Intestinal amoeba in man: cyst structure, life cycle
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Intestinal amoeba is a non-pathogenic microorganism that lives in the lumen of the lower part of the thin and upper large intestine. It is a constant parasitic organism, but it can also exist outside it.
In the external environment intestinal amoeba is well preserved, in some cases it can reproduce, but still a favorable place for it is the intestine of a person or other living organism. As a food, non-living organic substrates (bacteria, the remains of various foods) are used, while the amoeba does not secrete an enzyme that breaks down proteins into amino acids. Due to this in most cases there is no penetration into the wall of the intestine, which means that the owner is not harmed. This phenomenon is called carrying. With weakening of immunity and confluence of other circumstances, amoeba penetrates the intestinal mucosa and begins to multiply intensely.
Structure of the intestinal amoeba
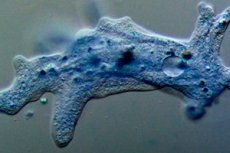
Intestinal amoeba is a type of protozoa. The structure of the intestinal amoeba consists of a body and a nucleus. In the body there is protoplasm (a liquid substance with specialized living structures) and one, two, rarely several nuclei. Protoplasm has two layers: the inner (endoplasm) and the outer (ectoplasm). The nucleus resembles a vesicle.
There are two phases of the existence of intestinal amoeba: a vegetative individual (trophozoite) and cyst. Trophozoites have a well-distinguishable core with a diameter of 20-40 μm. Amoeba constantly changes its shape due to the appearance of pseudopods, with the help of which movement and seizure of food takes place. Due to the shape of pseudopods, nuclei, their number, one or another species of amoebae is identified. Its movements are slow, like trampling on the spot. Reproduction occurs by dividing the nuclei first, then protoplasm.
Life cycle of the intestinal amoeba
The life cycle of the intestinal amoeba passes, beginning with the infection of the host organism by the fecal-oral route. With unwashed hands, vegetables, fruits, thanks to different vectors (flies, cockroaches) amoeba cysts fall into the inside of a person. Due to their shell, they are intact pass aggressive for them the environment of the stomach, duodenum, getting into the intestine. His enzymes dissolve the shell, giving way to intestinal amoeba.
The vegetative stage of development has the following forms: tissue, luminal and pre-cystic. Of these, the tissue phase is the most mobile, it is at this time that amoeba is the most invasive. The other two are inactive. Of the luminal form, part of the amoebas passes into the pre-cyst, the other is introduced into the intestinal mucosa, forming a pathogenic tissue form. As a result of its vital activity, the latter releases cytolysins, melts tissues and creates conditions for reproduction. The cyst is immovable, during defecation, it leaves the intestine. With a strong infection of up to 300 million individuals a day leaves the body.
Cysts of intestinal amoeba
After several cycles of reproduction, when unfavorable conditions for a vegetative individual come, it is covered with a shell, forming a cyst. The cysts of the intestinal amoeba have a round or oval shape, measuring 10-30 μm. Sometimes they contain a supply of nutrients. At different stages of development, cysts have a different number of nuclei: from two to eight. They come out with faeces, if they are infected in large quantities and have the ability to persist for a long time. Once again they enter the living organism, bursting into amoeba.
Symptoms
A large accumulation of intestinal amoeba, which happens in the case of a decrease in human immunity after the transferred stresses, viral infections, respiratory diseases, causes a disease that is called amoebiasis. Most often it is intestinal and extra-intestinal. Intestinal causes ulcerative lesions of the large intestine and, as a consequence, prolonged leakage. In this case, the amoeba, along with the blood, penetrates into other internal organs, more often into the liver, and damages them, causing extraintestinal abscesses.
Symptoms of amebiasis, in the first place, is a loose stool, which can be crimson. Painful sensations arise in the right upper abdomen, tk. The localization of these organisms occurs in the upper part of the large intestine. The temperature may rise, chills, jaundice.
