Testicular hematocele
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hematocele is the medical term for an abnormal accumulation of blood in body cavities. Most often, this pathology occurs in the male genital area - in particular, in the scrotum and the vaginal membrane of the testicles. Therefore, when mentioning this pathology, most experts mean exactly testicular hematocele.
The vaginal membrane is a kind of protective barrier that surrounds the testes (each testicle separately). This membrane should not be confused with the scrotum, which is a musculocutaneous bursa.
Hematocele usually results from hemorrhage from damaged blood vessels. This happens with traumatic injuries, surgical procedures. In some patients, the appearance of pathology is associated with the development of testicular cancer, when the tumor grows and violates the integrity of the scrotal vascular network. [1]
Treatment options range from conservative therapy to surgery. [2]
Epidemiology
Hematocele due to trauma and other damage to the organs of the scrotum accounts for less than 1% of all similar cases involving other organs. The low prevalence of such a pathology is due to the anatomical localization of the scrotum, the strength of the vessels and the protein membrane, as well as the protective function of the cremaster muscle, which reacts quickly at a time when there is a danger of injury.
And, despite this, an extensive hematocele poses a rather large threat to health, since aggravating pathological processes can lead to testicular loss, which will adversely affect fertility, can provoke the development of hypogonadism and negatively affect psychosocial terms. In addition, the production of antisperm antibodies can cause the formation of immunogenic infertility, adversely affecting the quality of semen.
Most often, hematocele is found in patients aged 16-40 years. According to statistical information, traumatic injuries of the scrotum are in the first place among all injuries of the urogenital tract in men. [3]
Hematocele often has a one-sided character (in almost 99% of cases), and the right testicle suffers more often than the left one: experts attribute this to the peculiarities of the location of the right testicle relative to the pubis and the inner femoral surface.
According to the research results, among the causes of the appearance of hematocele, sports and industrial and domestic injuries are in the lead (in about 74% of cases), of which about 13% of cases are caused by road traffic accidents. The most rare causes are animal bites.
Drug treatment is used at the first or second stage of pathology. An indication for surgical intervention can be considered a hematocele, the size of which exceeds the volume of an intact testicle by more than three times, as well as a tense form of hematocele, which provokes severe pain syndrome.
Causes of the hematocele
The most common cause of the development of hematocele is considered to be a closed or blunt trauma to the genitals - in particular, to the scrotum. Injury can be the result of a direct impact, bruising as a result of an unsuccessful landing, domestic or industrial damage, an accident, etc.
Less often, pathology is provoked by various medical manipulations and procedures:
- unsuccessful puncture with a puncture of a venous or arterial vessel;
- damage to the vascular wall during the treatment of hydrocele - dropsy of the testicle, which leads to the appearance of blood elements in the exudative fluid;
- complications during a testicular biopsy (for example, with chronic orchitis, etc.).
In extremely rare (almost isolated) cases, hematocele becomes the result of such a systemic pathology as hemorrhagic diathesis - we are talking about a specific blood disease with a tendency to excessive bleeding. In some patients, it is not possible to establish the cause of the hematocele at all. [4]
Risk factors
Many factors affect our health, and those that lead to the development of diseases and the appearance of injuries are called risk factors: they often coexist and interact with each other, leading to a particular problem. For example, engaging in certain sports increases the risk of developing hematocele. These sports include:
- cycling, motorcycling;
- horseback riding;
- hockey, football;
- wrestling, kickboxing and other martial arts;
- rugby;
- golf;
- gymnastics.
It is these sports that are most often associated with the occurrence of blunt trauma to the genital organs. To prevent damage, remember to use special protective equipment.
Other factors may include:
- surgical, urological manipulations in the scrotum;
- animal bites (there is also a risk of infection);
- household and industrial injuries.
Pathogenesis
Hematocele is formed:
- as a result of traumatic damage to the scrotum;
- due to a puncture of a blood vessel during a puncture of the testicular sheath (for example, during a procedure to remove fluid contents in patients with hydrocele);
- when taking material for testicular biopsy in patients with chronic hemorrhagic inflammation of the vaginal membrane, which is accompanied by hemorrhage into the intershell space and the formation of granulation tissue with a dense capillary network on the inside of the membrane.
