Multifollicular structure of the ovaries: causes, symptoms, diagnosis
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Quite a common conclusion of ultrasound is multifolllicular ovaries (MFN). Let's consider features of the given condition, the reasons, signs, methods of correction.
Ovaries are the paired organ of the female reproductive system, they are located in the pelvic cavity on both sides of the uterus. Relate to glands of internal secretion, produce sex steroid hormones: estrogen, androgen, progestin.
Appendages function from the moment of the end of puberty and up to menopause, performing such functions:
- Generative - the reproduction of eggs that are capable of fertilization. The cortex of appendages contains primordial follicles, in each of which egg maturation takes place. During puberty in the ovaries there are about 40,000 follicles, and after its completion, their number gradually decreases, which manifests itself in regular menstruation.
- Hormonal - provides an uninterrupted production of hormones. In this case, the secretion of estrogen and progesterone is controlled by the anterior pituitary gland. Estrogens are produced with the help of follicle-stimulating hormone in the first phase of the cycle, and the luteinizing hormone is responsible for the hormonal changes in the second phase.
- Vegetative - responsible for the development of external female sex characteristics, supports femininity.
The sex glands contain a certain number of follicles, in each of which the egg ripens. Normally, 4-7 follicles are maturing monthly, one of which is dominant and slows the development of others. It ripens an egg, ready for fertilization during the period of ovulation. If conception does not occur, the follicles dissolve, making room for the next batch.
If the number of follicles exceeds the norm, this indicates multifollicularity. The peculiarity of this condition is that the follicles do not reach full maturity. This is manifested by malfunctions of the menstrual cycle, the absence of menstruation for 6 or more months. But in some cases a large number of structural components is a variant of the physiological norm. This is typical for teenagers, when the hormonal function is not yet fully formed.
Similar is observed in women who have used hormonal contraceptives for a long period of time. In any case, a comprehensive correction of violations with the restoration of menstrual function and the elimination of related problems.
What does the multifollular ovary mean?
To describe the structure of the appendages, ultrasound specialists use such term as multifollicularity. It means a large number of structural elements of the ovary in its stroma - more than 7, and in the norm of 4-7 follicles. In this case, both organs look the same.
At the given conclusion the special attention is given to presence of such symptomatology:
- Hormonal failures.
- Violation of the menstrual cycle.
- Drawing pains in the lower abdomen.
- Impossibility of conception is another.
Such a structure can be one of the variants of the physiological norm. But in some cases it indicates pathological processes, for example, polycystosis. To determine the cause of the appearance of a large number of follicles, differential diagnosis is carried out.
Multifollicular structure of ovaries
The condition in which there are more than 7 structural elements in the stroma of the ovaries is multifollicularity. Such multifollicular changes in the ovaries can occur due to the action of various factors or act as one of the norm variants.
There are several main causes that cause multifalllicular changes:
- Prolonged use of hormonal drugs.
- The period of puberty.
- Hereditary predisposition.
- Excess or lack of body weight.
- Disruption of the pituitary gland.
- Endocrine pathologies.
Multifollicular transformation of the ovaries is detected during ultrasound. Ultrasound determines 12 or more mature follicles. Symptoms of this condition do not always make themselves felt. Complex diagnosis is carried out to determine the nature of the MFN and the risk of complications for the childbearing function. Based on the results of the studies, corrective techniques can be prescribed aimed at restoring the normal functioning of the reproductive organs.
Epidemiology
MFN represent a large number of follicles formed once or during each menstrual cycle. Statistics indicate that about 25% of healthy women of reproductive age face this diagnosis. Of these, more than 70% have hormonal problems and excess body weight. In 11% of cases, multifollicularity leads to the development of polycystosis and more serious complications.
Causes of the multifollicular ovaries
In most cases, multifollicularity is laid down at the genetic level and manifests itself with a decrease in luteinizing hormone. Hormonal changes occur with sudden fluctuations in body weight and endocrine disorders.
The conducted studies indicate that the causes of multifollicular ovaries can be divided into external and internal ones, we consider the main of them:
- Genetic predisposition.
