Blood in the smear
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Blood in the smear after a gynecological examination can be normal, but it can indicate a serious pathology. It is necessary to distinguish between conditions in which blood in a smear can be a dangerous symptom. To do this, you need to consider all possible options and reasons for this problem.
Morphological features of a blood smear
Most women after the examination at the gynecologist receive usual results of smears, but many do not know what to do with the results when they return abnormal. However, abnormal results usually do not indicate a serious pathology. Knowing the causes of an abnormal smear and protecting against the risk factors associated with this result can lower your chances of a serious uterine pathology.
The causes of the appearance of blood in the smear depend on which cells are found in this smear mainly. After all, the blood consists of different cells, and each performs its function. Accordingly, the detection of predominantly one or another cell indicates a certain pathology.
Leukocytes in the blood smear are the most important cells that protect the human body. All leukocytes have nuclei that distinguish them from others. There are five types of leukocytes. They fall into two main classes: granulocytes (including neutrophils, eosinophils and basophils) and agranulocytes (including lymphocytes and monocytes). This classification depends on whether granules can be isolated in their cytoplasm using a light microscope and conventional staining techniques. All leukocytes are able to move like an amoeba and can migrate from blood vessels to surrounding tissues.
The level of leukocytes is often an indicator of the disease, and, therefore, their calculation is an important indicator of blood. The normal level of leukocytes in the smear of peripheral blood is usually from 4,000 to 10,000 leukocytes per microliter of blood. They make up about 1% of the total blood volume in a healthy adult, which makes them significantly less numerous than red blood cells by 40-45%. This is normal when it is part of a healthy immune response that occurs frequently. This is sometimes abnormal when it is neoplastic or autoimmune in origin. A decrease below the lower limit is called leukopenia. This indicates a weakened immune system.
Leukocytes in a gynecological smear can also be in a small amount, but their number should not exceed 10 cells. If their number is larger, one can think of inflammatory changes in the cervix or uterus.
Platelets in the blood smear are a component of the blood, the function of which (along with the factors of blood coagulation) is to stop bleeding by starting blood clotting in blood vessels. Platelets do not have a cell nucleus: they are fragments of the cytoplasm, which are obtained from the megakaryocytes of the bone marrow, which then enter the bloodstream. These non-activated platelets are biconvex discoid (lenticular) structures, 2-3 μm in the largest diameter. On a stained blood smear, platelets appear as dark purple spots, about 20% of the erythrocyte diameter. A smear is used to examine platelets for size, shape, quality number and lumps. The ratio of platelets to erythrocytes in healthy adults ranges from 1:10 to 1:20.
The main function of platelets is to promote hemostasis: the process of stopping bleeding at the site of the interrupted endothelium. They gather in place and, if the interruption of the vessel is physically too large, they lock the hole. First, platelets attach to substances outside the interrupted endothelium: adhesion. Secondly, they change shape, include receptors and secrete chemical messengers: activation. Thirdly, they are connected to each other through receptor bridges: aggregation. The formation of this platelet plug (primary hemostasis) is associated with activation of the coagulation cascade with the resultant precipitation of fibrin and binding (secondary hemostasis). The end result is a clot.
A low concentration of platelets is thrombocytopenia and is caused either by a decrease in production, or by an increase in fracture. An increased concentration of platelets is a thrombocytosis and either congenital or due to unregulated production.
The concentration of platelets is measured either manually using a hemocytometer, or by placing blood in an automated platelet analyzer. The normal range of these cells in the peripheral blood is 150-400 thousand per microliter.
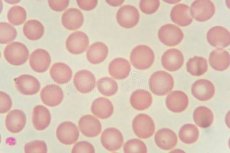
Erythrocytes in the blood smear are the most common type of blood cells and the main means for delivering oxygen to the body tissues through the circulatory system. The erythrocyte cytoplasm is rich in hemoglobin, an iron-containing biomolecule that can bind oxygen and is responsible for the red color of cells. The cell membrane consists of proteins and lipids, and this structure provides the properties necessary for the physiological function of cells, such as stability in circulating the circulatory system and, in particular, the capillary network.
In humans mature erythrocytes are flexible and oval biconvex disks. They do not have a cell nucleus and most organelles to accommodate the maximum space for hemoglobin; they can be considered as bags with hemoglobin. Approximately 2.4 million new red blood cells are produced per second in adults. Cells develop in the bone marrow and circulate for about 100-120 days in the body before their components are recycled by macrophages. Each treatment takes about 60 seconds (one minute). About a quarter of the cells in the human body are red blood cells.
