Cocci in the smear: treatment
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In modern medicine, there is a growing need for smears and bacteriological studies. This is due to the fact that the proportion of diseases of bacterial etiology increases dramatically. But often, even when determining the species composition and the amount of microflora, this is not enough to diagnose and select treatment. Difficulties arise in connection with the fact that along with the pathogenic flora, in the human body there is also a normal microflora that provides protection of the organism. One example is cocci in the smear, which are found in the analysis of each healthy person.
Cocci in a Smear in Women
Vaginal microbiocenosis is very important for a woman's health. It contains approximately 10% of the microflora of the whole body of a woman and plays a leading role in maintaining health. Its importance lies in the fact that it determines the health not only of a woman, but also of a newborn child. Violation of the normal vaginal microflora entails not only an increase in gynecological diseases, but also the growth of neonatal and pediatric morbidity and mortality.
The basis of microflora women form anaerobic microorganisms. These are mainly lactobacilli, bifidobacteria and propionebacteria. Also in this group are eubacteria, clostridia, bacteroides, peptococci. All together, they form an obligate microflora, which provides reliable protection of the urogenital tract of a woman from the introduction of pathogenic microflora (provide colonization resistance of the mucous membrane).
In addition to obligate microflora, there is also an indigenous, or facultative microflora, which is represented by conditionally pathogenic forms of microorganisms. Quite a large percentage here is given to cocci. Prevalent streptococci, staphylococci, enterococci, aerococci and other microorganisms. This means that under normal physiological condition of the body, their number is insignificant, and does not exceed 3-4%. This flora, along with the obligate one, provides reliable protection against pathogens, stimulates the immune system. But with a decrease in immunity and the development of the inflammatory process, as well as a decrease in the activity of the obligate flora, the opportunistic flora begins to grow actively, filling all the free space of the mucous membrane and the integument. In this case, they act as causative agents of infectious diseases.
Diseases are determined by which microorganism began to prevail sharply and quantitatively exceeded the norm values. With the predominance of cocci, severe infectious and inflammatory diseases of the internal organs begin to develop: bacterial vaginosis, infections of the genitourinary system, pyelonephritis, salpingitis, and chorioamnionitis.
Kokki causes postoperative complications, postpartum fever, and other complications, neonatal infections, sepsis, peritonitis. Kokki is one of the most dangerous forms of nosocomial infection, which can not be treated, and has an extremely high degree of resistance to drugs and disinfectants.
The composition of the microflora is relatively constant, evolved. But under the influence of various factors, changes can occur in it. The composition and quantity of microflora can be influenced by anatomical structure, hormonal background features, specificity of blood circulation and lymph circulation. As a result of taking certain medications, including antibiotics, serious changes can occur.
The formation of the microbiocenosis of a woman begins with the moment of birth. Already during the first day of life, the sterile initial vagina is colonized by the maternal microflora. That is why it is so important for a woman to maintain health and a normal microecological state of the reproductive organs. Formed mainly flora, which is dominated by lactobacilli and bifidobacteria. Then the amount of these microorganisms decreases, and before the period of puberty is in equilibrium with other microorganisms, or the coccoid forms of bacteria begin to actively multiply and predominate. This significantly increases the risk of contracting urogenital infections by household use.
After the girl reaches puberty, there is a surge in estrogen activity, resulting in an increase in the epithelial layer and the amount of glycogen. From this moment the lactate flora again takes the leading position, which ensures colonization resistance and protection of the woman's organism from pathogens.
With violations in the body, dysbacteriosis develops, in which the opportunistic flora begins to predominate over the obligate flora, which causes the development of infectious diseases and inflammatory processes. Especially negative conditions and a high risk of dysbiosis develop during the period of menstruation, when there is a change in the hormonal background, the amount of glycogen decreases sharply and accordingly, optimal conditions for the development of opportunistic microflora and suppression of the obligate one are formed. The microflora also changes during pregnancy, during the postmenopause, because the body undergoes intensive hormonal changes.
