Experimental modeling of osteoarthritis in animals
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
K.R.N. Pritzker (1994) defined the experimental model of a disease in animals as "a homogeneous group of animals that have inherited, naturally acquired or experimentally induced biological processes that undergo scientific research, which in one or more parameters is similar to that in humans." Models of osteoarthrosis in animals are convenient for investigating the evolution of structural changes in articular tissues in order to determine how different risk factors initiate or contribute to the appearance of these changes, as well as to assess the therapeutic measures used. It should be remembered that osteoarthritis is a disease of not one tissue - articular cartilage, but all tissues of the affected joint, including the subchondral bone, the synovial membrane, menisci, ligaments, periarticular muscles and afferent nerves, the end of which lie both outside and inside the joint capsule. The ongoing studies of pharmacological agents on animal models focus mainly on their effect on articular cartilage. On experimental models it is impossible to evaluate the main symptom of osteoarthritis in people - joint pain. At the same time, in modeling osteoarthrosis, animals do not take into account a number of important factors contributing to the development and progression of osteoarthritis (for example, the vertical position of the human body, the weakness of periarticular muscles, etc.).
Of course, the most obvious model of the disease is the one that has the greatest similarity with changes in human osteoarthritis. The most interesting models of osteoarthrosis in animals are presented in terms of studies of the effectiveness of DMOAD (disease modifying OA drugs). Despite the fact that a number of drugs in this group prevent or slow the progression of experimentally induced or spontaneous osteoarthritis in animals, when studying their effects in humans, they all proved ineffective.
Models of osteoarthritis in animals
|
Modeling mechanism |
Animal species |
Inducing factor / agent |
A source |
|
Spontaneous osteoarthritis |
Guinea pigs |
Age / Overweight |
Bendele AM etal., 1989 |
|
Mice STR / ORT, STR / INS |
Genetic predisposition |
Das-Gupta EP et al., 1993 Dunham J. Et al., 1989 Dunham J. Et al., 1990 | |
|
Black mouse C57 |
Genetic predisposition |
OkabeT., 1989 StabescyR. Etal., 1993 TakahamaA .. 1990 van der Kraan PM etal., 1990 | |
|
Mice |
Collagen II mutation |
GarofaloS. Etal., 1991 | |
|
Mice |
Collagen IX mutation |
NakataK. Etal., 1993 | |
|
Dogs |
Hip Dysplasia |
SmaleG. Etal., 1995 | |
|
Primates |
Genetic predisposition |
Alexander CJ, 1994 Carlson CS etal., 1994 ChateauvertJ.M. Etal., 1990 | |
|
Chemically induced osteoarthritis |
Chickens |
Iodoacetate in / s * |
Kalbhen DA, 1987 |
|
Rabbits |
Papain in / s |
MarcelonG. Etal., 1976 CoulaisY. Etal., 1983 CoulaisY. Etal., 1984 | |
|
Guinea pigs |
Papain in / s |
TanakaH. Etal., 1992 | |
|
Dogs |
Chymopapain in / s |
Leipold HR et al., 1989 | |
|
Mice |
Papain in / s |
Van der Kraan PM etal., 1989 | |
|
Mice |
Collagenase in / with |
Van der Kraan PM etal., 1989 | |
|
Mice |
TGF-R w / s |
Van den Berg WB. 1995 | |
|
Rabbits |
Hypertonic NaCl solution |
VasilevV. Etal .. 1992 | |
|
Physically (surgically) induced osteoarthritis |
Dogs |
Intersection of the anterior cruciate ligament (unilateral) |
Marshall JL et al., 1971 Brandt KD, 1994 |
|
Dogs |
Intersection of the anterior cruciate ligament (bilateral) |
Marshall KW. Chan AD, 1996 | |
|
Rabbits |
Cross anterior cruciate ligament |
Christensen SB, 1983 VignonE. Etal., 1991 | |
|
Sheeps |
Meniscatectomy |
Ghosh P. Etal., 1993 | |
|
Rabbits |
Meniscatectomy |
FamA.G. Etal., 1995 Moskowitz RW, Goldberg VM, 1987 | |
|
Guinea pigs |
Meniscatectomy |
Bendele AM, 1987 | |
|
Guinea pigs |
Myoectomy |
ArseverC.L, BoleG.G., 1986 LaytonM.W. Et al., 1987 Dedrick DK et al., 1991 | |
|
Rabbits |
Contusion of the patella |
OegemaT.RJ, etal., 1993 MazieresB. Etal., 1990 | |
|
Rabbits |
Immobilization |
Langenskiold A. Et al., 1979 Videman T., 1982 | |
|
Dogs |
Immobilization |
Howell DS et al., 1992 Ratcliffe A. Et al., 1994 Palmoski M., Brandt KD, 1981 | |
|
Dogs |
Denervation with subsequent intersection of the anterior cruciate ligament |
VilenskyJA etal., 1994 |
* in / s - intraarticularly.
