Respiratory system of bronchi
Last reviewed: 23.04.2024

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
With a decrease in the caliber of bronchi, their walls become thinner, the height and number of rows of epithelial cells decrease. Beshbrian (or membranous) bronchioles have a diameter of 1-3 mm, there are no goblet cells in the epithelium, Clara cells perform their role, and the submucous layer passes into adventitia without a clear boundary. Membranous bronchioles become terminal with a diameter of about 0.7 mm, their epithelium is single-rowed. From the terminal bronchioles respiratory bronchioles with a diameter of 0.6 mm depart. Respiratory bronchioles through the pores are associated with the alveoli. Terminal bronchioles are air-conducting, respiratory - take part in air and gas exchange.
The total area of the terminal section of the respiratory tract is many times larger than the area of the trachea and large bronchi (53-186 cm 2 vs. 7-14 cm 2 ), but bronchioles account for only 20% of airflow resistance. Due to the small resistance of the terminal sections of the respiratory tract in the early stages, bronchiolar involvement can be asymptomatic, not accompanied by changes in functional tests, and is an accidental finding in high-resolution computed tomography.
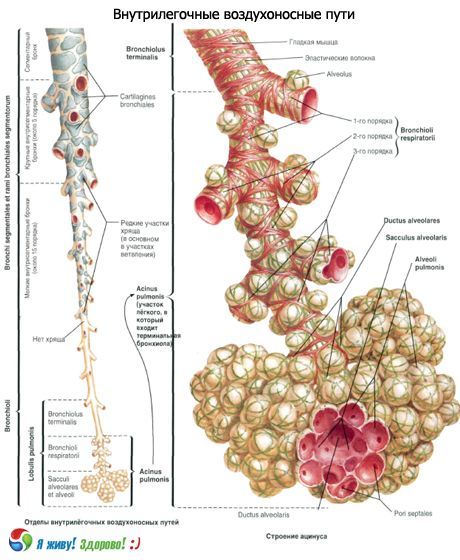
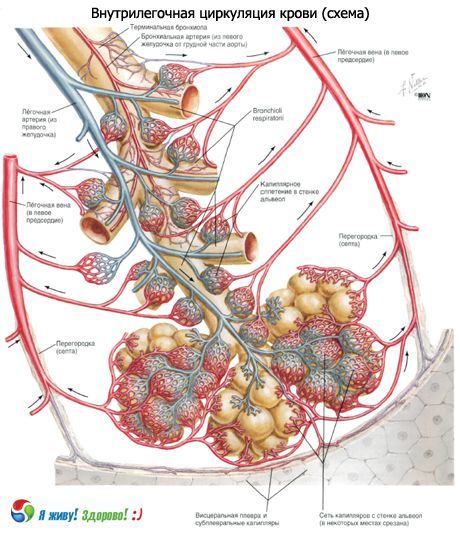
According to the International Histological Classification, a set of ramifications of terminal bronchioles is called the primary pulmonary lobe, or acinus. This is the most numerous structure of the lung, in which gas exchange takes place. In each lung, there are 150,000 acinus. Acinus of adult diameter of 7-8 mm, has one or more respiratory bronchioles. Secondary pulmonary lobe is the smallest unit of the lung, limited by septa of connective tissue. Secondary pulmonary lobules consist of 3 - 24 acini. The central part contains the pulmonary bronchioles and the artery. They are designated by the lobular nucleus or "centrilobular structure". Secondary pulmonary lobules are divided by interlobular septa containing veins and lymphatic vessels, arterial and bronchiolar branches in the lobular nucleus. The secondary pulmonary lobule is usually polygonal with a length of each of the constituent sides of 1-2.5 cm.
The connective tissue carcass of the lobule consists of interlobular partitions, intra-lobular, centrilobular, peribronchovascular, subpleural interstitium.
Terminal bronchioles are divided into 14-16 respiratory bronchioles of the first order, each of which in turn is dichotomously divided into respiratory bronchioles of the second order, and they are dichotomously divided into third-order respiratory bronchioles. Each respiratory bronchioles of III order is subdivided into alveolar courses (diameter 100 microns). Each alveolar course ends with two alveolar sacs.
