Medical expert of the article
New publications
Visual acuity: Visual acuity test
Last reviewed: 06.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Central vision is the vision that determines the perception of an object fixed by the gaze. Central vision is carried out by the sensors of the central fovea of the macula of the retina and is characterized by the greatest visual acuity. The impulse from each cone of the central fovea of the retina passes through separate nerves through all parts of the visual pathway, which guarantees the highest visual acuity.
Spatial visual acuity is the ability to distinguish individual elements of an object or perceive it as a whole. It is quantitatively equivalent to the minimum angle of discrimination, calculated from the nodal point of the eye between two objects, allowing them to be seen separately. The minimum angle of discrimination is 1 arc minute or less, which corresponds to line 6/6 on Snellen optotypes from a distance of 6 m.
Visual acuity is the sensitivity of the visual analyzer, which reflects the ability to distinguish the components and boundaries of noticeable objects; it is oriented by the minimum angular distance between two points, at which they are perceived separately. The smallest angular distance approximately corresponds to one minute, at this value the size of the image on the retina is 0.004 mm, which corresponds to the diameter of the cone. The visual analyzer is able to capture objects that are larger than the diameter of the cone. The component parts of an object are distinguished when excited cones are separated by even one unexcited one.
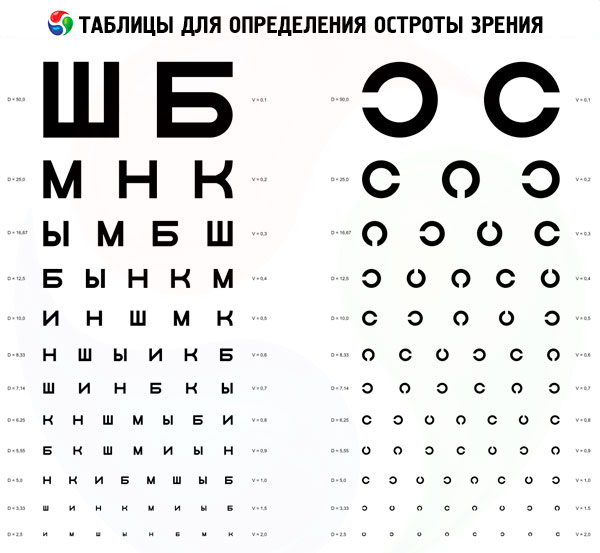
To study visual acuity, special tables are used that contain optotypes of different sizes (letters, numbers, signs).
Indications for visual acuity testing
Patient complaints about decreased vision. Visual acuity is also determined during preventive examinations.
Preparation for visual acuity testing
Equipment: Roth apparatus, Golovin-Sivtsev table (children's visometry tables), pointer, bright light source (to determine light projection).
Before the procedure for determining visual acuity, the patient is explained the procedure for conducting the study.
Methodology and interpretation of visual acuity testing
The patient sits at a distance of 5 meters from the table. The visual acuity test is performed alternately: first for the right (OD), then for the left (OS) eye. The eye that is not participating in the test is covered with a shield (a sheet of paper, a palm). The table symbols are presented for 2-3 seconds and the patient is asked to name them. Make sure that the pointer does not interfere with reading the symbols. Visual acuity is determined by symbols of the minimum size that the patient can recognize. There can be no errors when reading the first 7 lines; starting from the 8th line, one error in a line is neglected (visual acuity is indicated in any row to the right of the optotypes).
Example of data registration: Visus OD=1.0; Visus OS 0.6.
If the visual acuity is less than 0.1 (the patient does not see the first line of the chart from a distance of 5 meters), he should be brought to a distance (d), from which he will be able to name the symbols of the first row (the normal eye recognizes the symbols of this row from 50 m; D = 50 m). Calculation using the Snellen formula:
Visus=d/D (m),
Where Visus (Vis, V) is visual acuity;
D - the distance from which the patient reads the 1st row:
D is the calculated distance from which the components of the symbols in this row are visible at a visual angle of 1 (indicated in any row to the left of the optotypes).
If the patient does not recognize the symbols of the 1st row from a distance of 50 cm, then the visual acuity is characterized by the distance from which he is able to count the spread fingers of the hand presented by the doctor (example: Visus OD = counting fingers from a distance of 15 cm from the face). If the patient is unable to count fingers, although he sees the movement of the hand near the face, then the data on visual acuity are recorded as follows: Visus OS = movement of the hand near the face.
The lowest visual acuity is the ability of the eye to distinguish light from darkness; this is tested in a darkened room by illuminating the eye with a clear beam of light. If the patient sees light, then visual acuity is equal to light perception (Visus OD= 1/*, or perceptio lutis). By directing a beam of light at the eye from different sides (above, below, right, left), a test is performed to see how well the ability of individual areas of the retina to capture light is preserved. Correct answers are shown on the correct projection of light (Visus OD=1/* proectio lucis certa). In case of clouding of the oetic media of the eye (cornea, lens, CT), visual acuity may be reduced to light perception, but the projection of light is almost always determined correctly. In case of an erroneous projection of light, it is necessary to show from which side the patient sees the light (for example, light perception from the temple, above and below).
