Medical expert of the article
New publications
Vaginal trichomonas
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
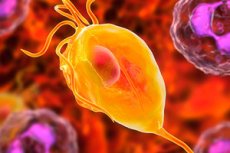
Vaginal trichomonas, or Trichomonas vaginalis, is a single-celled microorganism that can cause a vaginal disease called trichomoniasis. Trichomonas vaginalis is a parasite and is sexually transmitted during sexual intercourse.
Here is some information about vaginal trichomonas and trichomoniasis:
- Symptoms: Trichomoniasis can present with a variety of symptoms, including itching, burning, vaginal discharge (usually greenish-yellow in color and odor), pain during intercourse, and vaginal discomfort. Some women may be asymptomatic.
- Diagnosis: Trichomoniasis is usually diagnosed by laboratory testing of a sample of vaginal discharge or urine to detect Trichomonas vaginalis.
- Treatment: Trichomoniasis is treated with antiparasitic drugs that are usually taken orally. Treatment should be prescribed by a doctor.
- Consequences: If left untreated, trichomoniasis can cause other gynecologic infections and increase the risk of contracting other sexually transmitted infections, including HIV. In pregnant women, trichomoniasis can also increase the risk of pregnancy complications and premature babies.
- Prevention: Using condoms during sex can reduce the risk of transmitting trichomoniasis and other sexually transmitted infections.
Structure of the vaginal trichomonas
Trichomonas vaginalis (Trichomonas vaginalis) is a single-celled microorganism that causes a vaginal infection called trichomoniasis. The structure of Trichomonas vaginalis includes the following basic elements:
- Trichomonadbody: Trichomonads have a piring or oval body that is usually small and moves thanks to flagella (hair-like motors).
- Flagella (hair-like motors): This is one of the characteristic features of trichomonads. It has a number of long hair-like motors, or flagella, which provide the microorganism with motility and its ability to move in a liquid medium.
- Cytoplasm: Inside the trichomonad is the cytoplasm, which contains various organelles, including the nucleus, mitochondria, and other structures necessary for cell life.
- Envelope and membranes: Trichomonads possess an envelope or membrane that surrounds their cell.
- Nucleus: The nucleus contains the genetic information necessary for the microorganism to function.
- Blue corpuscles: Blue corpuscles may be present in the cytoplasm of trichomonads, which are structures containing iron and sulfur that play a role in metabolism and energy processes.
The structure of vaginal trichomonads can vary depending on their condition and environment. Trichomonads are usually found in vaginal swabs in the diagnosis of trichomoniasis.
Life cycle of the vaginal trichomonas
Vaginal trichomonas, or Trichomonas vaginalis, is a protozoan microorganism that causes an infection known as trichomoniasis (trichomoniasis vaginalis). The life cycle of vaginal trichomonas can be described as follows:
- Trophozoites (trophonts): This is the active and infective form of vaginal trichomonads. Trophozoites have a characteristic shape with flagella (flagella) that are used for movement and attachment to the cells of the vaginal mucosa. This form of microorganism is capable of causing symptoms of infection.
- Fission and replication: Trophozoites can divide by binary fission, leading to an increase in their numbers in the vagina.
- Active infection: Trophozoites can cause inflammation and irritation of the vaginal mucosa, which can lead to symptoms of trichomoniasis, including itching, burning, urinary pain and discharge.
- Passive form: Under certain conditions, such as dryness or low oxygen levels, trophozoites can transform into a more inactivated and stable form called a cyst. Cysts can survive in the external environment and serve as a source of infection.
- Spread: Vaginal trichomonas is spread through sexual contact, including vaginal and oral sex. It can also occur through the use of shared items such as towels or underwear.
- Cycle of infection: Vaginal trichomonas can cause recurring episodes of infection, especially if not adequately treated. This makes the infection chronic in some cases.
Pathways of infection
The route of infection for vaginal trichomonas (Trichomonas vaginalis) is the sexual route, and the infection is transmitted during sexual intercourse. Here is more information about the routes of infection:
- Sexualcontact: The main way of contracting trichomoniasis is through sexual contact with an infected partner. Trichomonads can be found in the vaginal or urethral secretions of an infected woman or man. Transmission occurs during sexual intercourse through contact with infected secretions.
- Vertical transmission: Vertical transmission of trichomoniasis from an infected mother through the birth can occur in newborn infants. This is, however, a rare occurrence.
- Public places: Contrary to some myths, trichomonas is not transmitted through public toilets, swimming pools, bathtubs or objects such as towels. It cannot survive for long periods of time outside the body and is not spread outside of sexual contact.