When red blood cells undergo stress in narrowed vessels, they release ATP, which causes the vessel walls to relax and expand to promote normal blood flow. When hemoglobin molecules are deoxygenated, erythrocytes release S-nitrosothiols, which also act to dilate the blood vessels, thereby directing more blood to the area of the body depleted of oxygen.
Erythrocytes can also synthesize nitric oxide enzymatically, using L-arginine as a substrate, like endothelial cells. The effect of red blood cells on physiological levels of shear stress activates nitric oxide synthase and the export of nitric oxide, which can contribute to the regulation of vascular tone.
Erythrocytes also play a role in the immune response of the body: when lysing with pathogens such as bacteria, their hemoglobin releases free radicals that destroy the cell wall and the pathogen membrane, killing it.
Women have about 4-5 million erythrocytes per microliter (cubic millimeter).
Reticulocytes in the blood smear are immature erythrocytes, usually amounting to about 1% of erythrocytes in the human body. In the process of erythropoiesis (formation of erythrocytes) reticulocytes develop, and then circulate about a day in the bloodstream, and then develop into mature red blood cells. They are called reticulocytes because of the reticular network of ribosomal RNA, which becomes visible under a microscope with certain spots. Reticulocytes appear slightly more blue than other red blood cells. The normal proportion of reticulocytes in the blood depends on the clinical situation, but usually ranges from 0.5% to 2.5%. This percentage is in the normal range with a normal level of red blood cells; for example, if someone is anemic, but has a percentage of reticulocytes as low as 1%, the bone marrow probably does not produce new blood cells at a rate that will correct anemia.
The amount of reticulocytes is a good indicator of bone marrow activity, as it is a recent production and allows you to determine the number of reticulocytes and the index of production of reticulocytes. These values can be used to determine if the production problem affects anemia, and can also be used to monitor the progression of anemia treatment.
Mononuclear cells in a blood smear are any cell of peripheral blood that has a round nucleus. These cells consist of lymphocytes (T cells, B cells, NK cells) and monocytes. Mononuclear cells are the largest type of leukocytes and can differentiate into macrophages and myeloid lines of dendritic cells. In humans, lymphocytes form the majority of the mononuclear population, followed by monocytes and only a small percentage of dendritic cells. Monocytes are produced by the bone marrow from precursors, called monoblast, bipotent cells, which differentiate from hematopoietic stem cells. Monocytes circulate in the bloodstream for about one to three days, and then usually move to tissues throughout the body, where they differentiate into macrophages and dendritic cells. They make up three to eight percent of the white blood cells in the blood. About half of the body's monocytes are stored as a reserve in the spleen. Monocytes that migrate from the blood to other tissues will then differentiate into resident tissue macrophages or dendritic cells. Macrophages are responsible for protecting tissues from foreign matter, but are also suspected of the importance of forming important organs such as the heart and the brain. These are cells that have a large smooth nucleus, a large cytoplasmic area, and many internal vesicles for processing foreign matter.
Mononuclear cells perform three basic functions of the immune system. This is phagocytosis, antigen presentation and production of cytokines. Phagocytosis is the process of absorbing microbes and particles with subsequent splitting and destruction of this material. Monocytes can perform phagocytosis using intermediate (opsonizing) proteins, such as antibodies or complement, that cover the pathogen, and also by binding to the microbe directly through the pattern recognition receptors that recognize the pathogens. Monocytes are also capable of killing infected cells through antibody-dependent cell-mediated cytotoxicity.
Eosinophils in the blood smear are one of the components of the immune system responsible for combating multicellular parasites and certain infections. These cells are eosinophilic or "acid-loving" because of their large acidophilic cytoplasmic granules, which show their affinity for acids. Inside the cells there are small granules that contain many chemical mediators, such as eosinophilic peroxidase, ribonuclease (RNase), deoxyribonuclease (DNase), lipase. These mediators are released by a process called degranulation after eosinophil activation, and are toxic to parasite tissues.
Eosinophils account for about 1-3% of white blood cells. Eosinophils persist in the circulation for 8-12 hours and can survive in the tissue for another 8-12 days in the absence of stimulation.
There are also eosinophils that play a role in the fight against viral infections, which is evident due to the abundance of RNase that they contain within their granules, and when fibrin is removed during inflammation. Eosinophils, along with basophils and mast cells, are important mediators of allergic reactions and the pathogenesis of asthma and are associated with the severity of the disease.