Cocci in a smear during pregnancy
In an organism of the pregnant woman optimum conditions for development of obligate microflora develop. This is due to an active "estrogen explosion", which contributes to the development of microorganisms of the group of lactobacilli and bifidobacteria. It is interesting that the normalization of microflora occurs not only in the vaginal biotope, but in all others, especially in the intestines, mouth, skin. It is for this reason that a healthy woman during pregnancy improves hair structure, skin condition, nails. Maintaining the optimal microflora is necessary in order to protect the child, preventing the development of intrauterine infections, as well as infection when passing through the birth canal. The interruption of pregnancy sharply reduces the colonization resistance of the mucous membrane, so the pathogenic microflora is actively developing. This leads to the development of infectious and inflammatory processes.
The protective properties and colonization resistance of microflora during childbirth, as well as in the early postpartum period, sharply decrease. At this time, the protective properties are minimal, so the woman is most at risk of infection. Especially dangerous during this period are hospital strains of microorganisms that quickly infect the weakened organism, cause severe pathologies, and practically can not be treated with antibiotics, antibacterial drugs. Very often leads to bacteremia, sepsis, can even have a lethal outcome. Restoration of normal microflora occurs by the end of 5-6 weeks of the postpartum period.
Cocci in a smear in men
Men normally have propionic acid bacteria and bifidobacteria, which form an obligate microflora. It provides colonization resistance of mucous membranes and prevents the development of pathogenic flora. Also in the body there is an indigenous microflora, which is represented by conditionally pathogenic forms. They can be activated and colonize the mucosa with reduced immunity and insufficient activity of the obligate microflora.
Indigenous microflora is represented mainly by coccoid forms. Among them are streptococci, staphylococci, enterococci. Normally, the indices should not exceed 10 3 cfu / ml. If the amount of indigenous microflora goes beyond this indicator, a bacterial infection that depends on the type of microorganism can develop. Kokkovye forms can provoke various infectious, inflammatory, purulent-septic infections, and even sepsis, which often results in death.
 [12],
[12],
Kokki in a Smear in a Child
Cocci in a smear in fairly large quantities can be found in various biotopes of the newborn, and this is the norm. This is due to the fact that in the first day of life in the child all the cavity organs remain relatively open. In all of them, including in the large and small intestine, contains a high amount of oxygen. This forms optimal conditions for the accumulation of aerobic microflora. This is facilitated by the immaturity of the immune system. It must be remembered that aerobic flora is conditionally pathogenic, which means that at this time the child is at maximum risk of developing pathogenic microflora, which can lead to an infection process and sepsis.
The first 7-10 days after birth can be characterized as a period of transient dysbiosis, in which there is an active development of aerobic microflora, as well as intensive colonization of skin and mucous membranes. At this time, and protective mechanisms are formed, which are strengthened by the mother's milk. Gradually, more favorable conditions for the development of anaerobic flora are formed.
Gradually begins to form an anaerobic microflora. This leads to a reduction in its oxidation-reduction potential. The end of the first week of life markedly increases the acidity of gastric juice, increases the synthesis of their own antibodies and immune complexes. Later, epiapithelial biofilms are formed, which are the main reservoir of human autoflora. The duration of the formation of epiepithelial biofilms is not exactly established. This process is slow, and depends on many factors, first of all - the health of the mother, the quality of her breast milk, the ecology of the external environment.
It is known that in a newborn the predominance in the colon of a physiological microflora, primarily bifidobacteria, begins to be noted until the end of the early neonatal period, that is, approximately 7 days after birth. But at the present time rather high concentrations of concomitant microflora are registered for several months and even 2-3 years of the child's life.
In parallel with the formation of the intestinal microflora, the microflora of the epithelium, the skin, is also formed. The trigger mechanism for its formation is application to the breast in the early period. First of all the child receives lactobacilli. Their populations quickly form a biotope, gradually reducing the amount of oxygen. These conditions are more suitable for bifidobacteria and propionic acid bacteria, which begin to grow. This is the second layer of microflora.