At the heart of the development process of hematocele is damage to the integrity of the blood vessel without an open wound surface. Against the background of increased pressure, blood flows out and accumulates between the membranes, in the cavity. Partially leaked blood seeps through the surrounding tissues, causing a characteristic discoloration of the skin of the scrotum. Under the influence of the breakdown of erythrocytes, the color gamut can change.
Over time, small-sized hematoceles can dissolve, or undergo a series of sequential pathological changes. During the autopsy of the "fresh" hematocele, there is no change in the color and structure of the blood (rarely, the blood becomes thicker under the influence of platelets). [5]
When an old hematocele is opened, a change in the color shade and density of the blood is observed, which becomes maroon or even black. In the case of infection, suppuration begins, and the cavity between the membranes is filled with purulent exudate.
With the development of atrophic processes, tissue degeneration occurs, with a deterioration in blood circulation and a decrease in the size of the affected testicle.
Symptoms of the hematocele
The clinical picture of hematocele as a whole depends on the period of the course of the disease. At the initial stage, clotted blood can be found in the tissues, and at later stages clots of old, "old" blood are revealed. Over time, such blood clots undergo structuring: in combination with an increase in the volume of connective tissue, this entails a deterioration in the blood supply to the testicle. If medical care is not provided, the process leads to atrophy.
Hematocele can be accompanied by a large number of symptoms, manifested separately or combined with each other.
The most common symptoms are:
- The appearance of pain in the zone of development of hemetocele. Pain occurs more often gradually, as the pressure on the surrounding tissues increases. Depending on the presence of the inflammatory process, the nature of the pain can be from acute stabbing to mild aching. Pain sensations can be given to the groin area, leg on the affected side, and also to the pelvic organs.
- Discoloration of the skin. The skin in the area of the scrotum on the affected side changes color from reddish to purple. Often, the color intensity reflects the stage of the pathological process: for example, at the initial stage, a barely noticeable redness can be observed, which gradually increases and changes. If blood circulation is impaired, a bluish tint appears.
- An increase in the size of the scrotum associated with edema, the accumulation of blood between tissues. The sizes often increase slightly, and pronounced edema indicates impaired blood circulation.
- Erectile dysfunction due to pain and other pathological symptoms.
- Violation of fertility associated with a change in the nature of the seminal fluid due to a long-standing focus of hemetocele and formed chronic pathological processes.
- Itching, manifested against the background of swelling and / or an infectious process.
Systemic signs can be:
- an increase in body temperature (with the addition of an infectious and inflammatory process);
- deterioration in general well-being, decreased performance and exercise tolerance (with the development of intoxication).
Against the background of the development of complications, additional pathological signs may be detected:
- fever, fever;
- signs of intoxication, anemia;
- change in testicular density, decrease or increase in size;
- apathy, general weakness, irritability, sleep disturbance;
- a decrease in libido, caused, both directly by pathology, and by a background decrease in testosterone production;
- impaired fertility, infertility.
Typical first signs of a hematocele are:
- swelling of the scrotum;
- prolapse of the scrotum;
- discoloration of the skin in the scrotal region to reddish and purple;
- pain syndrome in the testicular area.
Temperature readings usually remain within the normal range (if there is no accession of the infectious process). If medical care is not provided, complications often develop in the form of orchitis, epididymitis, etc.
Any of the above signs is considered more than a good reason for an urgent visit to a specialist - a urologist. It is important to consult a doctor in a timely manner, not only if hematocele develops after injuries and surgical procedures, but also for no apparent reason. Hematocele of unknown origin may be the result of an increasing neoplastic process. In particular, a testicular tumor may be the culprit. [6]
Stages
The scale and nature of pathological changes is varied, depending on the term for the existence of hematocele.
At the initial stage, clotted blood is found, after a while - brownish "old" blood and a substance of a mushy consistency. Even later, the formation of blood clots with pronounced connective tissue proliferation is noted, and in some patients - with the appearance of calcareous, cartilaginous or bone plaques.
At a later stage, as a result of pressure on the surrounding tissues and circulatory disorders in the testicle, atrophic degenerative processes can develop, characterized by a gradual decrease in the size of the testicle. This, in turn, entails a permanent reduction in the production of the male hormone testosterone and seminal fluid.
Forms
The classification of hematocele is carried out in order to divide them into groups, select therapeutic tactics, determine the appropriateness of the operation, assess the prognosis of pathology.