Causes of blood in the smear
It is natural to have blood in a smear after a vaginal examination, because although it is a non-traumatic method, there may be slight damage to the endothelial mucosa. This happens both with pregnant women, and with women who are not pregnant. The cervix and the vaginal area are very tender and have blood cells very close to the surface. During routine routine smear, even normal cleansing can cause slight bleeding. Usually bleeding stops on its own. But if the blood in the smear in a significant amount and there are different blood cells, then you need to look for the cause of this condition.
Why is a smear test performed in women? With each preventive examination, a swab is taken for examination. The very concept of "preventive examination" suggests that this is done with the purpose of timely exclusion of any pathology. Cervical screening is the process of detecting abnormal tissue. In an effort to detect and treat early neoplasia, screening is aimed at secondary prevention. Several screening methods are a test for Pap (also known as Pap smear), liquid-based cytology, HPV DNA testing and visual control with acetic acid. Promising screening methods that can be used in low-resource areas in developing countries are testing HPV DNA and visual inspection.
Usual cytology allows to reveal cells and to suspect a pathology.
The causes of the appearance of blood in a gynecological smear in women of reproductive age are as follows:
- Hormonal imbalance;
- Tubal or ectopic pregnancy (during examination, improper fixation of the embryo may cause partial or complete delamination of the placenta and bleed);
- Placenta growth - pregnancy, when the placenta lies near or near the cervix;
- Myoma of the uterus (the nodular form often bleeds when examined);
- Some types of cysts and tumors (for example, polyps are finger-shaped cervical protuberances filled with blood that can bleed);
- Endometriosis (involves the location of areas of the endometrium outside the uterine cavity, which are prone to periodic bleeding);
- Use of contraceptives (in non-pregnant women, bleeding is more likely if you take birth control pills that increase hormone levels and make the cervix more sensitive);
- Intrauterine spirals (create the risk of additional trauma);
- Infections: Vaginitis can be caused by yeast, bacteria and trichomonads.
In postmenopausal women, the causes of the appearance of blood in a smear can be limited to the following cases:
- The effect of hormone replacement therapy;
- Cervical cancer or other localization;
- Some tumors (not cancerous);
- Atrophic vaginitis (makes the mucous membrane very dry and easily traumatized).
Risk factors
Risk factors for the appearance of blood in the smear during pregnancy are higher, but in such cases it is often not caused by pathology. In pregnant women, blood vessels are more sensitive and bleed easier. Pregnant women need a smear during the early stages of pregnancy as part of routine prenatal testing.
Clinical manifestations of pathologies accompanied by abnormal smear
When it comes to this or that pathology of the female sexual sphere, the symptoms may not appear immediately. Therefore, it is so important to conduct an annual examination with a smear test. But sometimes there are manifestations of pathologies that a woman does not pay attention to.
Blood when taking a swab from the cervical canal may appear when the woman has a secretory phase of the cycle and the vessels are superficially placed. But if we talk about pathology, the blood can appear in cancer. It is associated with abnormal growth of cells that have the ability to penetrate or spread to other parts of the body. The first signs are most often local changes, which are determined in the smear. Later symptoms may include abnormal vaginal bleeding, pain.
Human papillomavirus infection causes more than 90% of cases.
Vaginal bleeding, contact bleeding (one of the most common forms of bleeding after intercourse) or (rarely) vaginal mass may indicate the presence of malignancy. With a common disease, metastases can be present in the abdominal cavity, lungs or elsewhere.
Another reason that the blood after a smear for cytology, can be a benign tumor, myoma of the uterus. Myoma of the uterus is a node of smooth muscle cells and fibrous connective tissue that develops in the wall of the uterus. Nodules can grow inside the uterine wall, or they can project into the inner cavity or the outer surface of the uterus. Most fibroids are found in women of reproductive age, and they are rare in young women.
The first signs of uterine fibroids can appear only when it reaches significant dimensions. If a woman is not examined on time, then the fibroid is detected late. Symptoms of fibroids may appear as bleeding after taking a smear. This is due to the fact that the node is traumatized, which causes a small bleeding. But, nevertheless, it contributes to early diagnosis.
Endometriosis is a common cause of blood in a smear in women of reproductive age. The name of endometriosis comes from the word "endometrium," a tissue that lines the inside of the uterus. In endometriosis, tissue that looks and acts like an endometrial tissue is outside the uterus, usually inside the abdominal cavity.
At the end of each cycle, when hormones cause the uterus to secrete, the endometrial tissue that grows outside the uterus bleeds. The tissues surrounding the endometriosis area can become inflamed or swollen. Inflammation can cause scar tissue around the endometriosis area.
