Medical expert of the article
New publications
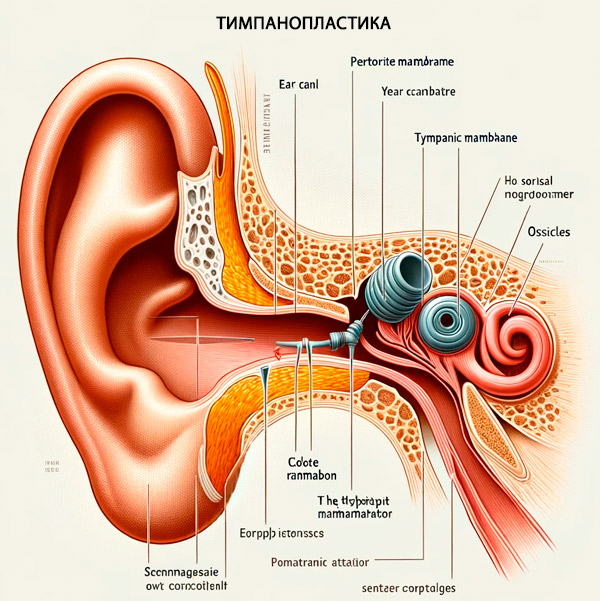
Tympanoplasty
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
In cases of damage to the tympanic membrane (membrana tympani) and dysfunction of the sound-conducting system of the middle ear located in the tympanic cavity (cavitas tympani) that do not respond to conservative treatment, they are surgically repaired - tympanoplasty, which refers to hearing-improving operations. [1], [2]
Indications for the procedure
Indications for this complex surgical procedure are: [3]
- Chronic purulent otitis media and its forms (inflammation of the mucous membrane of the middle and lower part of the tympanic cavity - mesotympanitis, as well as inflammation of the upper floor of the tympanic cavity with spread to the bony structures of the middle ear - epitympanitis) with violation of the integrity of the tympanic membrane; [4]
- Middle ear cholesteatoma of significant size, which often has a destructive effect on the membrane and the chain of the auditory ossicles; [5], [6]
- Displacement and impaired mobility of the middle ear ossicle chain due to trauma or conductive form of otosclerosis. In otosclerosis, tympanoplasty is performed with ossiculoplasty (restoration of the position of the middle ear ossicles) or their prosthesis (stapedoplasty). [7]
Tympanoplasty and myringoplasty. If there is no spontaneous healing of perforation of the tympanic membrane, restoration of its integrity - in the absence of disorders of the sound-conducting system of the middle ear - is performed by myringoplasty (from New Latin myringa - tympanic membrane; the term was introduced into the medical lexicon at the end of the 16th century by the famous Italian anatomist and surgeon Hieronymus Fabricius). And this is tympanoplasty of the tympanic membrane type 1 (see below about the types of this operation). [8]
Preparation
In preparation for surgery, patients undergo blood tests (general, biochemical, coagulation and RW); audiometry of hearing and tympanometry; [9] a CT scan of the ear and temporal bone; and an ECG.
At least one week before the scheduled surgery, stop taking anticoagulants (drugs that reduce blood clotting) and NSAIDs.
The choice of anesthesia in this type of surgery - general anesthesia or local anesthesia with standard sedation - depends on the scope of the intervention and its complexity. In most cases, general endotracheal anesthesia, i.e. Anesthesia, is used.
Technique of the tympanoplasty
The approach and specific technique of operations to restore the tympanic membrane and the sound conducting system depend on the size and location of the perforation, the cause of the pathology, the presence and degree of damage to the middle ear structures, anatomical features of the external auditory canal, etc. [10]
Some surgeries can be performed through the ear canal - transmeatal access (allowing for less invasive endoscopic intervention), but more often, to allow greater access to the middle ear and mastoid, an incision in front of the ear, called an endaural access, or behind the ear, called a retroauricular access, is required. [11]
Special microsurgical instruments and operating binocular microscopes are used for such operations, diamond burrs are used for bone drilling.
Autologous tissue is used as a transplantation material to close tympanic membrane perforations: fascia of the temporalis muscle (obtained through a small incision approximately 2-3 mm behind the upper part of the auricular sulcus), epicondyle of the auricle or tympanomeatal flap - a surgically created flap of tissue consisting of a segment of the ear canal skin and the attached tympanic membrane, which are lifted into the middle ear cavity. Allografts may also be used. [12], [13]
Autologous grafts for tympanic membrane defect closure are usually placed by the lining technique with additional fixation on the bony ear canal or by the overlay technique, placing the graft between the fibrous layer of the membrane and the raised epidermis of its outer layer. [14]
Wulstein tympanoplasty implies the choice of a type of surgical intervention that makes maximum use of the functioning structures of the sound conducting apparatus of the middle ear, and in case of their partial or complete loss - reconstruction of the auditory ossicles (malleus, incus and stapes) and the tympanic membrane using various materials. Various types of otologic prostheses are now used to replace the auditory ossicles. [15]
In the mid-1950s, German otosurgeon Horst Ludwig Wulstein (1906-1987), who is considered the founder of modern ear microsurgery, proposed the main types of tympanoplasty, which are constantly being improved by specialists in surgical otiatrics. [16]
Type 1 tympanoplasty - myringoplasty with transmeatal access - is indicated in the absence of damage to the auditory ossicle chain. The surgery recreates the almost natural size and shape of the middle ear cavity.
Type 2 tympanoplasty is performed in cases of perforation of the tympanic membrane with erosion of the bony malleolus; the membrane graft is fused to the anvil or the remains of the malleolus.