Practitioners point out the following types of hematocele:
- By localization - in the lungs, in the tissues of the scrotum, in the pelvic region (pelvic, parametric hematocele).
- By the nature of the damaged vessels (small-vascular, large-vascular hematocele).
In addition, hematocele is distinguished by the complexity of the pathology:
- mild form (minor damage that does not require treatment);
- moderate form (a focus of considerable size, requires conservative therapy);
- severe form (a large focus, characterized by significant size, proceeding with possible complications, requiring surgical intervention).
In general, scrotal injuries are categorized as follows:
- Grade I - hematocele without visible damage to the testicle and its membranes.
- II degree - hematocele with rupture of the albuminous membrane without visible damage to the testicle.
- III degree - rupture of the protein membrane with a loss of the parenchyma of less than half of the volume.
- IV degree - rupture of the parenchyma with the loss of more than half of the volume.
Complications and consequences
Post-traumatic hematocele can lead to the development of temporary infertility, which sometimes lasts up to several months. In the future, sperm production is most often restored, but the worst development of events is not excluded. Experts suggest that severe trauma can even lead to inhibition of testosterone production and its active transformation into estradiol, which can entail not only a disorder in the production of seminal secretions, but also a deterioration in potency.
Another possible complication of hematocele is an infectious process involving testicular tissue. The inflammatory reaction can also spread to the surrounding tissues: appendages, spermatic cord, etc.
Inflammatory process of the epididymis (epididymitis) is accompanied by severe swelling and pain in the scrotum. On ultrasound, there is an increase in epididymis, hypoechogenicity (against the background of hematocele, echogenicity increases). If untreated, epididymitis is complicated by orchitis and abscess.
An inflammatory reaction in the testicular tissue (orchitis) occurs as a result of trauma or hematocele, and the infection can spread retrograde from the prostate or bladder through the vas deferens. Inflammation usually originates in the epididymis, but soon passes directly to the testicle, so the pathology is often diagnosed as epididymitis orchiditis. The isolated form of orchitis is less common and occurs due to hematogenous infection. [7]
On ultrasound, orchitis looks like enlarged testicles with preserved homogeneity of the internal structure, or there is a blurred fuzzy parenchymal pattern against the background of the normal configuration of the organ. With a strongly pronounced inflammatory process due to edema, the parenchyma may have a homogeneously reduced echo density, or an inhomogeneous density. Acute orchitis on Doppler ultrasonography demonstrates increased circulation.
In the presence of atrophic changes, the testicular echo density remains low, and a weakening of blood flow is recorded.
Acute inflammation can trigger the development of an abscess.
Diagnostics of the hematocele
When making a diagnosis of hematocele, most often they mean the pathological accumulation of blood between the visceral and parietal sheets, localized near the vaginal membrane of the testicle. In addition, blood may also be present in the scrotum. In the first example, they talk about intravaginal pathology, and in the second, about extravaginal pathology.
The accumulation of blood - testicular hematocele - requires careful differential diagnosis, and especially if it is not possible to find out the causes of the pathology. Even with a minimal suspicion of a tumor process or with the slightest doubt, the doctor should refer the patient to narrow specialists for further detailed diagnostics. The sooner the cause of the disease or the tumor process is identified, the more favorable the prognosis will be, and the easier the treatment will be.
Rapid diagnostic appointments will relieve a man of excessive neuropsychic stress due to a long wait.
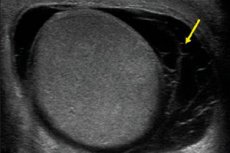
Currently, ultrasound is considered the most optimal way to diagnose hematocele. This procedure is non-invasive, quick and painless, helps to assess structural and functional changes, and can be performed several times without any harm to the patient. However, any study is performed only after a thorough history taking, an assessment of the symptoms of the disease, examination and palpation of the area of the pathological focus.
For ultrasound diagnostics, sensors with a radiated frequency of at least 5-10 MHz are used. If the area of the scrotum is sharply painful (with orchitis, epididymitis), then local superficial anesthesia may be required. Vascular studies are performed using color Doppler imaging. Power Doppler is used to assess the condition of the testicular parenchyma.
Echography is prescribed for scrotal injuries, for any increase in size and configuration disturbances, with a local increase in temperature, with a change in skin color, with pain, with the detection of atypical palpable formations, with suspicion of hematocele and other similar pathologies. Additionally, it is possible to prescribe an ultrasound of blood flow through the vessels of the testicle and along its parenchyma.