It is followed by a third layer, which is formed by lactobacilli. They stimulate the receptors of the cell walls, activate the epithelial microflora, resulting in the formation of a matrix of a biological structure that contains mucin and other active enzymes, exopolysaccharides. Optimal conditions for symbiont microflora are formed.
In the composition of the microflora of a healthy child, the level of conditionally pathogenic forms, which are represented mainly by cocci forms, does not exceed 5%. Inclusion of a small number of pathogens in the microbiota of the child is inevitable, due to their high content in the environment. But the physiological flora dominates, which does not allow the development of pathology.
Consequences and complications
The prevalence of cocci in the smear leads to the development of the infectious process. There are various diseases of internal organs, skin, inflammatory, purulent-infectious processes. The most dangerous conditions are peritonitis, bacteremia, sepsis, which are life-threatening conditions and can result in death.
A serious consequence is various postoperative complications, postpartum infections, neonatal infection, catheter-associated infections, wound infection. Especially dangerous are hospital strains of cocci, which have acquired multiple resistance, and practically do not lend themselves to treatment.
What are the dangerous cocci in the smear?
Normally, cocci are always found in the smear, because they are representatives of normal human microflora. If the indicators do not exceed the norm, cocci do not pose a danger, on the contrary, they perform a protective function in the body, preventing infection by other, pathogenic microorganisms. The danger arises when their number exceeds the norm - it becomes more than 103 cfu / ml. In this case, there are various infectious, purulent, inflammatory diseases.
The most dangerous complication of cocaine infection is sepsis, in which infection from the hearth penetrates into the blood, and with the blood flow spreads throughout the body, infecting other organs, forming new foci. Sepsis requires urgent measures, immediate antibiotic therapy, otherwise a fatal outcome is possible.
No less dangerous are such conditions as bacteremia, septicemia, in which there is an insignificant and moderate amount of cocci in the blood and other normally sterile liquids. The danger is that at this stage the disease progresses very quickly and within a few hours can go into sepsis and end with a fatal outcome.
Are the cocci transferred to a partner?
If one of the partners has a high content of cocci and an active inflammatory process, the pathogenic microflora can be transmitted to the partner. Whether the disease will develop, or not, depends on the state of immunity and overall endurance of the organism. If immunity is normal, the general condition of the body is satisfactory, most likely there will be no disease. This is due to the fact that the partner's own microflora possesses a sufficiently high colonization resistance, which will not allow the alien microflora to penetrate into the biotope.
If the immunity is lowered, the body is weakened, a bacterial infection may develop, because the protective activity and colonization resistance of its own microflora are at a very low level. This will allow the alien microflora to penetrate into the biotope, resulting in the appearance of symptoms of the disease.
Differential diagnostics
It implies the need to clearly differentiate the pathogen: to prove that the cause of the disease is precisely the high concentration of cocci. For this, a routine smear or a complete bacteriological study is performed.
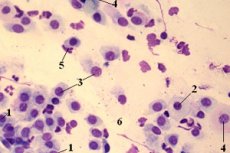
This will require biological material from the biotope under study. So, with diseases of the respiratory tract usually take a swab from the nose and throat, with urogenital infections - a swab of the vagina or urethra, etc. Then a smear is applied to the slide, dried over the tribe of the burner, or fixed by chemical methods and examined by microscopy.
If necessary, additional staining is carried out, which allows the different structures to be clearly differentiated. For the detection of cocci, the Gramm coloring technique is most often used. In this case, the cocci acquire a bright violet color and are clearly visible in the field of vision under a microscope. You can study their morphology, the main characteristics.
Often, in order to obtain more detailed information on the culture isolated during the microscopy, bacteriological culture is produced. To do this, the resulting culture is sown on an artificial nutrient medium, incubated under optimal conditions for 3-5 days. After this, the culture is removed, done by re-settling to isolate the pure culture (pathogen), again incubated. Then, the grown colonies are analyzed, qualitative and quantitative analysis is carried out. With the help of a number of biochemical and immunological techniques, the culture is identified using the Berdi determinant. The cell concentration in 1 milliliter of the slurry is then determined using any convenient method. The most commonly used method is serial dilution, or a turbidity standard.