Physically and chemically induced models of osteoarthrosis are very popular at the present time, but they rather reflect the processes that are observed in secondary osteoarthritis in humans than in idiopathic ones. An alternative to them are models of spontaneous osteoarthritis in bipedal primates and quadruped animals.
Some authors are very skeptical about modeling osteoarthritis in animals in general. So, according to MEJ Billingham (1998), the use of models for the discovery of osteoarthritic modifying drugs is a "... Costly adventure".
Models of spontaneous osteoarthritis
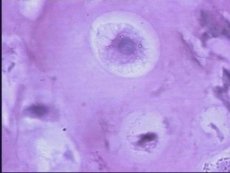
Virtually all inbred lines of mice develop osteoarthritis of varying severity and localization. The highest incidence of osteoarthritis and the most severe course of the disease is observed in STR / ORT and STR / INS mice. Among STR / ORT mice, the disease is more common, it is more severe in males than in females. The primary damage to articular cartilage develops in the medial part of the tibia plate. It was assumed that the appearance of changes in the cartilage is preceded by a patellar mixing, but RG Evans and co-authors (1994), S. Collins and co-authors (1994) found that in all mice of this line the cartilage damage develops by 11 months, but not all have a patellar bias . The same authors have found that changes in articular cartilage in STR / ORT mice are often preceded by chondrocyte-osteoblastic metaplasia of the tendon and ligament cells around the affected knee joints, which points to the primacy of these changes in the pathogenesis of osteoarthritis in this model. It is possible that the primary calcification of ligaments and tendons changes the mechanical pressure on the intraarticular structures and further changes in articular cartilage reflect an attempt to maintain a normal load on the joint. Unlike models using guinea pigs and macaque, in which cartilage degeneration is preceded by changes in the subchondral bone, in the STR / ORT and STR / INS mice, subchondral sclerosis appears later.
The advantage of this model of osteoarthritis is the small size of the animals, which requires a minimum expenditure of the test pharmacological agent. However, the size is also a drawback, since biochemical, pathohistological cartilage analysis is difficult in mice.
Research А.М. Bendele, JE Hulman (1988), A.M. Bendel et al. (1989), as well as SCR Meacock et al. (1990), devoted to the study of the natural course of spontaneous osteoarthritis in guinea pigs, have intensified interest in this model of the disease. Since the age of 13 months, all the male guinea pigs of the Dunkin Hurtley line have degeneration of the articular cartilage. Similar changes in females appear somewhat later and are of a milder character. At the age of 1 year, a complete loss of articular cartilage is observed in the medial condyle of the femur and the plate of the tibia. The increase in the body weight of the Dunkin Hurtley marine pigs aggravates the course of the disease, and a decrease in body weight of up to 900 g and less improves the course of osteoarthritis. At the age of 8 weeks, changes in the subchondral bone are already observed in this model, i.e. The latter precede cartilage damage. Changes in the cruciate ligaments of the knee joints can accelerate the remodeling of bone tissue.
Spontaneous osteoarthritis develops in rhesus and cynomolgus monkeys. A very important advantage of primates over other animals used to create an experimental model of osteoarthritis is biped. The disease develops in individuals of middle / old age. Early histological findings are a thickening of the subchondral bone, followed by fragmentation of the articular cartilage in the medial plate of the bollylebic bone. Later, the lateral plate is involved in the process. It is noteworthy that degeneration of articular cartilage begins to develop only after the thickness of the subchondral bone reaches 400 μm. The increase in prevalence and severity of osteoarthritis in macaques occurs with age, but these parameters are not affected by sex and body weight. Until now, models of osteoarthritis in primates have not been used to study the effectiveness of DMOADs.