The absence of a correct projection of light (perceptio et proectio lucis incerta) in the subject or the absolute absence of light perception (Visus=O) indicates damage to the retina or optic nerve.
In English-speaking countries, visual acuity is traditionally determined from a distance of 20 feet or 6 m (there are 30.5 cm in one foot) and is written down using the Snellen formula as a fraction.
Testing visual acuity in children in the preverbal phase of development
A comparative assessment of the vision of both eyes is carried out by simply observing the child.
- Covering one eye, which is perceived negatively by the child, indicates low visual acuity of the fellow eye.
- The fixation test is carried out as follows:
- a 16 D prism is placed with its base down in front of one eye, while the other eye is covered;
- the eye behind the prism deviates upward, maintaining fixation;
- observe the eye located behind the prism;
- fixation is assessed as central or non-central, stable or unstable;
- open the other eye and determine the ability to maintain fixation;
- if the slightly open eye becomes fixated, then visual acuity is reduced;
- if fixation remains after blinking, visual acuity is high;
- if fixation alternates, visual acuity in both eyes is equal;
- the test is repeated by placing the prism in front of the other eye;
- Monocular fixation must be central, stable, and maintained by each eye.
- The Hundreds and Thousands of Sweets Test is a large test that is rarely performed. Typically, a child is able to see and pick up small sweets at a distance of 33 cm with a visual acuity of at least 6/24.
- The rotation test is quantitative and evaluates the child's ability to fix the gaze with both eyes open. It is carried out as follows:
- the examiner holds the child facing him/her and quickly rotates him/her 360;
- with normal vision, the child's gaze is directed towards rotation under the influence of the vestibular-ocular reflex. The eyeballs intermittently return to the primary position, which is accompanied by rotational nystagmus;
- when rotation stops, nystagmus disappears with suppression of post-rotational nystagmus by restoration of fixation;
- If vision is significantly reduced, the induced nystagmus does not disappear after rotation stops, since the vestibular-ocular reflex is not blocked by the principle of visual feedback.
- Preferential fixation techniques can be used from infancy. Infants tend to respond to a pattern rather than a homogeneous stimulus. The infant is shown a stimulus and the examiner observes the fixation movements of the eyes. Examples of stimuli include Teller charts for visual acuity testing, which consist of black bars of varying thickness, and Cardiff charts, which consist of shapes with varying contours. Thick bars or shapes with thick contours (with low spatial frequency) are seen better than those with thin ones, and visual acuity is assessed accordingly. In amblyopia, visual acuity determined by gratings is often higher than that estimated by Snellen optotypes; in turn, visual acuity determined by Teller charts may also be overestimated.
- Pattern-evoked visual cortical potentials reflect spatial contrast sensitivity. They are used primarily to diagnose optic neuropathy.
- Optokinetic nystagmus may indicate visual acuity depending on the size of the bands.
Testing visual acuity in children in the verbal phase of development
- By age 2, most children have acquired sufficient language skills to name optotype pictures, such as those according to Kau.
- By age 3, most children can recognize individual optotypes in the Sheridan-Gardiner test. The disadvantage of this method is that it overestimates visual acuity in amblyopia because it does not produce the phenomenon of "crowding." The Keeler LogMAR test is more chart-like and more accurate for determining visual acuity in amblyopia because it requires the child to match a pair from a group of optotypes.
- By age 4, most children can have their visual acuity tested using Snellen charts.
Study of stereopsis
Stereopsis is measured in arc seconds (1 = 60 arc minutes; 1 arc minute = 60 arc seconds). It should be remembered that normal spatial visual acuity is 1 arc minute, and normal stereostrophy is 60 seconds (which corresponds to 1 minute). The lower the value, the higher the acuity.
Titmus test
This is a three-dimensional polaroid vectorograph in the form of a booklet, consisting of two tables viewed by the patient through polaroid glasses. On the right side of the booklet is a large fly, on the left - circles and animals. The test is carried out at a distance of 405 mm.
- "Fly" - a test for coarse stereopsis (3000 arc seconds), especially informative for small children. The fly should look three-dimensional, and the child is asked to "lift" it by one of its wings. In the absence of coarse stereopsis, the fly looks flat, as in the photograph (if you turn the booklet over, the image becomes flat). If the patient insists that the fly's wings protrude, the assessment of stereoscopic vision is incorrect.
- "Circles" is a series of step tests for assessing stereo vision. Each of the Y squares consists of 4 circles. Each of the circles has a certain degree of disparity and, with normal stereopsis, protrudes in front of the plane. Stereoscopic visual acuity is calculated using the table attached to the test. The angle of disparity is from 800 to 40 arc seconds. If the patient sees a shift of the circle to the side, he does not have stereoscopic vision and is oriented monocularly.