Alveolar courses and sacs in their walls have protrusions (vesicles) - the alveoli. Alveolar course involves about 20 alveoli. The total number of alveoli reaches 600-700 million with a total area of about 40 m 2 with exhalation and 120 m 2 with inspiration.
In the epithelium of respiratory bronchioles, the number of ciliated cells progressively decreases and the number of non-exfoliated cubic cells and Clara cells increases. Alveolar courses are lined with a flat epithelium.
A great contribution to the modern understanding of the structure of the alveolus was made by electron microscopic studies. Over a large extent, the walls are common to two adjacent alveoli. In addition, the alveolar epithelium covers the wall from two sides. Between the two sheets of the epithelial lining is interstitium, in which septal space and the network of blood capillaries are distinguished. In the septal space there are bundles of fine collagen fibers, reticulin and elastic fibers, a few fibroblasts and free cells (histiocytes, lymphocytes, neutrophilic leukocytes). Both the epithelium and the endothelium of the capillaries lie on the basal membrane with a thickness of 0.05-0.1 μm. In places, the subepithelial and subendothelial membranes are separated by septal space, in places touching, forming a single alveolar-capillary membrane. Thus, the alveolar epithelium, the alveolar-capillary membrane, and the layer of endothelial cells are components of the air-blood barrier through which gas exchange takes place.
Alveolar epithelium is heterogeneous; it distinguishes between cells of three types. Alveolocytes (pneumocytes) type I cover most of the surface of the alveoli. Gas exchange is carried out through them.
Alveolocytes (pneumocytes) of type II, or large alveolocytes, have a rounded shape and protrude into the lumen of the alveoli. On their surface are microvilli. The cytoplasm contains numerous mitochondria, a well-developed granular endoplasmic reticulum and other organelles, of which the osmiophilic plate-like bodies surrounded by a membrane are most characteristic. They consist of an electronically dense layered substance containing phospholipids, as well as protein and carbohydrate components. Like secretory granules, lamellar bodies are released from the cell, forming a thin (about 0.05 micron) surfactant film that reduces the surface tension, preventing the alveoli from falling off.
Alveolocytes of type III, described under the name of brush cells, are distinguished by the presence of short microvilli on the apical surface, numerous vesicles in the cytoplasm and bundles of microfibrils. It is believed that they carry out fluid absorption and concentration of surfactant or chemoreception. Romanova L.K. (1984) suggested that their neurosecretory function.
In the alveolar lumen, a few macrophages normally absorb dust and other particles. At present, the origin of alveolar macrophages from blood monocytes and tissue histiocytes can be considered established.
Reduction of smooth muscles leads to a decrease in the base of the alveoli, a change in the configuration of the vesicles - they also lengthen. It is these changes, and not the gaps in the septum, that underlie bloating and emphysema.
The configuration of the alveoli is determined by the elasticity of their walls, which are stretched due to the increase in the volume of the thorax, and the active contraction of the smooth muscles of the bronchioles. Therefore, with the same volume of respiration, different stretching of the alveoli in different segments is possible. The third factor determining the configuration and stability of the alveoli is the force of the surface tension formed at the boundary of two media: air filling the alveolus and a liquid film lining its inner surface and protecting the epithelium from drying out.
To counteract the surface tension (T), which tends to compress the alveoli, a certain pressure (P) is necessary. The quantity P is inversely proportional to the radius of curvature of the surface, which follows from the Laplace equation: P = T / R. It follows that the smaller the radius of curvature of the surface, the higher the pressure is necessary to maintain a given volume of alveoli (at constant T). However, the calculations showed that it would have to exceed the intra-alveolar pressure existing in reality many times over. When exhaling, for example, the alveoli would have to subside, which is not the case, since the stability of the alveoli at low volumes is provided by a surface-active substance, a surfactant, which reduces the surface tension of the film with a decrease in the area of the alveoli. This is the so-called anti-teleleptatic factor discovered in 1955 by Pattle and consisting of a complex of substances of a protein-carbohydrate-lipid nature, which includes a lot of lecithin and other phospholipids. The surfactant is produced in the respiratory department by alveolar cells, which together with the cells of the superficial epithelium lining the alveoli from the inside. Alveolar cells are rich in organoids, their protoplasm contains large mitochondria, therefore they are distinguished by high activity of oxidative enzymes, they also contain nonspecific esterase, alkaline phosphatase, lipase. Of greatest interest are inclusions occurring continuously in these cells, determined by electron microscopy. These osmiophilic bodies are oval-shaped, 2-10 microns in diameter, of a lamellar structure, bounded by a single membrane.