On ultrasound, mature testes normally have a smooth rounded surface, a homogeneous fine-grained structure with an average echo density. The mediastinum is clearly seen as a line of high echogenicity in the sagittal plane. The epididymis is better defined with longitudinal scanning: it is located along the posterior border and has a club-like shape. It defines the head, body and tail, without clearly defined anatomical boundaries. The body of the epididymis is flattened, and its tail flows into the vas deferens. Ultrasound examination helps to detect tumor processes, inflammatory reactions, hydro and hematocele. A healthy testicle and epididymis are surrounded by a protein and serous membrane. The albuminous membrane is represented by a thin continuous stripe with a high-intensity reflected echo signal. The physiological fluid in the scrotum has a volume of 1-2 ml and has the form of an echo-negative bracket with a size of 1 to 3 mm in the area of the superior testicular pole. [8]
With an asymmetric lesion, the diagnosis begins with a reference point to the healthy side. Be sure to examine the area of the scrotum from the front and back.
Usually, an ultrasound scan is sufficient to diagnose and prescribe appropriate therapy. Only in some cases, to clarify some points, they connect computed and magnetic resonance imaging, Doppler scanning of testicular vessels.
In severe injuries that provoked the appearance of a hematocele, it is often necessary to refer the patient for an operation to revise the testicle.
Analyzes
General clinical laboratory tests are not required for hematocele. But they allow the doctor to diagnose concomitant pathology in the body, to track the course of the treatment.
It is possible to take such material for analyzes:
- blood;
- urine;
- ejaculate;
- a smear from the urethra.
Information obtained in the course of general clinical diagnostics often does not indicate any specific disease, but shows the state of the body as a whole, helps to narrow the diagnostic search.
With hematocele, it is possible to carry out such laboratory tests:
- general urine analysis;
- study of discharge from the genitourinary organs;
- microscopy of discharge from the genitourinary organs;
- general clinical analysis of prostate secretion;
- spermogram (semen analysis);
- blood test (hemoglobin content, quantity and quality of erythrocytes and leukocytes, erythrocyte sedimentation rate, assessment of the quality of blood coagulation, etc.).
To assess the state of the genitourinary system, the following indicators are considered:
- physical properties of urinary fluid (color, density, transparency, odor);
- the presence of protein in the urine (as well as urobilin, hemoglobin, glucose, acetone);
- sediment study.
Instrumental diagnostics
For traumatic injuries that require urgent surgery (for example, ruptured testicles, extensive hematoma), early diagnosis helps prevent such persistent complications as ischemic atrophy and infectious processes.
Damage to the scrotum on echography shows signs of hematocele - sometimes in the form of post-traumatic epididymitis, epididymic hematoma, testicular infarction or hematoma, testicular hyperemia, swelling and rupture. If there is a rupture, then echographically shows a "broken" line, testicular fragmentation, a violation of the configuration and echo density. With extensive hemorrhage, the use of color Doppler mapping is required to assess the state of the vasculature and determine the tactics of surgical intervention.
On echography with hematocele, fluid heterogeneity is noted, a large number of small moving echogenic structures is determined in the lumen.
Echography for scrotal injuries is prescribed to characterize damage, to confirm or exclude testicular rupture (which further helps to assess the prognosis of pathology), to distinguish hematocele from soft tissue hematoma, to monitor the dynamics of patient recovery after surgery, or to determine indications for drug treatment. [9]
Differential diagnosis
Hematocele should be distinguished from other benign formations (cysts, hydrocele, spermatocele, tuberculous or non-tuberculous epididymo-orchitis, varicocele, inguinal hernia, syphilitic gum) and from malignant processes (carcinoma, lymphoma).
Epididymal cysts are found mainly in middle-aged patients. Such cysts are multiple and often bilateral. Outwardly, they are defined as fluctuating elements that can be palpated in the back of the testicle, separate from itself. It happens that the cyst is displaced to the front: in such patients, it is felt in front of the testicle.
Spermatocele has a lot in common with cystic formations. It is characterized by the location above the testicles in the area of the vaginal membrane.