- Sharp changes in body weight.
- Emotional shocks, stress.
- Prolonged use of hormonal drugs.
- Use of oral contraceptives.
- Endocrine disorders.
- The period of puberty.
- Breast-feeding.
- Inflammatory and infectious diseases of the genitourinary system.
- Pituitary hypofunction.
Having established that it was the cause of the deviation, the need for medical correction is determined. If the patient is healthy and has a functioning reproductive system, then provoking factors should be eliminated. In other cases, a further examination is carried out and treatment is prescribed.
Multifolllicular ovaries after cancellation OK
Oral contraceptives are very popular, they are accepted by about 60% of women. After stopping the intake of OK in the body, changes begin:
- Ceases to act gestagens.
- The period of ovulation is accelerated.
- The gonadotropic function of the pituitary gland is restored.
Against this background, a large number of luteinizing and follicle-stimulating hormones are produced. Within 2-3 months the reproductive function is restored and the menstrual cycle is stabilized.
As a rule, contraceptives are not likely to affect the female body. Very often they are prescribed not only to prevent unwanted pregnancy, but also to treat gynecological diseases: amenorrhea, fibroids, dysfunctional uterine bleeding, endometriosis and others.
But in some cases, long-term use of contraceptive pills leads to the development of multifallikuljarnosti. After cancellation of OK, this condition requires correction, since there is a risk of developing polycystosis with further transformation into scleropolycystosis.
 [4]
[4]
Risk factors
The increased number of structural elements in the female sex glands arises from the impact on the body of endogenous and exogenous factors. Let's consider the main risk factors that can provoke MFN:
- Heredity.
- Prolonged intake of oral contraceptives.
- Obesity or lack of weight.
- Stress.
- Lactation.
- Diabetes.
- Impaired synthesis of luteinizing hormone.
- Adolescence.
- Age over 35 years.
Very often multifollicularity develops because of obesity, which is encountered by 35-60% of women. The deposition of excess fat is directly associated with an increase in the concentration of triglycerides and insulin in the blood plasma. This leads to a decrease in glucose tolerance and diabetes. Another common factor of MFJ is arterial hypertension and dyslipidemia.
Pathogenesis
The mechanism of multifluculosis development to date has not been sufficiently studied. MFN arises from the action of various causes and factors. Pathogenesis is based on the violation of normal organs. Normally, each appendage produces no more than 10 antral follicles at the beginning of the cycle. Under the action of hormones, one of them turns into a dominant one, its capsule diverges and ovulation sets in.
Due to this, the ovarian reserve is consumed gradually and the possibility of becoming pregnant is preserved up to 45 years. Improper work of the adrenal cortex leads to increased production of follicles. This condition entails the development of multifollicularity, and in some cases, polycystic.
Symptoms of the multifollicular ovaries
In most cases, MPP is detected during ultrasound. But there are a number of symptoms that indicate the development of multifloculosis, consider them:
- Malfunction of the menstrual cycle.
- Drawing pains in the lower abdomen.
- Increased vegetation on the body and face.
- Acne and acne.
- Increased fatty scalp.
- Infertility.
- Change in body weight in the direction of increase.
The presence of the above symptoms in conjunction with the conclusion of ultrasound is the reason for further diagnosis. Based on the results of the studies, methods of correction or treatment will be prescribed. If symptoms are left unattended, it can lead to polycystic organ changes.
Symptoms of MFN can be either indirect or direct. The first signs are manifested by the absence of menstruation for a long period of time without the onset of pregnancy. Also, many patients note a decrease in the tonality of the voice, weight gain and the appearance of excess vegetation on the body.
A large number of structural elements leads to anovulatory cycles, which can occur up to 5 times a year. They appear due to incomplete maturation of the follicle dominant or due to the follicular cyst.
Anovular cycles are characterized by a violation of ovulation, which in turn creates problems with conception. It is the inability to become pregnant, that is, the infertility of an unknown genesis, can be the reason for the passage of ultrasound and the detection of MFN.