- "Animals". The test is similar to the circle test and consists of 3 rows of animals, one of which protrudes in front of the plane. The degree of dissimilarity is from 400 to 100 arc seconds.
TNO test
The Random Dots test consists of 7 tables viewed through red-green glasses. Each table shows various figures (squares, crosses, etc.) formed from random dots of complementary colors. Some figures are visible without red-green glasses, while others are "hidden" and visible only with stereoscopic vision in red-green glasses. The first 3 tables are designed to identify stereoscopic vision, and the following ones - to quantify it. Since the TNO test does not contain monocular "hints", it measures stereopsis more accurately than the Tiimus test. Disparity ranges from 480 to 15 arc seconds.
Lang test
This test does not require special glasses. Objects are visualized separately by each eye through built-in elements with cylindrical lenses. The displacement of dots creates disparity. The patient is asked to name or point to a simple figure on a card, such as a star. The Lang test is especially informative for assessing stereopsis in small children and infants, since they instinctively stretch out their hands and point to pictures. The examiner can watch the child's eye movements from one picture to another. Disparity ranges from 1200 to 600 arc seconds.
Frisby Test
The test consists of 3 transparent plastic plates of varying thickness. On the surface of each plate are printed 4 squares with small random figures. In one of the squares there is a "Hidden" circle, within which the figures are printed on the back of the plate. The patient is required to identify this hidden circle. The test does not require special glasses, since the disparity is created by the thickness of the plate and can be varied by approaching and moving away from the plate. Disparity ranges from 600 to 15 arc seconds.
Prism with base facing outwards
A quick and easy method for detecting binocular vision in children who cannot undergo stereo testing. The test is performed as follows: a 20 D prism is placed with its base outward in front of the eye (in this case, the right). This shifts the retinal image toward the temple, inducing diplopia. The examiner observes the adjustment movement:
- movement of the right eye to the left to restore fixation (adduction on the right) with a corresponding movement of the left eye to the left (abduction on the left) in accordance with Hering's law;
- the left eye makes an adjusting movement to the right (readduction to the left);
- removing the prism, observe the movement of both eyes to the right;
- the left eye moves to the right to restore fusion.
Most children with good binocular vision should be able to overcome a 20 D prism, otherwise weaker prisms (16 D or 12 D) should be used.
Investigation of sensory abnormalities
Worth's Four Point Test
Conducting
- The patient is given a red lens in front of the right eye, which cuts off all colors except red; a green lens is given in front of the left eye, which cuts off all colors except green;
- The patient is shown a drum with 4 circles: 1 red, 2 green and 1 white.
Results
- All figures are visible - normal fusion.
- The visibility of all figures in the presence of a manifest form of strabismus indicates ACS.
- The patient sees 2 red figures - suppression of the left eye.
- The patient sees 3 green figures - suppression of the right eye.
- The patient sees 2 red and 3 green figures - the presence of diplopia.
- If the green and red figures alternate, then alternating suppression is present.
Bagolini striped glasses
Each lens is coated with tiny stripes, and a point source of light viewed through them becomes a line, similar to a Maddox wand.
Conducting
- two lenses at an angle of 45 and 135 are placed in front of each eye, and the patient fixates on a point source of light;
- each eye perceives an oblique line of light, perpendicular to the line perceived by the paired eye;
- different images appear before each eye under conditions of bi-ocularity.
The results cannot be interpreted correctly until the fact of the existence of manifest strabismus is known.
- Two stripes intersect in the center, forming an oblique cross ("X") - the patient has orthotropy or ACS.
- Two lines are visible, but not in the shape of a cross - the patient has diplopia.
- If only one stripe is visible, then simultaneous perception does not occur.
- In one of the stripes a small gap is visible - there is a central suppression scotoma.
Sequential image
The test demonstrates the visual direction of the fovea.
Conducting
- one fovea is stimulated by a vertical strip of bright light, and the other by a horizontal one;
- The vertical stripe is more difficult to suppress, so it is projected onto the fovea of the squinting eye.
Results: The patient draws the relative positions of successive images.
- Two consecutive images intersect in the form of a cross - the correspondence of the retinas is normal.
- If two consecutive images do not intersect, then ACS is diagnosed.
- If, in esotropia with ACS, the horizontal sequential image is projected onto the right fovea, it is seen to the left of the vertical image.
- The opposite results are obtained with exotropia.
- A patient with eccentric fixation will also see a cross. Eccentric fixation is a unilateral condition in which the extrafoveal portion of the fovea is used for fixation under binocular and monocular conditions. The reorientation of sensory and motor functions occurs in such a way that this area usurps the primary visual image belonging to the fovea. On the fovea of the dominant eye, the successive image is projected directly from the visual space. The successive image on the eccentric area of the squinting eye will also be projected directly from the visual space, since the area has "lost" the primary visual direction.


 [
[