Hydroceles are formed by the accumulation of liquid contents in the cavity of the vaginal membrane. Such a disease can be primary or secondary: the primary pathology is most often idiopathic (without an obvious cause), and the secondary one usually becomes a consequence of tumor processes, trauma and infectious diseases. The clinical picture of a hydrocele is as follows: the edematous area around the testicle is palpable, in some cases the testicle is not palpable. When the testicle is translucent, light is transmitted.
Hematocele is the accumulation of blood in the cavity of the vaginal membrane. Pathology can be the result of trauma, or it can be a complication of testicular carcinoma. Symptomatically, a hematocele is similar to a hydrocele, however, when the testicle is translucent, no light is passed through. In the absence of treatment, the hematocele subsequently shrinks and becomes denser: at this stage, the disease should be distinguished from testicular carcinoma.
The tuberculous form of epididymo-orchitis is relatively rare. The main manifestations of this pathology are the formation of a dense, not very intense edema of an irregular configuration, a thickening of the vas deferens. Often the movement of the testicles in the scrotum is limited.
With a non-tuberculous form, generalized edema of the epididymis and testicle occurs. But regardless of the presence of pain, such a disease has many clinical signs of a tumor process, which also requires differentiation.
Varicocele is also accompanied by an enlargement of the testicle, but its cause lies in the expansion of the uviform branches of the internal spermatic vein or the spermatic venous vessel itself. Varicocele is better diagnosed when the patient is upright. If the development of such a process is too rapid, then you can think about the existence of renal cell carcinoma. [10]
An inguinal hernia differs from a hematocele in the impossibility of probing the upper border and a positive breakdown of the cough impulse.
As for malignant tumors, they are most often found in men from 20 to 40 years old. The most common development of such processes occurs from the germ cells, as a result of which a teratoma or seminoma is formed. Tumors are thickened edema that covers all parts of the testicle. Many patients complain of severe pain.
Lymphoma is more common in old age.
An enlarged, painful and reddened scrotum can also indicate damage to other organs, even those that are located relatively far from the external genitalia. For example, blood can flow into the scrotum as a result of abdominal trauma, and in newborns, due to adrenal hemorrhage.
If a man seeks medical help with signs of hematocele, then the doctor must carefully take an anamnesis and complete all stages of the local and general examination. This will help to confidently make the correct clinical diagnosis.
Treatment of the hematocele
With a small hematocele, treatment may be limited to conservative measures:
- applying ice compresses, dry ice to the scrotum area;
- taking analgesics, anti-inflammatory drugs;
- providing absolute rest for several days, complete rejection of physical activity for the entire period of treatment.
If there is a risk of secondary infection, then antibiotic therapy is prescribed. After normalization of the patient's condition and the disappearance of acute signs of hematocele, it is possible to use physiotherapy, the action of which is aimed at resolving the problematic accumulation of blood (magnetotherapy, ultrahigh-frequency therapy).
If the conservative technique turns out to be ineffective, they resort to surgical treatment. The type of surgery and the technique for its implementation are selected depending on the size of the hematoma, the patient's age, and the presence of complications. [11]
Conservative therapy consists of the following activities:
- the use of a suspensor;
- applying cold to the scrotum;
- taking analgesics and non-steroidal anti-inflammatory drugs;
- strict bed rest for at least two days;
- prescribing antibiotic therapy if you suspect the development of epididymitis or an infectious process in the genitourinary system;
- if conservative treatment is ineffective, repeated ultrasound and Doppler ultrasound is required.
The scrotum revision is assigned:
- if it is impossible to determine the diagnosis;
- if there are symptoms of testicular damage;
- when the protein shell is destroyed;
- with an expanding focus of hematocele, or with the development of massive bleeding;
- in the absence of blood flow according to the information of ultrasound with color Doppler mapping.
First aid for hematocele consists in the following actions:
- Cold is applied to the damaged area (ice wrapped in a towel to prevent frostbite) in order to narrow blood vessels and inhibit the inflammatory process. A cold compress is applied every 3-4 hours, holding for about 15-20 minutes.
- Give the patient an analgesic (Ibuprofen, Analgin, Nimesil).
- Provide the victim with maximum rest in a horizontal position.
A man with a hematocele must be examined by a doctor. After the diagnosis, he will prescribe the necessary therapeutic measures. [12]
Medicines
Medicines are prescribed in accordance with the cause of the development of hematocele, which is determined by a specialist during the diagnosis.
