Medical expert of the article
New publications
Trophic ulcers in diabetes mellitus on the legs
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.

Why is diabetes often accompanied by the formation of ulcers on the body, and why is it so difficult to get rid of them? There are indeed many questions about the formation of ulcers in diabetes, which medicine is quite capable of explaining.
Diabetes is a complex disease that manifests itself not only by an increase in sugar levels. The function of many organs is disrupted, the innervation and trophism of the skin deteriorates. Unfortunately, this process is difficult to treat and can occur again in the same place.
Epidemiology
Ulcers are the most common diabetic complication, accounting for about a third of hospitalizations in patients with diabetes.
In approximately every second patient, ulcers lead to amputation of a limb (or pair of limbs).
According to statistics, ulcerative tissue damage is registered in 80% of diabetics with a 15-20-year history of the disease. In this case, two out of three patients die from gangrenous complications.
About 40% of patients after the operation lose the ability to move, or are severely limited in their movement. In about 60% of cases, purulent necrotic consequences occur on the other limb, so such patients have to have the other leg amputated as well.
Gangrenous complications of ulcers in diabetes occur 40 times more often than in people without diabetes. In 85% of patients, foot ulcers lead to amputation.
The cause of the development of ulcerative lesions in diabetes in 4 cases out of 5 is external mechanical damage.
Causes of diabetic ulcers
In people suffering from diabetes, the main disorder is considered to be a disrupted mechanism of carbohydrate metabolism - both in blood cells and in the cellular structures of the entire body. In some cases, such a disorder does not manifest itself in any way until either signs of diabetes or another secondary disease (which many do not associate with diabetes) appear. Such a secondary pathology can be a stroke, acute heart attack, a sharp deterioration in visual function, the development of renal failure. Ulcers are most often found in patients with type 2 diabetes - most likely due to the fact that this type of disease can proceed for a long time without any symptoms, at a time when metabolic processes in tissues are already disrupted.
Doctors point to another important reason for the formation of ulcers in diabetes - this is the patient's inattention and ignoring the advice of doctors to change their diet and lifestyle. Unfortunately, many patients continue to smoke and drink alcohol, despite the doctor's requirement to eliminate bad habits from their lives.
Individual risk factors also play a significant role.
Risk factors
- Mechanical injuries to the skin (abrasions, cracks, burns, etc.).
- Varicose veins, other vascular diseases.
- Wearing poor quality or uncomfortable shoes.
- Impaired lymph flow in the extremities.
- Atherosclerotic changes in blood vessels, hypertension.
- Bedsores, prolonged wearing of bandages, including plaster ones.
- Long-term intoxication, ketoacidosis, liver and kidney disease.
- Failure to follow the doctor's recommendations on nutrition for diabetes, the presence of bad habits.
Pathogenesis
Pathogenetic characteristics of ulcers in diabetes are varied. The essence is as follows: diabetes is a complex metabolic pathology, which is accompanied by a failure of insulin sensitivity and production. Type 1 diabetes occurs with impaired insulin production. For type 2 diabetes, this symptom is not typical, but insulin sensitivity is impaired, which leads to its incorrect use by the body.
Insulin is an essential protein hormone that is directly involved in the processes of glucose absorption and transformation. If tissues perceive insulin incorrectly, a series of disorders will begin – in particular, the level of glucose in the bloodstream will increase. This, in turn, entails the development of neurovascular changes.
Doctors describe the changes mentioned in different terms. Thus, damage to neurons in diabetes is called "diabetic neuropathy", and changes in the smallest vessels are called diabetic angiopathy. Both the first and second pathologies are a consequence of a systemic failure of metabolic processes.
First of all, the disorders concern the vascular walls, which become thin and fragile. The capillaries become clogged, and large vessels are gradually affected by atherosclerosis. However, ulcers in diabetes do not appear in all patients, but primarily in those who ignore treatment, do not listen to medical recommendations and do not control blood glucose levels. The fact is that ulcers do not appear "out of the blue": their appearance must be preceded by high sugar levels and a state of ketoacidosis.
The formation of an ulcer in most cases is combined with the appearance of eczema or dermatitis. If left untreated, the ulcerous lesion increases in size and can even develop into gangrene.
Symptoms of diabetic ulcers
Ulcers are one of the common complications of diabetes, which develop after a certain period of time after the onset of the disease. For example, with decompensated diabetes, ulcers can form within a year.