Type 3 tympanoplasty is used when the integrity of the tympanic membrane is compromised and the two auditory ossicles are destroyed - with an intact and mobile stapes to which the graft is fixed. It shortens the chain of the auditory ossicles somewhat, but eliminates its interruption.
Type 4 tympanoplasty may be performed if all or part of the stapes of the stapes has been affected by the destruction of the auditory ossicles; the tympanic membrane defect is closed with the preserved tense part (pars tensa) or with a free flap that is connected to the stapes foot at the edge of the open oval window of the cochlea.
Type 5 tympanoplasty involves not only placing a membrane graft and connecting the auditory ossicles to the anterior labyrinth ladder, but also creating a new oval window separating the labyrinth from the middle ear. However, this type of surgery is appropriate only in cases of ankylosis (immobility) of the stapes.
In chronic purulent otitis media, as well as in case of mastoiditis that develops against the background of its exacerbation to remove purulent exudate from the middle ear (or cells of the mastoid process), a sanitizing operation with tympanoplasty can be performed. This is a so-called separate atticoanthrotomy with tympanoplasty of type 1 - myringoplasty, during which the suprabasal space (epitympanum or attic) is opened with the removal of its outer wall, as well as the opening of the mastoid cavity (mastoid antrum).
At the end of all types of tympanoplasty, all incisions are sutured layer by layer and the skin is sutured intradermally with absorbable chrome catgut. A steri-strip patch may also be applied to the incision site. Spongy postoperative Merozel swabs impregnated with suspension (antibiotic Ciprofloxacin + corticosteroid Dexamethasone) are placed in the ear canal. Then a firm compressive dressing is applied for 24 hours.
Contraindications to the procedure
Specialists refer to contraindications to tympanolastics: [17]
- Otorrhea (the presence of active discharge from the middle ear);
- Acute otitis externa or otitis media;
- Lack of hearing in the other ear;
- Obstruction of the eustachian (auditory) tubes of any etiology;
- Dysfunction of the cochlea;
- Damage to the auditory nerve;
- Presence of inflammatory process of any localization;
- Uncontrolled allergic rhinitis;
- Exacerbations of chronic diseases;
- Bleeding.
These surgeries are not performed on children under the age of three.
Consequences after the procedure
After almost any surgical intervention, patients feel pain of varying intensity, and pain after tympanoplasty doctors recommend that pain after tympanoplasty be managed with simple painkillers, such as Paracetamol or Ibuprofen.
These same remedies will help if your ear hurts after tympanoplasty, and it may hurt for one to two weeks; there may also be mild pain in the temple or when chewing.
In the first two weeks after surgery, you may experience a small bloody or watery discharge from the ear and swelling in the ear area.
Tinnitus after tympanoplasty (due to blockage in the middle or outer ear) can be felt even by patients who did not complain about it before the operation. This also applies to those who have ear stuffiness after tympanoplasty. As the ear heals, this will go away on its own.
In addition, patients may feel numbness in the upper part of the ear, but it goes away about three months after surgery. [18]
Complications after the procedure
Among the possible complications of this surgical intervention are noted: [19]
- Rejection of a membrane graft and/or otologic prosthesis;
- Formation of adhesions between the graft and the cape of the cochlea;
- Blunting of the anterior tympanomeatal angle due to the formation of excessive fibrous tissue, which reduces the transmission function of the middle ear;
- Deterioration of hearing, progressing to hearing loss;
- Damage to the facial nerve or its parasympathetic branch (tympanic string) leading to paralysis of mimic muscles - with taste disturbance;
- Damage to the structures of the labyrinth (inner ear) causing vertigo after tympanoplasty;
Chills and fever after tympanoplasty, as well as purulent discharge from the ear are signs of infectious inflammation.
Severe headache after tympanoplasty, fever above +38℃, nausea and vomiting, as well as neck stiffness and pain in the eyes when looking at the light means inflammation of the cerebral membrane - bacterial meningitis (which can develop in the first 10-14 days after surgery).
Care after the procedure
During healing, the ear must be protected by bandages that fill the ear canal and only the doctor can authorize their removal. The dressings on the outer sutures should remain in place for seven to ten days.
Proper ear care after tympanoplasty is very important. First, the ear must be kept dry: the swab covering the external ear canal can be changed as needed, and initially this may be three to four times a day. For two to three weeks after surgery, drops (Ciloxan, Ciprodex or other antibacterial drops prescribed by the doctor) are injected twice a day (5 drops each) onto the swab in the ear canal.
The swab is removed from the canal two weeks after surgery, and the drops continue to be applied twice a day for another two weeks.
Oral antibiotics are also prescribed: Amoxicilin (Augmentin) or Cephalexin (Cefazolin) - one tablet twice a day for 10 days.
To reduce pressure on the operated ear and swelling, it is recommended to rest sitting or semi-reclining at a 45° angle.
What should not be done after tympanoplasty? You should not: blow your nose hard, sneeze with your mouth closed and cough; take a bath, swim or dive in swimming pools and natural water bodies.
For at least six months, increased physical activity and sports are excluded after tympanoplasty. Alcohol is absolutely prohibited after tympanoplasty.
Air travel after tympanoplasty should be postponed for at least three to four months (and in consultation with your doctor).
Patients are interested in how to wash their hair after tympanoplasty. Since the ingress of water into the ear is absolutely inadmissible, when showering or washing hair, the external ear canal should be closed with a cotton swab smeared with petroleum jelly.
But what patients are most interested in is how long after tympanoplasty their hearing will improve. According to otosurgeons, the timing and degree of hearing improvement depends on many factors, including the reasons that led to the need for the surgery, the type of surgery, the presence of complications, and more. The fastest improvement in hearing is near normal after myringoplasty, which is a type 1 tympanoplasty.

