Epstein-Barr virus
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
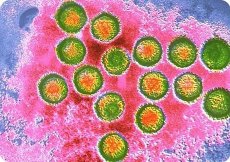
The Epstein-Barr virus (EB) causes infectious mononucleosis, which affects people of all age groups, as well as a tumor in the children and young men in Central Africa, most often the upper jaw - Burkitt's lymphoma and in adult men in China - nasopharyngeal carcinoma. The Epstein-Barr virus was first detected by electron microscopy of transplanted cells derived from Burkitt's lymphoma.
The Epstein-Barr virus differs significantly from other herpesviruses in antigenic properties. With the help of RSK, immunodiffusion and RIF, various antigens are detected. In the past, a membrane antigen (MA, or LYDMA: membrane antigen, or lymphocyte detected membrane antigen), complement-binding nuclear antigen (EBNA-Epstein-Barris nucleic antigen) is the most common; late antigen is the antigen of the viral capsid (VCA - virus capsid antigen).
The Epstein-Barr virus is very original in its interaction with the host cell that it afflicts: it causes not the death, but the proliferation of lymphocytes. The transformation of lymphocytes caused by the Epstein-Barr virus allows long-lasting cultivation; a positive RIF with an antiserum to the Epstein-Barr virus is detected. This transformation makes lymphocytes capable of endless fission. In all cells, the genomes of the Epstein-Barr virus appear in large numbers, and the nuclear antigen (EBNA) is released into the environment.
 [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13]
[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13]
Pathogenesis and symptoms of infectious mononucleosis
The pathogenesis of the infection caused by the Epstein-Barr virus is still little understood. In infectious mononucleosis, the Epstein-Barr virus enters the mucosa of the mouth and nasopharynx, then penetrates the regional lymph nodes, multiplies and spreads hematogenously. In the lymph nodes, tonsils and spleen, proliferation of reticular and lymphoid cells occurs with the formation of large mononuclear forms; Often there are focal necrosis. In the liver, lymphoid cell infiltrates can form.
The incubation period for infectious mononucleosis is from 4 to 60 days, usually 7-10 days. For the disease is characterized by a gradual development: the temperature rises, there is a pain in the throat, nasal breathing is disrupted, regional lymph nodes increase, tonsils appear on the tonsils. In the blood there is leukocytosis, one of the most characteristic signs of the disease is the appearance in the blood of atypical mature single-core cells of medium and large size with a broad basophilic protoplasm - atypical mononuclears and wide-plasma lymphocytes; their number is 10-15% or more. Complications (sinusitis, pneumonia, meningitis, nephritis) are rare, the prognosis is favorable. Very peculiar immunity. B-lymphocytes produce viral particles, but malignancy usually does not occur. This is due to the appearance of specific T-killers, the target of which is the viral antigen of MA on the surface of the B-lymphocyte. Natural killers, the K-cell mechanism, are activated. The activity of suppressors inhibiting proliferation and differentiation of B-lymphocytes and thereby preventing the multiplication of affected cells increases. When recovered, T-cells of memory appear, which destroy virus-infected B-lymphocytes after their restimulation. These cells circulate in the blood of those who have recovered for life. Viral neutralizing antibodies are also synthesized. With Burkitt's lymphoma and nasopharyngeal carcinoma, the affected cells contain multiple copies of the integrated genome of the Epstein-Barr virus, the EBNA antigen appears in the cell nuclei. In the blood of the patients, antibodies to the capsid antigen appear first of the IgM class, then of the IgG class. Later antibodies to early AM and EBNA antigens appear. Antibodies persist for life. To detect viral DNA in the affected transformed cells, the DNA probe method is used.