The most common symptom is bleeding when taking a smear. Other symptoms may include pain, especially excessive menstrual cramps (dysmenorrhea), which can be felt in the abdomen or lower back during or after sexual activity. Infertility occurs in 30-40% of women with endometriosis.
Infections are one of the reasons that can cause vaginitis of varying severity. Chlamydia are pathogens that can cause vaginitis. These parasites are located inside the cells, so when researching a smear they can rarely be detected. Symptoms in women may include vaginal discharge, including bloody. In women of reproductive age, this pathogen can cause infertility. But since it is difficult to detect in a smear from the vagina, there is a need to conduct a blood test for the pathogen even with a negative cytological smear. When there are antibodies to chlamydia in the blood, there is no smear in the smear, this indicates that the woman has an active chlamydial infection.
A similar situation with ureaplasma. The causative agent also refers to intracellular parasites, so if antibodies to ureaplasma in the blood, and in the smear, there is still an infection in the body.
Trypanosome in a blood smear is a symptom of a serious illness. The trypanosome is the genus of unicellular parasitic flagellated protozoa. Most species are transmitted by blood-sucking invertebrates, but different mechanisms exist between different species. Trypanosomes infect many hosts and cause various diseases, including fatal diseases. If this pathogen is suspected, a thorough examination, including blood tests, is performed. Since the intracellular stages of the life cycle of trypanosomes are usually found in human erythrocytes, a smear is necessarily examined, and if the trypanosome is in the smear, the diagnosis is confirmed.
Cytomegalovirus refers to intracellular persistent viruses in humans. Often, women before planning pregnancy, undergoing tests for this virus, are worried because of the results. When the cytomegalovirus is in the smear, and there is no blood in the swab, this does not indicate an active infection. After all, he can be inside the cells all his life, but the woman is not sick. Therefore, if the acute phase (M) antibodies are negative, do not worry.
The consequences and complications depend on the pathology, which caused bleeding or a bad smear. If the process is malignant, then the consequences of untreated pathology can be fatal.
Treatment
What if a bad smear for cytology? Of course, everything depends on which cells are determined. If in the cervical cytology that accompanies the sample, suspicious cells are marked, the laboratory should make a recommendation for colposcopy. Colposcopy is a procedure that looks at the uterus by increasing it under microscopic glass. The doctor can see the endometrium and the orifices of the fallopian tubes, which is not visible during routine examination. This procedure is minimally invasive and allows you to directly examine the endometrium and take a sample for biopsy.
Treatment must necessarily be etiological. If the cause of blood in a smear is confirmed cancer, then you can not delay with treatment in any case. Since cervical cancer is radiosensitive, radiation can be used at all stages. Surgical intervention may have better results than radiological approaches. In addition, chemotherapy can be used in certain stages or in combination with other methods.
Myoma of the uterus is not treated actively if it is at the initial stages of development. As a measure of growth, you can use hormonal combination drugs, and when you reach a large size - surgical treatment.
Although there are no cures for endometriosis, there are two types of interventions: the treatment of pain and the treatment of infertility associated with endometriosis. In many women, menopause (natural or surgical) will reduce this process. In women in reproductive years, endometriosis is simply controlled: the goal is to provide relief of pain, limit the progression of the process and restore or maintain fertility where necessary. In general, the diagnosis of endometriosis is confirmed during the operation, and at this time, ablative steps can be taken. Ablation of endometriosis (burning and evaporation of lesions by an electrical device) showed a high rate of short-term recurrence after the procedure.
Conservative treatment may increase the risk of relapse.
Infections that cause the appearance of blood in a smear or other type of discharge require medical active treatment. The drugs are used according to the pathogen and its sensitivity to these or other drugs. It should be borne in mind that infections of the genital tract in most cases are caused by intracellular pathogens, so the course of antibacterial drugs can be prolonged.
Alternative methods of treatment and homeopathy are not used, since active infectious processes or neoplastic are not subject to such types of treatment. If a long time to use alternative methods without drug therapy, this can lead to complications.
Prevention
Prevention of the appearance of bad tests in the cytology of the smear is the maintenance of the health of the reproductive system of a woman. It is very important to undergo preventive examinations in a timely manner, because it is a pledge of a timely diagnosed disease.
Forecast
The prognosis in most cases with the appearance of blood in the smear is positive, because it is often a normal reaction. In the presence of pathology, a smear will allow it to be sufficiently informative to determine its appearance and start treatment in time.
The appearance of blood in a smear on cytology during gynecological examination can sometimes frighten women. But this is not always so scary, because everything depends on what elements of the blood are found there. You should always wait for the full results of the examination and talk them through with the doctor, without panicking before the time and without self-medication.


 [
[