With the infectious nature of the pathology, antibacterial or antiviral medicines are used, taking into account the resistance of microorganisms. If a sexually transmitted infection is detected, then treatment is prescribed depending on the pathological pathogen. The non-specific nature of hematocele requires the use of antibiotics of a broad spectrum of activity, with a selection from several groups.
|
Ibuprofen |
Non-steroidal anti-inflammatory agent, eliminates pain and inhibits the development of the inflammatory process. The tablets are taken orally whole with water, 1-2 tablets no more than three times a day. It is undesirable to take the drug for more than five days in a row, due to its irritating effect on the mucous membrane of the digestive tract. |
|
Nimesulide |
An anti-inflammatory and analgesic drug intended for oral administration (the term of treatment with Nimesulide is no more than 15 days). As a rule, 100 mg of the drug is taken twice a day after meals. Possible side effects: abdominal pain, nausea, diarrhea, dizziness. |
|
Actovegin |
A drug that stimulates tissue metabolic processes, improves trophism and tissue regeneration. It is taken orally before meals - on average, 2 tablets three times a day. Treatment can be long - up to several months. Possible side effects: allergic reactions. |
|
Dipyridamole |
An antiplatelet agent, an antithrombotic drug that is used during the recovery phase after an injury. If there is a tendency to bleeding (hemorrhagic diathesis), then the drug is not prescribed. It is taken orally between meals, without chewing, with water, 1-2 tablets three times a day. The duration of therapy is determined individually (from several weeks to six months). Possible side reactions: allergies, headache, tremors, tachycardia, abdominal discomfort. |
|
Troxerutin |
Angioprotective, capillary stabilizing drug. It is taken orally after meals, in an average dosage of 2 capsules per day. Treatment can be lengthy. Possible side effects: allergic reactions, headache, sleep disturbances, abdominal pain, nausea. |
In general, conservative treatment includes:
- elimination of symptoms (most often the patient complains of severe pain, which is quite effectively "removed" by analgesics);
- elimination of the immediate cause of the violation (if possible);
- creation of conditions conducive to therapy (bed rest, movement restrictions, applying a bandage or suspensor, use of angioprotectors);
- the use of physiotherapy.
Physiotherapy treatment
Physiotherapy can be an effective adjunct method for the treatment of hematocele, along with drug therapy, as well as a means to accelerate the body's recovery after surgery.
Today, medicine offers a lot of procedures and medicines that can be used for hematocele. However, many drugs exert a rather powerful load on the body and cause the development of side effects. It is also possible that the patient has contraindications to the use of certain drugs. In addition, the effect of medications may not be effective enough, since the active substance with the bloodstream cannot get in the required amount to the affected tissues. If you combine conservative treatment with physiotherapy, then, thanks to an integrated approach, you can achieve a significant improvement in the well-being and quality of life of a man, and with the minimum possible drug load on the body. Physiotherapy procedures improve blood circulation, lymph circulation, accelerate metabolism in the area of exposure.
The effect of physiotherapy is based on the absorption of physical energy by the tissues of the body and its transformation into biological reactions. It is optimal to undergo a course of electrical, radiation or magnetic therapy in order to achieve the desired success. If, simultaneously with the procedure, the patient receives a drug, then it accumulates mainly in the pathological focus, getting directly to the diseased organ.
During the recovery period after hematocele (including after surgery), the patient is prescribed phonophoresis of therapeutic mud, electrotherapy with pulsed currents, interstitial magnetic laser electrophoresis of enzyme preparations.
Herbal treatment
People often use alternative methods to speed up the healing of hematoceles. We present to your attention the most popular recipes:
- A fresh leaf of white cabbage is beaten off with a hammer for meat, applied to the scrotum and kept for at least 1.5-2 hours. You can fix the sheet with compression underwear.
- Arnica infusion is used for internal use and for the formulation of compresses. The infusion is prepared as follows: one teaspoon of flowers is poured with hot water and infused for two hours. Instead of flowers, you can also use the root of the plant. The tool is used for cool compresses, and is also taken orally, 50 ml three or four times a day, between meals.
- A fresh plantain leaf is washed, lightly crushed with your fingers and applied to the damaged area (scrotum), it is possible at night. Additionally, you can take inside the pharmacy tincture of plantain (according to the instructions).
- Aloe leaf and honey compress is prepared as follows: aloe leaves are ground or passed through a meat grinder, mixed with honey. Used for compresses at night, once a day.