If the smear is good, can there be an infection?
Any good smear always contains the entire set of microorganisms that are characteristic of this biotope. The quantity should correspond to the norm. That is, the results of the analysis will list the representatives of normal microflora and their number. A good smear means that the obligate microflora prevails over the opportunistic pathogen, and any other microorganisms are absent.
Single microorganisms are admitted as representatives of a transitory (accidentally introduced) microflora. This means that there is no infection, as colonization resistance and immune mechanisms are at a sufficiently high level in order to withstand the infection.
Treatment
If cocci is found in the smear, in the redistribution of the norm - no treatment is required. If their number significantly exceeds the norm, antibiotic therapy may be required. Also apply homeopathic, folk remedies, herbal medicine. When choosing a method of treatment, one should consult a doctor and rely on the results of the analysis. With a moderate number of cocci and expressed dysbiosis, the use of probiotics or prebiotics is advisable.
Medications
When treating cocci, you need to follow the basic precautionary measure - to begin treatment only after a preliminary consultation with a doctor. The doctor is also insured - he should prescribe the treatment only on the basis of the results of the tests.
If antibiotic therapy is expected, it is advisable to perform an antibiotic sensitivity test and use it to select the most effective drug and its optimal dosage. The consequences and side effects of improper intake of medications can be deplorable - aggravation of the situation, development of serious dysbiosis with affecting of deep microbiocenoses, development of bacterial infection. It is better to start treatment with probiotics, which act gently, normalizing the microecological state of the body.
For the treatment and prevention of intestinal dysbacteriosis, coccal infection, it is recommended to take bifilact-extra 1 capsule per day. The capsule contains bifidobacteria and lactobacilli, as well as auxiliary substances.
In intestinal infections, diarrhea, meteorisms, as well as in the complex therapy for the treatment of acute inflammatory and allergic diseases, bifi-forms are used, 1 capsule each.
For the treatment and prevention of vaginal dysbacteriosis and other diseases of the female genitourinary system, apply bifolac in the form of suppositories. Apply for the night, intravaginally 1 suppository.
Ointment emulate is used externally for various skin diseases. Contains a stabilized culture of lactobacilli. It is used for dermatitis, any other skin diseases, dysbiosis. Apply a thin layer to clean skin.
Antibiotics from cocci in the smear
Antibiotics are widely used to treat cocci, especially if their concentration is high enough. For today, ciprofloxacin has proved to be well - 500 mg once a day for three days. Quickly removes all symptoms of bacterial infection, normalizes the level of cocci. Similarly, other antibiotics also work: amoksiklav, amoxicillin, azithromycin, azitrok, penicillin.
The Indian company offers a new drug that combines an antibiotic and a probiotic. The antibiotic kills the pathogenic microflora, the probiotic immediately restores the normal flora, which is also damaged. The composition includes 250 mg of amoxicillin and cloxacilin, as well as 60 million microbial bodies of lactobacilli. Take any diseases of bacterial etiology of any localization.
Candles from cocci in a smear
If the pathology is not systemic, that is, does not affect the entire body, taking antibiotics orally is not recommended. It is better to use suppositories (suppositories). They allow to quickly and effectively eliminate pathology locally. The risk of side effects and overdose is minimized. Candles should appoint only a doctor. Depending on the pathology, apply rectally, or intravaginally. Usually the course of treatment is from 3 to 14 days. Apply more often antibiotics or probiotics.
 [26], [27], [28], [29], [30], [31]
[26], [27], [28], [29], [30], [31]
Folk treatment
For the treatment of coccal infection among the people, aloe juice was widely used. For this, you need to take 2-3 juicy fleshy leaflets, squeeze out the juice, and apply either orally, depending on the localization of the pathology. Inside take in its pure form, 1 tablespoon, or diluted in a glass of warm water.