Models of physically (surgically) induced osteoarthritis
Models of osteoarthritis, based on surgically induced loosening of the knee joints, changing the mechanical pressure on them, are most often used in dogs and rabbits. The most widely used model is the intersection of cruciate ligament in dogs. When creating surgical models of osteoarthritis, rabbits use operations to cross the cruciate ligament with excision of the medial and collateral ligaments or without it, total or partial meniscactomy, surgical rupture of menisci. Guinea pigs describe surgical models of osteoarthritis, created by crossing the cruciate and collateral ligaments, partial meniscectomy. Partial meniscactomy in guinea pigs leads to the formation of osteophytes for 2 weeks and excessive degeneration of articular cartilage for 6 weeks.
Until recently, the model of osteoarthritis in dogs that developed after crossing the anterior cruciate ligament was skeptical in view of the lack of cartilage ulceration and the marked progression of the disease observed in human osteoarthritis. JL Marshall and S. - E. Olsson (1971) found that changes in the tissues of the knee joints in dogs were practically the same as those recorded immediately after 2 years after the operation. The authors suggested that mechanical factors (for example, articular capsule fibrosis and osteophyte formation) stabilize the knee joint loose after surgery and prevent further progression of the destruction of the articular cartilage. It was also suggested that this model be considered a model of cartilage damage and repair, and not a model of osteoarthritis. However, the results of studies conducted by KD Brandt and co-authors (1991), who studied the dynamics of changes in the tissues of knee joints destabilized by the intersection of anterior cruciate ligaments, disproved the previous authors' assumptions.
S.A. McDevitt and co-authors (1973, 1977) found that even during the first days after the crossing of the cruciate ligaments, the synthesis of proteoglycans by chondrocytes of articular cartilage increases. Within 64 weeks after surgical inducing knee instability, the thickness of the articular cartilage was higher than normal, although biochemical, metabolic and histological changes in it corresponded to those in osteoarthritis. This thickening of the cartilage was associated with an increased synthesis of proteoglycans and their high concentration in the articular cartilage. Using Magnetic Resonance Imaging (MPT), ME Adams and KD Brandt (1991) showed that after crossing the cruciate ligament, hypertrophy of the cartilage is maintained for 36 months, subsequently a progressive loss of cartilage occurs, so that after 45 months most of the articular surfaces are deprived cartilage. Morphological examination of cartilage 54 months after the operation confirmed the results of MRI. Thus, M.E. Adams and KD Brandt (1991) have shown that surgically induced instability of knee joints in dogs can be considered a model of OA.
The phenomenon of hypertrophic repair of articular cartilage is well illustrated by the above-described model of osteoarthritis in dogs. However, it is known that this phenomenon is inherent not only to it. Hypertrophy of articular cartilage, which was reparative in nature, was first described in patients with osteoarthritis EGL Bywaters (1937), and later LC Johnson. It is also found in other models of osteoarthritis - in rabbits after partial meniscactomy (Vignon E. Et al., 1983), in rhesus monkeys, cartilage hypertrophy develops spontaneously.
The current description of pathogenesis is mainly focused on the progressive "loss" of cartilage, but often the authors overlook the thickening and strengthening of the synthesis of proteoglycans, which corresponds to the homeostatic phase of stabilized osteoarthritis. During this phase, cartilage repair compensates for its loss and can maintain the joint in a functional state for a long time. But reparative tissue often can not cope with the mechanical load imposed on it in the same way as a healthy articular cartilage does, which leads to the inability of chondrocytes to maintain the normal composition of the matrix and reduce the synthesis of proteoglycans. The final stage of osteoarthritis develops.