Read also: Multifolllicular ovaries and pregnancy
Multifollicular Ovary Syndrome
Quite common ultrasound, which is due to deficiency of luteinizing hormone and a number of other factors is the syndrome of MFN. This conclusion of an ultrasound examination is characterized by the following features:
- Ovaries slightly enlarged in size.
- Echogenicity of the uterus body is higher than the appendages.
- Multiple antral follicles with a diffuse location in the stroma.
- The dominant follicle does not have a thickened capsule.
The syndrome can cause a violation of the menstrual cycle: a prolonged absence of menstruation or a rare period. It is also possible to increase body weight, increased vegetation on the face and body. The symptoms of multifollicularity are very similar to polycystic disease, so a set of laboratory tests to determine the hormonal background is carried out to confirm the diagnosis.
Treatment of the syndrome of multifollicularity is carried out during anovulatory cycles. The main goal of therapy is the normalization of the hormonal background and the restoration of reproductive functions.
According to the research, multifollicularity is more often observed in the right appendage. While the lesion of the left branch is diagnosed less often. At the same time, the most unfavorable option is the simultaneous increase of structural elements in both organs.
In most cases, the pathological condition is associated with impaired functioning of the endocrine system. MFN occurs with hormonal failures, as well as with prolonged intake of oral contraceptives, which block the natural formation of follicles.
Often, there are no significant signs of abnormality. But irregularities in the menstrual cycle, inability to conceive, weight gain and excess vegetation on the body allow one to suspect the problem. Absence of ovulation in combination with other symptoms can lead to the transition of multifollicularity to polycystosis as any of the ovaries, and either or both.
Delay of menstruation, no monthly
One of the main signs of MFIA is a violation of the menstrual cycle. Delay of menstruation and multifollicularity are interrelated concepts. Monthly become irregular, there are long delays.
In this case, the cycle can remain normal, but stretch for a long time. In some cases, the cycle lasts from 2-3 months to six months. Against this background, there is a problem of conception, because the follicles do not ripen and are not ready for fertilization. To restore menstruation and the process of ovulation hormonal drugs are used that stimulate the normal production of female sex hormones.
Difficulty with multifollicular ovaries
The effect of MPL on menstrual discharge is due to the hormonal nature of this condition. The cycle goes astray, the allocation becomes meager and painful. If the daub with diagnosed multifallicular changes appears in the middle of the cycle, this can be caused by both ovulation and more serious problems:
- Stress and emotional experiences.
- The presence of an intrauterine device.
- Reception of hormonal contraceptives.
- Diseases of the thyroid gland.
- Fibromatous nodes.
- Inflammatory processes in the uterus and cervix.
- Injuries of the vagina.
To establish the true cause of bloody discharge, a laboratory study is performed on the level of hormones and ultrasound organs that affect the functioning of the reproductive system. Based on the results of the analyzes, corrective treatment is selected, aimed at the resumption of normal discharge during menstruation.
Pain in the lower abdomen with multifollicular ovaries
The appearance of painful sensations in the lower abdomen with MPJ is most often due to increased production of prostaglandins. Similar symptoms occur when the pelvic organs are squeezed with enlarged appendages, but in this case, polycystosis is diagnosed. Most often, the discomfort is caused by the ovary in which the egg is ripe.
- Pain in the abdomen is explained by the process of maturation of the egg. The walls of the maturing follicles are stretched and discomfort arises. In the case of multi-follicularity, several dominant structural elements are observed simultaneously.
- Painful sensations can be felt by the rupture of the vessels located at the base of the ruptured follicle. The follicular fluid enters the uterine epithelium and abdominal wall, causing tissue irritation and discomfort. In this case, in addition to pain, minor spotting appears.
Discomfort lasts from a couple of minutes to 1-2 days. In addition to pain increases libido, the consistency and viscosity of mucus from the vulva varies.
But do not exclude the option, when unpleasant feelings are associated with the development of gynecological disease or inflammatory process. Aching right pain in combination with fever may be a sign of appendicitis. Such a symptomatology is characteristic of a commissural disease in a small pelvis. In any case, pain is the reason for examination and consultation with a gynecologist.