To prevent infection with trichomoniasis, the use of condoms during sexual intercourse is recommended. Condoms can reduce the risk of transmission but do not eliminate it completely, as trichomonas can be found not only in the genital area but also in the urethra, urethra, urethra and vagina.
Pathogenesis
The pathogenesis of vaginal trichomonas (Trichomonas vaginalis) is related to its ability to cause infection in the vagina of women and the urethra in men. The infection process and pathogenesis may be as follows:
- Sexual contact: Trichomonas vaginalis is sexually transmitted during sexual contact with an infected partner. This means that a person can become infected with Trichomonas vaginalis through unprotected sex with an infected partner.
- Introduction into the vagina: After contact with the vaginal or urethral mucosa, trichomonads can invade the epithelial cells and begin reproduction.
- Tissue damage: The reproduction process of trichomonads can cause tissue damage to the mucous membrane of the vagina or urethra. This can lead to inflammation, irritation and symptoms such as itching, burning and pain.
- Discharge and inflammation: Trichomonas vaginalis can cause changes in the composition of the vaginal discharge. Usually, the discharge in trichomoniasis is greenish-yellow in color and has an unpleasant odor. The discharge may contain a large number of inflammatory cells and leukocytes, indicating an inflammatory response from the body.
- Increased risk for other infections: Trichomonas can increase the vulnerability of the mucous membrane, making it more susceptible to other infections. For example, it can increase the risk of HIV and other sexually transmitted infections.
Symptoms
Trichomoniasis (a vaginal infection caused by trichomonads) can present with a variety of symptoms. Some women may be asymptomatic, while other women may experience the following signs and symptoms:
- Vaginal discharge: One of the most characteristic symptoms of trichomoniasis is copious, foaming, greenish-yellowish or grayish-greenish vaginal discharge. They may have an unpleasant odor reminiscent of fish odor.
An infection caused by vaginal trichomonas (Trichomonas vaginalis) can be accompanied by various types of vaginal discharge, which may include the following characteristics:
- Abundance: The discharge from trichomoniasis can be profuse and wet. This may result in the need for frequent changes of underwear or the use of sanitary pads.
- Color: Usually the discharge in trichomoniasis is greenish-yellow in color, although it can also be grayish or grayish-green.
- Odor: The discharge may have an unpleasant odor that is usually described as fishy or metallic.
- Consistency: Trichomoniasis discharge often has a liquid or frothy consistency.
- Accompanying symptoms: In addition to discharge, the infection may be accompanied by itching, burning, pain or discomfort in the vagina.
It is important to note that not all women infected with trichomonads show symptoms, and the infection can be asymptomatic.
- Vaginal itching and irritation: Many women with trichomoniasis experience itching, burning and irritation in the vaginal and external genital area.
- Swellingand redness: Inflammation of the vaginal walls can lead to swelling and redness.
- Pain when urinating: In some women, trichomoniasis can cause discomfort and pain when urinating.
- Lower abdominal pain: In some cases, an infection can cause pain or discomfort in the lower abdomen.
- Pain during sex: An infection can lead to pain or discomfort during intercourse.
- Sexual contact and dysuria: Trichomoniasis can be sexually transmitted and men may also experience dysuria (pain and difficulty urinating).
- Asymptomatic course: Some women and men may have the infection without obvious symptoms.
It is important to note that the symptoms of trichomoniasis can vary in intensity and duration.
In men, the symptoms of trichomoniasis can manifest in a variety of ways and may include the following signs:
- Urethral burning and itching: Men with trichomoniasis may experience burning and itching in the urethra (urethra).
- Pain or discomfort when urinating: An infection can cause pain or discomfort when urinating.
- Urethral discharge: Some men may experience urethral discharge that may be white, greenish, or grayish. The discharge may have an unpleasant odor.
- Pain or discomfort in the scrotal area: Some men may experience pain or discomfort in the scrotal area.
It is important to note that in some men, trichomonas infection can be asymptomatic, that is, with no visible signs. Asymptomatic infections can be dangerous because the man is unaware of his status and can transmit the infection to partners.
Trichomonas in children
Vaginal trichomonas infection (trichomoniasis) is usually associated with sexual activity and is more common in adolescents and adults. In children, trichomoniasis is extremely rare, and if it occurs, it occurs mainly in children who have been sexually abused.