Intestinal amoeba in children
The mechanism of infection of intestinal amoeba in children is the same as in adults, and the source is unwashed hands, flies, dirty toys and household items. Amoebiasis can occur asymptomatically, manifestly, in acute or chronic form. Asymptomatic is invisible to the child. On the manifest form indicates deterioration of health, weakness, decreased appetite. The temperature can be normal or slightly increase. Diarrhea appears, defecation occurs several times a day, learning up to 10-20 times. In fetid liquid feces appears mucus with blood. Crimson color of feces is not always. There are paroxysmal pains in the right side of the abdomen, intensifying before emptying. Without treatment, the acute stage lasts a month and a half, gradually fading. After the stage of remission flares up with renewed vigor.
Diagnostics
Diagnosis of intestinal amoeba occurs, beginning with the clarification of the patient's anamnesis: what symptoms, how long ago appeared, whether the patient stayed in countries with a hot humid climate and low sanitary culture. It is there that amoeba is widespread and it can be imported from there.
The blood, feces and urine are analyzed. Pathogens are found in feces, while it is important to identify the vegetative form of amoeba. The analysis should be done no later than 15 minutes after bowel movement. Also, amoeba can be detected in the tissues with sigmoidoscopy - a visual examination of the rectal mucosa with the help of a special device. Recto-manoscope gives the opportunity to see ulcers or fresh scars on its inner surface. Not revealing traces of lesions of the mucous does not yet indicate the absence of amoebiasis, they may be in the higher parts of the intestine. There is a blood test for the detection of antibodies to amoeba, he will confirm or refute the diagnosis.
With the help of ultrasound, fluoroscopy, tomography determine the localization of abscesses with extraintestinal amebiasis. Intestinal amebiasis is differentiated with ulcerative colitis, and amebic abscesses - with abscesses of a different nature.
The difference between intestinal amoeba and dysentery
The difference between intestinal amoeba and dysentery in its structure: the dysentery shell is a two-contour, refracting light, it has 4 nuclei (in the intestinal - 8), located eccentrically, it includes blood cells, which is not in the intestinal. Dysenteric amoeba is more vigorous in movement.
Treatment
Treatment of intestinal amoeba is carried out depending on the severity and form of the disease. The drugs used to eliminate the disease are divided into amoebicides of universal action (metronidazole, tinidazole) and direct, directed to a specific localization of the pathogen: in the lumen of the intestine (quinophone (yatren), meksaform, etc.); in the wall of the intestine, liver and other organs (emetin hydrochloride, dehydroethymine, etc.). Antibiotics of the tetracycline series are indirect amoebicides, affecting amoebae in the lumen of the intestine and in its walls.
Asymptomatic intestinal amebiasis is treated with yatren. During an acute outbreak, metronidazole or tinidazole is prescribed. In severe form, metronidazole is combined with yatrene or antibiotics of the tetracycline series, possibly adding dehydroethymethane. In the case of extraintestinal abscesses, metronidazole is treated with yatrene or hingamine with dehydro-methine. Clinical follow-up is conducted throughout the year.
Prevention of the intestinal amoeba
The best prevention of intestinal amoeba is the observance of personal hygiene - frequent washing of hands, raw vegetables and fruits under running water, not using tap water or open sources. Especially strictly these rules should be adhered to when traveling to countries with hot and humid climates.
Isolation of the sick until complete recovery is another necessary measure of prevention. If the pathogen is identified in the public catering worker, the entire room is disinfected.
Forecast
Timely detection of intestinal amoeba gives a favorable prognosis of treatment. Prolonged infection without treatment is complicated by the formation of adhesions in the intestine, perforation of amoebic ulcers, peritonitis, which is very dangerous.
After curing the disease, a second infection may not be present or the disease passes easily, since immunity is produced. In the case of the appearance of extraintestinal abscesses and their late diagnosis, a lethal outcome is possible.


 [
[