Surfactant system of the lungs
The surfactant lung system performs several important functions. The surface-active substances of the lungs reduce the surface tension, and the work necessary for ventilation of the lungs stabilizes the alveoli and prevents their atelectasis. In this case, the surface tension increases during inspiration and decreases during exhalation, reaching a value close to zero at the end of the exhalation. The surfactant stabilizes the alveoli by immediately decreasing the surface tension with decreasing alveolar volume and increasing the surface tension with increasing alveolar volume during inspiration.
The surfactant creates conditions for the existence of alveoli of different sizes. If there was no surfactant, then the small alveoli, dropping, would transmit air larger. The surface of the smallest respiratory tract is also covered with a surfactant, which ensures their patency.
For the functioning of the distal part of the lung the most important is the patency of the bronchoalveolar anastomosis, where the lymphatic vessels, lymphoid accumulations are located and the respiratory bronchioles begin. Surfactant, covering the surface of respiratory bronchioles, comes here from the alveoli or is formed locally. Substitution of surfactant in bronchioles with the secretion of goblet cells leads to narrowing of the small airways, increasing their resistance and even complete closure.
The clearance of the contents of the smallest airways, where the transportation of the contents is not associated with the ciliary apparatus, is largely provided by the surfactant. In the zone of functioning of the ciliated epithelium, the dense (gel) and liquid (sol) layers of bronchial secretion exist due to the presence of the surfactant.
The surfactant system of the lung participates in the absorption of oxygen and the regulation of its transport through the air-blood barrier, as well as in maintaining the optimal level of filtration pressure in the pulmonary microcirculation system.
The destruction of the surfactant film by a twin causes atelectasis. Inhalation of aerosols of lecithin compounds, on the contrary, gives a good therapeutic effect, for example, in case of insufficient respiration in newborns, in which bile acids can destroy the film during aspiration of fetal waters.
Hypoventilation of the lung leads to the disappearance of the surfactant film, and the restoration of ventilation in the collapsed lung is not accompanied by a complete restoration of the surfactant film in all the alveoli.
The surfactant properties of the surfactant also change with chronic hypoxia. With pulmonary hypertension, there was a decrease in the amount of surfactant. As shown by experimental studies, violation of bronchial patency, venous congestion in a small circle of blood circulation, a decrease in the respiratory surface of the lungs contribute to a decrease in the activity of the surfactant lung system.
An increase in the concentration of oxygen in the inspired air leads to the appearance in the lumens of alveoli of a large number of membrane formations of the mature surfactant and osmiophilic bodies, which indicates the destruction of the surfactant on the surface of the alveoli. The tobacco surfactant system is adversely affected by tobacco smoke. Reduction of the surface activity of the surfactant is caused by quartz, asbestos dust and other harmful impurities in the inspired air.
In the opinion of the authors' authors, the surfactant also prevents transudation and edema and has a bactericidal effect.
The inflammatory process in the lungs leads to changes in surfactant properties of the surfactant, and the degree of these changes depends on the activity of inflammation. Even more severe negative impact on the surfactant lung system is caused by malignant neoplasms. With them, surfactant properties of the surfactant decrease much more often, especially in the atelectasis zone.
There are reliable data on the disruption of surfactant surfactant activity during long (4-6 hours) fluorotanic anesthesia. Operations involving the use of cardiopulmonary bypasses are often accompanied by significant impairments in the surfactant lung system. Known defects of the surfactant system of the lungs are also known.
Surfactant can be detected morphologically by the method of luminescent microscopy due to primary fluorescence in the form of a very thin layer (from 0.1 to 1 micron) lining the alveoli. In an optical microscope, it is not visible, moreover, it breaks down when the preparations are treated with alcohol.
It is believed that all chronic respiratory diseases are associated with a qualitative or quantitative deficiency of the surfactant system of the respiratory system.


 [
[