It is important to realize that trichomoniasis is a sexually transmitted infection and in children it is not usually the result of normal childhood activities or play. If you suspect that a child may be infected with trichomonas or another sexually transmitted infection, you should:
- Seek medical attention: If you suspect an infection in your child, it is important to see a pediatrician or pediatric infectious disease specialist immediately. The doctor will perform an examination, ask questions and, if necessary, send for appropriate tests.
- Child Safety Concerns: If sexual abuse or inappropriate sexual contact is suspected, law enforcement should be contacted immediately and a child protection professional should be included.
- Testing and treatment: After diagnosis, the doctor will determine what treatment is needed. Antibiotics may be prescribed to treat trichomoniasis, but treatment should only be prescribed by a doctor.
It is important to provide children with information about sexual lifestyles, how to prevent sexually transmitted infections and that sexual contact should not occur without consent and at inappropriate ages.
Complications and consequences
Vaginal trichomonas (Trichomonas vaginalis) can cause various complications and consequences, especially if the infection is untreated or recurrent. The uncontrolled spread of this microorganism can lead to the following problems:
- Chronic infection: An uncontrolled or inadequately treated vaginal trichomonas infection can become chronic, which means it will recur and lead to recurrent symptoms and discomfort.
- Spread of other infections: Vaginal trichomonas can increase the risk of contracting other infections, including human immunodeficiency virus (HIV) and other sexually transmitted infections.
- Increased risk in pregnantwomen: In pregnant women, vaginal trichomonas infection may be associated with pregnancy complications such as preterm labor and low birth weight.
- Pelvic inflammatory disease: In women, infection can lead to the development of pelvic inflammatory disease (PID), including endometritis and salpingitis, which can lead to pain and complications in the long term.
- Increased risk of transmission of sexually trans mitted infections: Infection with vaginal trichomonas can increase the risk of transmission of other sexually transmitted infections such as chlamydia, gonorrhea, and others because it can damage the mucous membranes and mucous membranes of the genitals, making them more vulnerable.
- Link to cervical cancer: Several studies have shown that infection with vaginal trichomonads may increase the risk of cervical cancer, although this link requires additional research to better define.
Diagnostics
Diagnosis of vaginal trichomonas (Trichomonas vaginalis) usually involves the following methods:
- Microscopic smear examination: This method involves taking a swab from a woman's vagina or a man's urethra and then examining it under a microscope. Trichomonads may be visible in the smear as moving microorganisms. However, this method may be less sensitive and requires some skill to diagnose.
- Culture test: The swab sample can be seeded on special media for culturing Trichomonas vaginalis. This method may take longer, but helps to confirm the presence of the microorganism and determine its sensitivity to antiparasitic drugs.
- Molecular methods: Modern molecular diagnostic methods such as PCR (polymerase chain reaction) can be used to detect and identify Trichomonas vaginalis in a swab sample. These methods are usually more sensitive and specific.
- Diagnosis by symptoms: The presence of characteristic symptoms such as itching, burning, unusual vaginal discharge and discomfort may also lead the doctor to suspect trichomoniasis. However, laboratory testing is required to confirm the diagnosis.
Differential diagnosis
Differential diagnosis of vaginal trichomonas infection (trichomoniasis) involves identifying and distinguishing this condition from other vaginal infections and conditions that may cause similar symptoms. Here are some of the most common diagnostic methods and conditions to consider in the differential diagnosis:
- Candidiasis: A yeast infection caused by the fungus Candida can mimic the symptoms of trichomoniasis, such as itching, burning, and discharge. However, in candidiasis, the discharge is more likely to be white in color and have a characteristic raw odor.
- Chlamydia: This is a viral disease caused by the bacterium Chlamydia trachomatis, which can also be manifested by vaginal discomfort, changes in discharge and lower abdominal pain. Laboratory analysis is required for differential diagnosis.
- Gonorrhea: Infection with the gonococcus bacteria Neisseria gonorrhoeae can cause similar symptoms, including burning and discomfort. Laboratory testing is required for an accurate diagnosis.
- Bacterial vaginosis: This is a condition caused by an imbalance of bacteria in the vagina and can be manifested by a foul odor and changes in discharge. However, bacterial vaginosis usually lacks the itching and burning that characterizes trichomoniasis.
- Pelvic inflammatorydisease: Inf lammatory conditions such as salpingitis and endometritis can cause lower abdominal pain and fever, which are not always characteristic of trichomoniasis.
- Allergic reaction: Sometimes symptoms such as itching and irritation may be due to an allergic reaction to certain hygiene products or contraceptives.
For an accurate differential diagnosis and treatment prescription, you should see a physician or gynecologist who can perform the necessary laboratory tests, including a vaginal swab and urinalysis, to make an accurate diagnosis and determine the best treatment option.