- Fresh cucumbers are cut into circles and applied to the scrotum, fixed with a bandage or compression linen. The minimum retention of the product on the affected area is 30 minutes. You can repeat the procedure several times a day.
- Fresh banana peel is applied to the site of the hematocele, with the inside to the skin. This remedy helps to eliminate pain and speed up the resorption of blood accumulations.
With a small hematocele, alternative methods help no worse than modern drugs, and without any side effects. Most of the proposed recipes are quite simple and affordable.
Surgery
The minimum volume of hematocele, at which surgery is indicated, has not been determined by specialists. But most surgeons believe that if the size of the pathological focus does not exceed 1/3 of the diametrical size of the testicle, then wait-and-see tactics with medical management of the pathology can be used. There is no need for surgery if there is little
Hematocele without a picture of testicular rupture. The combination of a hematocele (regardless of its size) with an intra-testicular hematoma is always regarded as an indication of testicular rupture, even if there are no echographic signs of rupture.
However, there is evidence of insufficient information content of echography. For example, testicular rupture was accurately identified by ultrasound scanning in only 50% of cases. To avoid mistakes, experts recommend early surgery if testicular rupture is suspected.
The operation is prescribed with a large volume of blood flowing out, with the development of a purulent process or calcification. It is optimal to carry out the intervention as early as possible: the less time has passed since the development of hematocele, the greater the chances of preserving the testicle itself and its function. In old cases, the surgeon has to perform orchiectomy - an operation to remove the testicle.
Surgical manipulations can be as follows:
- stopping bleeding, removing the outflowing blood;
- removal of necrotic areas;
- applying seams to the fabric of the shell;
- returning the testicle back to the scrotum;
- torsion correction, restraint release;
- suturing of tissues with impaired integrity, damaged vessels;
- in some cases, partial or complete removal of the testicle.
After surgery, a man can be left in hospital for a period of 5 to 8 days, which depends on the complexity of the violation and on the volume of the operation. The drains are removed after a few days. The patient is discharged home with the condition of a mandatory repeated visit to a specialist for examination and consultation.
Prevention
Hematocele is a serious pathology that requires urgent medical attention and comprehensive diagnostics. The long-term consequences of undiagnosed hematocele can be abscesses, other inflammatory and atrophic processes, erectile dysfunction, etc.
Violation can be prevented if:
- protect the genitals during traumatic sports;
- to raise the level of sexual culture and sex education;
- be careful with pets;
- avoid traumatic sexual positions;
- entrust the conduct of therapeutic and surgical procedures only to qualified, experienced specialists.
It is equally important to follow simple preventive rules to keep the genitals and circulatory system healthy:
- be physically active, avoid physical inactivity;
- eat right, include in the daily diet foods rich in minerals, vitamins, useful microelements, proteins;
- promptly treat any pathologies of an infectious and inflammatory nature;
- quit smoking and drinking alcohol;
- have a regular sex life with a trusted partner, avoid unprotected sex and interrupted sexual intercourse;
- prevent overheating or hypothermia of the body.
If you follow all the recommendations proposed, then you can minimize the risk of developing hematocele and other lesions of the genitourinary system. But we must not forget that with any suspicion of pathology, it is important to visit a doctor as early as possible. Early diagnosis and proper treatment will help avoid complications.
Forecast
The prognosis of the disease as a whole and completely depends on the duration of its course. At the initial stage, the doctor determines only a blood clot, and at a later stage, the presence of seals is noted, which are structured over time. In combination with an increasing volume of tissues, the pathological process entails a deterioration in the blood supply to the testicle, which can subsequently lead to its complete atrophy. [13]
Before proceeding with the treatment of hematocele, you need to understand that in some patients, the accumulation of blood can disappear by itself, without any intervention. However, this is not always the case. Many men have to carry out a whole range of activities, including drug therapy. An ice compress is applied to the scrotum, analgesics and anti-inflammatory drugs are prescribed. The patient is prescribed a gentle bed rest, complete rest with the maximum possible limitation of motor activity. With pronounced hematocele, a puncture is performed, which is often ineffective, and even worse - it can provoke repeated bleeding or the development of a purulent process. If it is not possible to remove the blood that has poured into the cavity, then they resort to surgical intervention to avoid testicular atrophy. With proper timely treatment, the prognosis is considered favorable.