Multifollicular polycystic ovaries
If the number of follicles in the ovaries exceeds the norm, then this indicates their multifallikulyarnost. These changes can be determined by ultrasound. MFN is diagnosed in healthy women in the first week of the menstrual cycle. But if the changes are preserved in other periods of the cycle, this is the reason for a comprehensive survey and correction.
Despite the fact that the FPJ detect at each 4-6 ultrasound, polycystosis is diagnosed in 4% of women. Multifollicular polycystic or Stein-Leventhal syndrome is a rare disease that arises from the action of such factors:
- Excess body weight.
- Genetic predisposition.
- Complications of infectious and inflammatory processes.
- Long emotional experiences, stress.
- Hormonal disbalance.
- Increased production of androgens.
- Pathologies of the brain.
- Resistance to insulin.
The disease occurs with a decrease in the level of female estrogen hormones and an increase in testosterone. The concentration of insulin increases and the ratio of luteinizing and follicle-stimulating hormone changes from 1.5-2 to 2.5-3. The main signs of polycystosis include:
- Violated menstrual cycle.
- Secondary amenorrhea.
- Obesity.
- Hirsutism.
- Acne and pimples.
- Reduced voice timbre.
- Infertility.
- Frequent pain in the lower abdomen.
- Greasy oily scalp and face.
Polycystic changes are divided into primary and secondary. Primary does not cause insulin jumps and develops in patients with normal body weight. This form is characterized by severe course and poorly treatable. Secondary disorders are more often diagnosed in women with excessive body weight. In this case, the disease develops due to the extinction of the organ function during the menopause. Treatment of the secondary form does not cause difficulties.
In addition to affecting the ovaries, polycystosis can develop in other organs. For example, polycystic kidney disease refers to genetic diseases. And when the polycystosis of the uterus is diagnosed, it is a cystic lesion of the cervix of the organ. The main danger of the disease is that it significantly increases the risk of developing pathologies from the cardiovascular system and diabetes.
Multifollicular cysts of the ovaries
Tumor benign tumors, usually of a one-sided nature, forming inside the ovary are multifollicular cysts. This pathology refers to functional cysts and arises as a result of physiological processes in the organ. The cyst is a follicle in which a cell with a liquid ripens during the ovulation period.
The main causes of follicular cysts are:
- Congestive congestion of the pelvic organs.
- Inflammatory processes in the appendages of the uterus.
- Infectious diseases.
- Abortion and gynecological interventions.
- STDs.
- Hormonal disorders.
- Hyperstimulation of ovulation with infertility.
- Stress and increased physical activity.
- Childbirth.
If the size of the follicular cyst does not exceed 5 cm in diameter, then as a rule this does not cause clinical symptoms. But against this background, there may be irregularities in the menstrual cycle due to an increase in the level of estrogen in the bloodstream. In this case, women complain of a delay in menstruation, smearing discharge between menstruation and painful sensations in the second phase of the cycle. Also, the appearance of such symptoms:
- Increase in basal body temperature.
- Feeling of bursting and heaviness in the lower abdomen.
- Painful sensations in the second phase of the cycle, which increase with physical activity.
- General weakness and malaise.
Treatment consists of laparoscopy, that is, surgical intervention to remove neoplasms and a course of drug therapy. If you leave multifollicular cysts without treatment, then it is dangerous for such complications: rupture of the cyst, partial or complete torsion of the ovary, organ rupture.
Hypoplasia of the uterus and multifollicular ovaries
Underdevelopment of the uterus with a decrease in its size in comparison with the age-related physiological norm is hypoplasia. This condition arises from the inadequate production of female sex hormones. As a result of hormonal imbalance, the organ has a long conical neck, a small and hyperanteflex body.
In most cases, hypoplasia is hereditary, but it can develop because of the action of such factors:
- Ovarian insufficiency.
- Increased gonadotropic activity of the pituitary gland.
- Hypovitaminosis.
- Intoxication.
- Nervous disorders and increased physical activity.
- Frequent infectious and inflammatory diseases.
