent muscle atrophy, special exercise therapy exercises are prescribed:
- Muscle tension with a gradual increase in intensity, lasting 6 seconds, with a number of repetitions of about 10 per set.
- Repetitive flexion and extension of the fingers of the limb, exercises for training peripheral circulation (lowering and lifting the limbs).
- Exercises for the prevention of joint stiffness (up to 14 movements per approach).
It is possible to use mud therapy, hydrotherapy, at the discretion of the attending physician.
Herbal treatment
Dissecting osteochondritis in adults is a dynamically unfavorable pathology, which, if not properly treated, can lead to disability. Therefore, the sooner measures are taken to combat the disease, the better.
Treatment for osteochondritis dissecans should be carried out in a complex manner. If the attending physician does not object, some alternative methods can also be connected - in particular, herbal medicine.
- Rub the horseradish root on a grater, heat it a little to a warm state, put it on a cloth and put it in the form of a compress on the affected area. The procedure is repeated every other day.
- A vegetable collection is prepared from 1 tsp. Birch leaves, the same amount of nettle and dandelion leaves, marigold flowers and willow rhizomes. The mixture is poured into 1 liter of boiling water, insisted under the lid for 10 hours. Drink the remedy for half a glass three times a day for half an hour before meals. The term of treatment is 8 weeks.
- A collection is prepared on the basis of an equal amount of wild rosemary grass, hop cones, chamomile flowers and St. John's wort. Next, take 2 tbsp. L. Collection, pour 1 liter of boiling water, insist under the lid for about 10 hours, take half a glass 4 times a day before meals.
- Prepare a collection of 1 tsp. Raspberry stalks, the same amount of elecampane and nettle leaves, 1 tbsp. L. Wild rosemary and 1 tsp. Elderberry colors. 0.5 l of boiling water is added to the mixture, kept under the lid for 15-20 minutes. Filter and take 100 ml three times a day before meals. Duration of admission - up to three months.
- Pour 500 ml of boiling water 2 tbsp. L. Lingonberry leaves, insist for 40 minutes. Take 100-150 ml three times a day before meals.
Rubbing the affected joint with elecampane tincture gives a good effect (50 g of rhizome is poured into 150 ml of vodka and kept in a dark place for 2 weeks).
Surgery
Some authors believe that conservative treatment should be the first line of treatment for stable lesions in children [23]. [24]The only consensus regarding this method is that if this treatment is chosen, then its duration should be 3 to 6 months before the choice of surgical treatment. [25]
Surgery is usually indicated for unstable and stable foci of acute osteochondritis dissecans that are not amenable to conservative treatment. [26], [27]
Differences in surgeon preference for surgical treatment are reflected in the variety of surgical techniques. These include drilling (both retrograde and antegrade) [28], [29] bone grafting [30], [31] fixation, [32]alignment [33] procedures, [34] and debridementation. [35]
Osteochondritis dissecans, diagnosed in an adult patient, often becomes an indication for surgical intervention. At the initial stage of pathology development, the dead area is replaced by a newly formed tissue, and at subsequent stages, free fragments are removed by arthrotomy.
The scale of the intervention is determined after performing magnetic resonance imaging and arthroscopy. As a rule, while maintaining the contact of the free element with the surrounding tissue, the detached bone and cartilage fragment is reamed and replaced with living tissue. For tunneling, a Kirschner needle or a thin awl is used. The needle is placed in the center of the necrotic zone, perpendicular to the surface of the joint. The intervention is completed by resection of the cartilaginous area and processing of its edges.
If the OCD lesion is fragmented or not fixable as a result of cartilage quality or mismatch, then the fragment should be removed, the donor site removed, and the defect repaired based on individual findings. [36] Excision of the fragment may relieve short-term pain. [37], [38]
If the free element has a pronounced mobility, then it is first fixed with a clamp. Then the connecting junction (bone or cartilage) is cut, after which the element is removed. Channels are drilled in the subchondral plate, the edges are processed. The joint is washed, sutures and an aseptic bandage are applied.
After refixation of the free element, the wires are removed after about 2-2.5 months. In the postoperative period, the patient is prescribed antibiotic therapy and symptomatic drugs.
A new, modern arthroplasty technique is autogenous chondrocyte transplantation. The method involves the cultivation and transplantation of cells, however, due to the high cost of the procedure, its practice is currently limited. [39], [40]
Most authors report that the time to radiographic healing ranges from 6 weeks to 2 years.
Prevention
Since the etiology of osteochondritis dissecans has not been fully elucidated, there is no specific prevention of the disease yet. However, doctors still give a number of recommendations to prevent the development of such diseases. Such recommendations are primary and secondary.
Primary prevention consists in the general maintenance of the health of the musculoskeletal system:
- fight against excess weight;
- regular moderate physical activity;
- injury prevention, wearing comfortable and high-quality shoes;
- practice of general strengthening measures;
- exclusion of hypothermia, timely treatment of any pathologies in the body.
Secondary prevention involves preventing the aggravation of an existing osteochondritis dissecans. The main preventive measures are:
- limitation of the joint load;
- refusal of sports such as running, athletics, weightlifting, gymnastics, basketball, volleyball, football;
- correction of professional features, avoidance of prolonged standing, frequent squatting, regular walking up the stairs;
- revision of the diet, avoidance of starvation, refusal of fatty and monotonous food, ensuring the intake of essential microelements and vitamins in the body.
Physiotherapy exercises are carried out only under the supervision of a doctor. Proper exercises should not burden the musculoskeletal system, but restore the strength and elasticity of the joints, accelerate blood circulation and improve metabolic processes.
On the recommendation of a doctor, you can practice massage sessions for different muscle groups.
Forecast
Osteochondritis dissecans is a complex orthopedic problem, because it is not easy to both identify and treat, even despite the emergence of new developments in this direction.
The prognosis of the disease may depend on the type of treatment used (medical, surgical), on the maturity of the growth zones, on the location, stability and size of the detached element, on the integrity of the cartilage. In childhood, the outcome of the disease is mostly favorable: osteochondritis dissecans responds well to treatment in children. In adulthood, early diagnosis of pathology is important, which directly affects the long-term prognosis. The most unfavorable outcome is observed in patients with complications, as well as with pathology of the lateral condyle of the femur.