Also at all times, the infection was taken with honey. It has an antiseptic effect. In diseases of the respiratory tract, honey is added to tea, or to vegetable decoctions, from honey make compresses, lotions. It is used for massages and wraps. To eliminate the infection will help the use of honey in its pure form, on a tablespoon in the morning and in the evening.
From external and internal infection the mummy helps. It must be diluted in a liter of water and drink a glass in the morning, before you get out of bed. After drinking, you still need to lie for 40 minutes, only after that you can get up.
Herbal Treatment
The most famous herb, which has anti-infective and anti-inflammatory effect, is chamomile. It is used in the form of a decoction or in the form of infusion. The difference is that the infusion is prepared on alcohol or vodka, it is more concentrated and saturated, contains more active components, so its dosage is required lower than for decoction. Insist infusion longer - up to 7 days, while the broth is ready for 1-2 hours. Drink the infusion on a tablespoon, while the broth - to a glass a day. Store infusion can be up to a year, broth - no more than a day.
Calendula has an antiseptic effect. Apply in the form of a decoction: a tablespoon of grass to a glass of boiling water. To insist 30 minutes, and to drink within day. The result is usually noticeable within 1-2 days.
In intestinal infections, a decoction of fennel has proved to be a good idea. To make it, you need a third of a teaspoon of seed to pour a glass of water and drink a third of the glass three times a day.
Homeopathy
It is important to observe the precautionary measures - do not take any funds from the preliminary consultation with the doctor. Homeopathic remedies have side effects only if the remedy is misused, or in case of an overdose. Usually deterioration occurs.
Vitaflor is a biologically active additive, which is represented by two strains of lactobacilli. It is used for dysbacteriosis, with a lack of lactobacilli and a predominance of cocci 1 capsule per day.
Vitasporin is a sporic probiotic, which includes a complex of bacillary forms of microorganisms. It is used for staphylococcal and other coccal infections, 1 capsule per day.
Gastrofarm is a probiotic containing the main representatives of normal intestinal microflora. It is used for infections and dysbacteriosis. Take a pill a day.
Enterol is used for acute and chronic diarrhea, enteritis. Available in bags. Take a sachet 2-3 times a day. Contains lyophilized saccharomycetes.
Prevention
The disturbance of microbiosis has serious consequences for the population. It should be borne in mind that the majority of parturient women, even in the normal course of pregnancy and childbirth, have deviations in the microbiocenosis, expressed to a greater or lesser degree. This inevitably affects the health of the newborn. Therefore, the widespread occurrence of dysbiosis among the population in recent years is most closely associated with primary microecological defects that arose during the formation of microbial ecosystems in newborns. In the body, defective biofilms and microbial associations are initially formed that are unable to perform physiological functions.
Analysis of patterns of primary formation and further functioning of microbial biocenoses of the child's organism leads to the conclusion that it is necessary to introduce and carry out special measures for the prevention of dysbacteriosis. First of all, the solution is seen in the elimination of those factors that contribute to the development of pathology. It was found that the primary disorders are primarily in the obstetric-gynecological chain. It is necessary to increase the effectiveness of therapeutic and preventive measures to prevent pathological changes in endomicroecology of pregnant women, parturient women, and puerperas.
It is also important to maintain a culture of communication between the mother and the child: timely application to the breast, breastfeeding, regular and constant contact of the mother and the child. The third place is the observance of sanitary and hygienic standards and requirements.
It is also necessary to ensure adequate correction of existing dysbiotic disorders, to apply rational therapy schemes, to use preliminary preparation of pregnant women, targeted colonization of biotopes of children at risk, to reduce the use of antibiotics, and other antibacterial drugs, if necessary, to use probiotics, prebiotics.
Forecast
If timely detection of cocci in the smear, or rather their high concentration, you can take action and prevent the development of bacterial infection. Requires a comprehensive treatment, matched by a doctor based on the results of the tests. If the increased number of cocci is ignored, the forecast may be unfavorable. A bacterial infection that tends to progress, up to sepsis with a fatal outcome, may develop.