With regard to clinical symptoms, there is later onset of menstruation, irregular cycle with increased morbidity, decreased libido, multifollicularity, miscarriages, anomalies of labor. MFN in this case are caused by hormonal disorders.
Treatment consists of substitution or stimulating hormone therapy. This allows you to achieve an increase in the size of the organ, restore the normal menstrual cycle and reproductive functions.
Hyperplasia of the endometrium and multifollicular ovaries
The formation of an excessive amount of structural elements of the tissue is hyperplasia. Thickening and proliferation of the mucous membrane of the uterus is a hyperplasia of the endometrium. It has several varieties, which differ from each other by histological indices, that is, the structure of the areas of thickening.
Hyperplasia of the endometrium and MPJ can occur due to hormonal disorders, that is, with increased estrogen production and progesterone deficiency. Often, this condition is diagnosed in patients with diabetes mellitus, excessive body weight, arterial hypertension, chronic inflammatory processes of the reproductive system.
Symptoms of the disease:
- Anovulatory uterine bleeding.
- Bloody discharge between menstruation.
- Delay of menstruation.
- Increased weakness and fatigue.
- Anemia.
- Headaches and fainting.
- Decreased appetite.
The danger of a painful condition is that it can lead to infertility and malignant degeneration of uterine tissues. For the treatment of endometrial hyperplasia in combination with the syndrome of multifallikulyarnosti apply both medicamental and surgical techniques. In the first case, the patient is prescribed hormone therapy. As a surgical treatment, ablation is carried out, that is, removal of the endometrial layer. Particular attention is paid to prevention, which consists of normalizing body weight, minimizing stress and timely treatment of any infectious and inflammatory diseases.
Multifollicular ovaries and ovulation
Insufficient development of the anterior lobe of the pituitary gland of luteinizing hormone is one of the reasons for the development of MFN. The hormone is released in the second half of the menstrual cycle and is responsible for stimulating the ovulation process.
The lowered level of luteinizing hormone can be caused by sudden changes in weight, prolonged intake of hormonal drugs, endocrine diseases and a number of other reasons. Deficiency of the hormone leads to the fact that the follicles can not ripen or vice versa, several dominant ones appear simultaneously.
Multifollicular ovaries and ovulation are interrelated. If several follicles are maturing simultaneously, this entails an increased production of estrogen. Because of this, the menstrual cycle is delayed. If ovulation does not occur during ovulation, it causes anovulatory menstruation, which is dangerous for infertility.
Complications and consequences
Multifollicular ovaries, caused by hormonal disorders or more serious causes, require treatment. If you leave the MFIA without attention and medical care, it will only aggravate the painful symptoms, will cause a number of consequences and complications:
- Inability to conceive a child.
- Exchange disorders in the body.
- Persistent increase in blood pressure.
- Disturbance of blood supply to the heart muscle.
- Cancer of the uterus due to atypical cells that form on the endometrial mucosa with prolonged impairment of the functions of the appendages.
- Spontaneous termination of pregnancy.
- Hyperglycaemia.
To reduce the risk of these complications, it is necessary to regularly undergo gynecological examinations and begin treatment at the first signs of MFN.
What are the risk of multifollicular ovaries?
The main danger of MPL is that they cause a malfunction of menstruation, which in turn leads to anovulatory cycles. Because of this, there is a risk of developing such problems:
- Infertility.
- Anovulatory dysfunctional uterine bleeding.
- Anemia.
- Dysfunction of the ovaries.
In order to prevent possible dangers, all medical appointments must be observed during the period of correction of MFN. Hormonal therapy in conjunction with fortifying methods can restore the normal operation of the female sex glands and reproductive function.
Diagnostics of the multifollicular ovaries
MFJ requires medical supervision, especially if accompanied by pathological symptoms. Diagnosis of this syndrome is carried out using a set of different techniques. But special attention is paid to ultrasound research, which confirms the change in the number of structural elements of the organ.
For diagnostics use such methods:
- Ultrasonic diagnosis of ovaries.
- Magnetic resonance imaging of pelvic organs.
- MRI of the brain.
- Dopplerography.