Treatment
Treatment for vaginal trichomonas (trichomoniasis) is usually done with antiprotozoal drugs that can kill the Trichomonas vaginalis microorganism. The most commonly used oral antiprotozoal drug is metronidazole (sold under the trade names Metrogel, Flagyl), but tinidazole (sold under the trade names Tindamax, Fasigyn) may also be used. Treatment may be as follows:
- Oral metronidazole: Metronidazole in tablet form is usually recommended. The treatment regimen may vary, but usually the doctor will prescribe one large dose (e.g., 2 g) or short-term treatment, including taking small doses for 5-7 days. It is important to follow your doctor's instructions and complete the full course of treatment.
- Tinidazole: This is an alternative antiprotozoal drug. The treatment regimen for tinidazole may be similar to metronidazole and the dosage is determined by the doctor.
- Avoiding alcohol: Alcohol should be avoided during treatment with metronidazole or tinidazole as it can cause unpleasant side effects such as nausea and vomiting.
- Avoiding sexual contact: Av oiding sexual contact during treatment is recommended to prevent the spread of infection and re-infection.
- Partner treatment: If you have been diagnosed with vaginal trichomonas, your partner should also be treated, even if he or she has no symptoms, to prevent recurrence and spread of the infection.
- Follow-up test: After treatment is complete, it is important to have a follow-up test to make sure you are completely cured and infection-free.
If vaginal trichomonas is suspected or symptoms are present, a doctor or gynecologist should be consulted for diagnosis and appropriate treatment. Self-treatment is not recommended, as improper treatment can lead to recurrences and complications.
Treatment regimens for vaginal trichomonas
There are several treatment regimens for vaginal trichomonas (trichomoniasis) with antiprotozoal drugs such as metronidazole or tinidazole. The final regimen and dosage is prescribed by the doctor, taking into account the individual characteristics of the patient and the severity of the infection. Here are some of the typical treatment regimens:
-
Single treatment with metronidazole:
- Metronidazole: 2 g (grams) in one administration.
- Effective for many cases of trichomoniasis.
- The patient takes one large dose of metronidazole, usually the doctor prescribes this treatment in the office.
-
Short-term treatment with metronidazole:
- Metronidazole: 500 mg (milligrams) twice a day for 7 days.
- Effective in cases where a single dose is not effective or in the presence of relapses.
-
Single treatment with tinidazole:
- Tinidazole: 2 g in one administration.
- Similar to the metronidazole regimen, but tinidazole is used.
-
Short-term treatment with tinidazole:
- Tinidazole: 500 mg twice daily for 7 days.
- Effective in cases where a single dose is not effective or in the presence of relapses.
-
Treatment of pregnant women:
- Treatment of pregnant women may require caution and the regimen is prescribed by a physician taking into account the possible risks and benefits.
It is important to note that alcohol should be avoided during treatment with metronidazole or tinidazole, as it can cause unpleasant side effects such as nausea and vomiting. It is also important to complete the full course of treatment, even if symptoms have improved, to prevent recurrences.
Prevention of the vaginal trichomonas
Vaginal trichomonas prevention includes a number of activities that will help reduce the risk of contracting this infection. Here are some recommendations for prevention:
- Use condoms: Using condoms (male or female) every time you have sex can reduce the risk of transmission. Condoms provide a barrier that helps prevent contact with infected secretions.
- Afaithful and healthy sexual partner: One way to reduce the risk of infection is to make sure your sexual partner is healthy and free of infections. It is important to discuss sexual health and follow safe sexual practices.
- Regular medical check-ups: Regular medical exams and check-ups with your doctor or dentist can help detect infections early and get timely treatment.
- Personal hygiene: Good personal hygiene is important to maintain vaginal health. It is recommended to wash the external genitalia with warm water before going to bed without using scented soaps and gels.
- Avoid public bathrooms: When visiting public places where public bathrooms are used, try to avoid contact with dirty surfaces.
- Adhering to Safe Sexual Practices: Learn to adhere to safe sexual practices, including using condoms, reducing the number of sexual partners, and building trust with your partner.
- Avoid alcohol and drug use: Alcohol and drug use can decrease alertness and lead to more risky sexual behaviors. Remember that decreased self-control can increase the risk of infection.
- Antibiotic adherence: If you have received antibiotic treatment for any reason, complete the course of treatment to the end, even if symptoms have gone away. Failure to follow the course of treatment can lead to recurrences and the development of resistant bacteria.