The study of Sharko's arthropathy led to the appearance of a method of neurogenic acceleration of the modeling of surgically induced osteoarthritis. Charcot's arthropathy is characterized by severe destruction of the joints, articular "mice", effusion to the joint, instability of the ligaments, the formation of new bone and cartilaginous tissue within the joint. The general concept of the pathogenesis of Sharko's arthropathy (neurogenic) consists in interrupting sensitive signals from proprioceptors and nociceptors of the extremities into the central nervous system (CNS). To accelerate the progression of osteoarthritis induced by the intersection of the anterior cruciate ligament in dogs, a ganglionectomy or excision of the innervating joint of the nerve is performed before the operation, which leads to cartilage erosion in the first week after the operation. Interestingly, the new DMOAD diacerein was effective when used on a slowly progressive (neurologically intact) model of osteoarthritis, but with neurogenically accelerated experimental osteoarthritis, the drug was ineffective.
In conclusion, it should be noted that it is impossible to fully assess the identity of the experimental model of osteoarthritis and osteoarthrosis in humans, since the etiology and precise mechanisms of the pathogenesis of the disease have not yet been elucidated. As stated earlier, the main task of using experimental models of osteoarthritis in animals is their use to evaluate the effectiveness of new drugs, mainly the group of "disease modifying". The likelihood that the results of treatment of an animal will coincide with the results of using an experimental pharmacological agent in humans can also not be determined. NS Doherty and co-authors (1998) focused on the significant differences between animal species used to model osteoarthritis in terms of the different pathologies, different mediators, receptors, enzymes, leading to a biased extrapolation of the therapeutic activity of new drugs used in animals to humans . An example is the high effectiveness of NSAIDs in the modeling of inflammatory arthritis in rodents. This led to a reassessment of the effectiveness of NSAIDs in a person whose prostaglandins do not play that fundamental role in the pathogenesis of the disease they play in rodents, and the clinical efficacy of NSAIDs is rather limited to the treatment of symptoms rather than modification of the disease.
At the same time, underestimation of new pharmacological agents in the study of their effectiveness in animal models can lead to loss of potentially effective therapeutic agents in humans. For example, gold salts, penicillamine, chloroquine and sulfasalazine, which have a definite effect in the treatment of rheumatoid arthritis, are absolutely ineffective in animals used for screening antirheumatic drugs.
The difference between the animal's response to simulated osteoarthritis and a patient with osteoarthritis for DMOAD treatment depends largely on collagenase, an enzyme that is believed to be actively involved in the pathogenesis of osteoarthritis. In rodents with modeled OA, interstitial collagenase inhibitors (collagenase-1 or matrix metalloproteinase (MMP) -1) are often found, but the homologue of human collagenase-1 is not found in rodents, it probably does not exist. Thus, specific inhibitors of human collagenase-1 will not exhibit therapeutic efficacy in rodents with experimental osteoarthritis. Most MMP inhibitors created to date are non-selective and therefore inhibit collagenase-3 (MMP-13), which is involved in the pathogenesis of experimental osteoarthritis in rodents. Moreover, studies by NRA Beeley and co-authors (1994), JMP Freije and co-authors (1994) show that human collagenase-3 is expressed in the articular cartilage of patients with osteoarthritis and, possibly, plays a role in the pathogenesis of the disease.
It can be assumed that these mediators, receptors or enzymes play a similar role in the pathogenesis of simulated osteoarthritis in a particular animal and in humans. An example is the chemotactic ability of leukotriene B4, which is the same in humans, mice and rabbits, but the activity of antagonists of this biologically active substance between animal species is 1000 times different. In order to avoid such inaccuracies in experiments, it is necessary to create methods that allow investigating pharmacodynamics in vivo. For example, one can study the effect of any substances on the activity of exogenous enzymes or human mediators. This technique was applied by V Ganu and co-authors (1994) to assess the activity of MMP inhibitors by determining the ability of drugs to inhibit the release of proteoglycans from articular cartilage after injection of human stromolesin into the rabbit's knee.
Although the results obtained in the simulated osteoarthritis experiment may lead to an incorrect evaluation of potential DMOAD, the model of osteoarthrosis in animals plays an important role in basic studies. The final decision on the effectiveness of pharmacological agents in the treatment of human diseases can be done only after the third phase of clinical trials in humans.


 [
[