- Blood test for hormones.
- Determination of the presence of ovulation.
Particular attention is paid to anamnesis. The doctor asks the patient about the features of the menstrual cycle, its regularity and the nature of the secretions. Also taken into account unsuccessful attempts to become pregnant, the presence of endocrine disorders, hormonal abnormalities.
The main goal of diagnosis of multifollicular ovaries is to distinguish them from a more serious disease - polycystic syndrome. Based on the results of the studies, the doctor makes a treatment plan, that is, a method for correcting the existing disorders.
Analyzes
An obligatory component of diagnosis in case of suspicion of MFN is laboratory tests. Analyzes are needed to assess the general condition of the body and the level of hormones, the violation of which can cause painful symptoms.
For detection of MFN and polycystosis, a laboratory determination of the concentration of such hormones is carried out:
- Androgen DHEA-S - produced by the adrenal glands, is detected with hirsutism, reproductive disorders, alopecia, multifollicularity and PCOS.
- Free testosterone - if its value is more than 1%, then the symptoms of hyperandrogenism occur.
- Estradiol is an active estrogen, values above or below the norm indicate certain disorders in the body.
- Cortisol - if its level is more than 20 or less than 9 mg / dl, this indicates a severe stressful condition, which may be the cause of the MFN.
- FSH and LH - reveal abnormalities in the pituitary gland. FSH stimulates the epididymis and prepares the follicles for ovulation. If the ratio of these hormones is increased, that is, a violation of the pituitary and reproductive system.
- Prolactin is produced by the pituitary gland, its elevated level can indicate neoplasms in the organ that activate excessive production of hormones. High prolactin inhibits FSH and the possibility of fertilization. Also, values above the norm arise with tumors of the hypothalamus, pituitary, Cushing syndrome.
In addition to the above studies, it is necessary to pass tests for hormones of the thyroid gland. Violations of the functions of this organ is manifested by an irregular menstrual cycle, the absence of ovulation. Another mandatory analysis is the evaluation of glucose metabolism, that is, the determination of blood sugar level, a test for glucose tolerance, insulin.
Laboratory diagnosis is carried out in certain phases of the menstrual cycle: at the beginning, with ovulation, at the end. The results obtained are compared and analyzed, which allows the final diagnosis to be made.
Instrumental diagnostics
One of the most important methods for detecting an increased number of structural components of the ovary is ultrasound. Instrumental diagnostics determines the echoscopic signs of changes, the number of follicles and other features of the pelvic organs.
Ultrasound examination is necessary for examination of the thyroid gland and adrenal glands. Visible changes in these organs can cause hormonal disorders that have caused multifollicularity.
Magnetic resonance imaging of the brain, in particular the hypothalamus, is also performed. This endocrine organ regulates metabolic processes, is responsible for reproductive and hormone-forming function. MRI reveals any changes in the structure of the pituitary and hypothalamus.
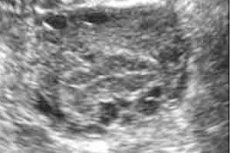
Uzi, echovirus signs of multifollicular ovaries
Symptoms of MFN can be either direct or indirect. To confirm the syndrome of multifollicularity, ultrasound is performed.
The main echolineses of MFJ for transvaginal ultrasound:
- Ovaries slightly enlarged in size or within normal range.
- Echogenicity of the uterus body is higher than the appendages.
- In the sexual glands there are multiple antral follicles 12 or more, about 9 mm in diameter.
- There is one or more dominant follicles.
- The dominant has no thickened capsule.
- Antral follicles differ diffuse (scattered) location in the stroma.
In addition to ultrasound, folliculometry can be performed to determine the presence of ovulation, if it has not been for several cycles.
Multifollicular echostructure of the ovaries
Normally, in patients of childbearing age, the size of the ovaries is 15 mm in thickness, 30 mm in length and about 25 mm in width. With MFN, these parameters are slightly increased. Also, the appendages contain structural components:
- Capsules of small parameters not more than 7-9.
- Dominant follicle.
- Yellow body.
With multifallikulyarnosti observed more than 12 antral follicles not more than 9 mm with a high probability of ripening. The dominant follicle does not have a thickened capsule, in some cases several dominant forms are formed.
Another feature of the syndrome is the diffuse arrangement of antral capsules. With MFN, the organ's echostructure is smaller than that of the uterus. Normally, the ehostruktura is homogeneous, minor fragments of fibrosis in the capsule are possible.
Differential diagnosis
If there is a suspicion of MFN syndrome, a complex of laboratory and instrumental studies is carried out. Particular attention is paid to differential diagnosis. Multifollicularity is compared with diseases in which menstrual disorders, infertility, hyperandrogenia, hirsutism and other symptoms are observed.
Differentiation of MFN is carried out with such pathologies:
- Adrenogenital syndrome.
- Tumors of the adrenal and ovaries.
- Syndrome Itenko-Cushing (hypercorticism).
- Tumor lesions of the pituitary gland.
- Diseases of the thyroid gland.
- Endocrine disorders.
For diagnosis, both laboratory and instrumental methods are used. Particular attention is paid to the results of the analysis for hormones and ultrasound.
The difference between polycystic and multifollicular ovaries
Two similar on the symptoms and the nature of the origin of the disease are polycystosis and MFN. An increased number of follicles is detected on every fourth ultrasound, but polycystosis is diagnosed only in 30% of such patients. Polycystic is a pathology of the structure and function of the ovaries. In contrast to the MFN, it proceeds with chronic anovulation (with the MPL anovulatory cycle) and hyperandrogenism. Moreover, multifollicularity can be one of the causes of PCOS development.
Consider the main differences between PCOS and MFIA:
- Echogenicity - the density of appendages with MPJ does not exceed the echogenicity of the uterus. With polycystic organ tissue is much denser than the uterine tissue.
- The size of the ovaries - with multifollicularity, their volume is slightly higher than normal. With PCOS length is more than 40 mm, with a norm of 34-37 mm.
- Follicles - in both syndromes multiple structural elements are observed. With MFN, their diameter is not more than 9 mm, and in PCOS they significantly exceed the norm. The follicle capsule under polycystosis is strongly thickened, which prevents the egg from coming out and provoking the growth of follicular cysts.
- Localization of follicles - with MPL antral follicles scattered throughout the ovary, with polycystosis they are located in the shape of a necklace, that is, on the periphery.
- DHEA and 17-OH progesterone hormones are produced by the adrenal glands, with MPF within normal limits, and with PCOS their values are increased.
When the final diagnosis is made, the results of MPJ differentiation with polycystic disease and the risk of multifollicularity transformation into PCOS are taken into account. Correctly designed treatment regimen allows you to restore reproductive functions with minimal consequences for the body.
Treatment of the multifollicular ovaries
From the results of the diagnosis, causes and symptoms depend on the methods of treatment of multifollicular ovaries. It is impossible to completely cure multifollicularity. But with the help of hormonal correction, diet therapy and vitamin therapy, it is quite possible to restore a stable menstrual cycle, the ability to ovulate and a childbearing function.
Prevention
The female organism, and especially the reproductive system, is very sensitive to any changes. Therefore, prevention of multifollicular ovaries reduces to such rules:
- Regular preventive examinations at the gynecologist.
- Control of body weight to prevent hormonal imbalance.
- Balanced diet.
- Moderate, but regular physical activity.
- Timely treatment of any diseases.
- Minimizing stressful situations and emotional shocks.
- Reception of any drugs, especially hormonal contraceptives only for medical purposes.
If MFN is a variant of the norm and do not harm the reproductive system, regular ultrasound is recommended to prevent any complications in order to detect changes in time.
Forecast
Multifolllicular ovaries are diagnosed in many women. Their appearance can be associated with age characteristics and act as a norm or indicate certain disorders in the body.
The prognosis of MFN syndrome depends on its cause, the patient's age and symptoms. In 90% of cases, after a complex correction, the woman regains ovulation and the ability to conceive. At the same time there is a risk of miscarriage at an early age, multiple pregnancy and gestational diabetes.