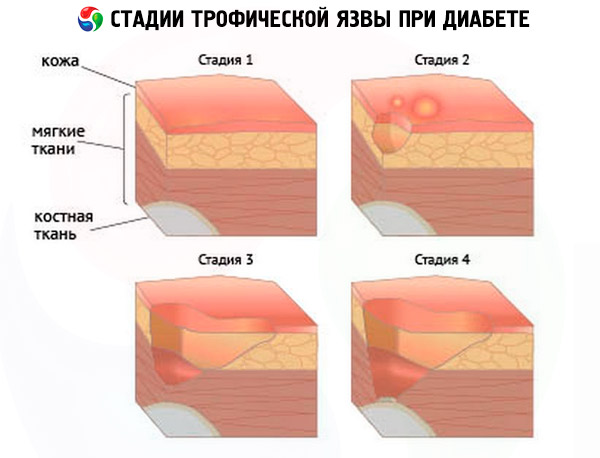
Medical experts have determined a conditional classification of the appearance of ulcers - these are a kind of stages of the disease, which are characterized by a separate set of symptoms:
- Pre-ulcer stage, when ulcers are already beginning to form, but this remains barely noticeable to the patient. The first signs of the initial stage may be as follows:
- decreased receptor sensitivity (sensitivity to pain and temperature worsens);
- the appearance of barely perceptible pain in the ankle area, as well as a feeling of mild burning and/or itching;
- the appearance of minor cramps in the ankle area;
- swelling of the extremities (to varying degrees);
- change in skin color, increased pigmentation, redness or blueness, appearance of vascular patterns.
- Initial clinical stage – at this stage the patient already pays attention to the first signs, but does not always consider it necessary to consult a doctor. Although it is at this stage that treatment can lead to the most positive prognosis. The first signs of the second stage are as follows:
- the appearance of minor skin defects, erosions;
- formation of ulcers that are difficult to heal.
- Stage of obvious clinical symptoms:
- destruction of the upper layers of the skin, formation of crusts on ulcers;
- the appearance of bloody discharge, then purulent;
- increase in the size of ulcerative lesions;
- the appearance of other lesions, varying in size and depth of damage.
- Progressive stage:
- transformation of small trophic ulcers into a purulent infected focus;
- the appearance of intoxication (temperature rises, fever, headache, weakness are observed);
- worsening leg pain;
- damage to deep tissues (down to the bone).
- Gangrenous stage – accompanied by the development of wet gangrene of part of the limb.
Like any injury, an ulcer in diabetes is accompanied by pain, but at an early stage this pain may be weakly expressed, even almost unnoticeable. As the process worsens, the symptoms are especially evident at night: there is a sensation of itching, cramps, the limbs seem to "fill up".
What do ulcers look like in diabetes?
At first, small wounds, scratches, abrasions may appear on the skin - if the formation of an ulcer in diabetes is preceded by mechanical damage. Then the wounds begin to bleed and increase in size over time. When the wounds become infected, an external infectious and inflammatory process develops: the discharge becomes purulent, and the tissues around the lesion swell and turn red.
The ulcerative lesion grows, but at first the patient does not feel pain – this is the result of impaired innervation in the tissues.
An ulcer in diabetes is almost impossible to treat with conventional methods, which is also a typical symptom of the disease.
Forms
Different types of ulcers in diabetes require different approaches to treatment. Of course, any trophic ulcer in diabetes occurs as a result of damage to the small capillary network and nerve fibers, but each individual type has its own features and characteristics that are taken into account by the doctor when determining the treatment regimen. Thus, ulcers of the lower extremities are divided into the following types:
- Capillary ulcer of the foot in diabetes mellitus develops due to damage to the capillary network. This type of pathology is diagnosed most often.
- Venous leg ulcers in diabetes are caused by a disorder of the venous system. As a rule, venous ulcers are found in patients who have not sought medical help for a long time and have not treated diabetes, or have treated it incorrectly. In such a situation, the ulcer initially does not appear on the foot or toe, but affects the area of the leg, or becomes a consequence of the growth of the necrotic process.
- Arterial ulcers on the legs in diabetes are formed when the arterial lumen is blocked, which often happens with blood clotting disorders and atherosclerosis. Such a disorder causes rapid tissue necrosis localized below the affected section of the artery.
- Pyogenic ulcer in diabetes is a consequence of microbial infection of small wounds and scratches on the skin.
Some types of ulcers are found more often in diabetes, while others are less common. For example, ulcers of the foot and lower leg are most often diagnosed.
Heel ulcers in diabetes are also quite common, and in the vast majority of cases they form due to long-standing heel cracks, calluses, or after a heel puncture with a hard and sharp object. Sometimes a diabetic can develop an ulcer even after an ordinary splinter.
An ulcer on a finger in diabetes occurs when wearing uncomfortable shoes, when abrasions, blisters, etc. appear. Such lesions are quite difficult to treat, and often end in surgery to remove one or more fingers.
A gastric ulcer in diabetes mellitus does not belong to the category of typical trophic lesions of the disease. Rather, it is a concomitant pathology. Trophic ulcers characteristic of diabetes are formed in the area with impaired innervation - as a rule, on the lower extremities. However, the presence of a gastric ulcer against the background of diabetes requires particularly complex treatment and adherence to an appropriate diet.
Ulcers on the hands in diabetes, as well as on the body or head, are formed extremely rarely. Only in isolated cases can an ulcer form after significant traumatic injury - for example, after a burn, lacerated wound, open fracture, etc. Due to physiological characteristics, the vascular network of the lower extremities is more susceptible to pathological changes than the vessels of the arms. Therefore, the legs are affected first. But - there are exceptions, and this must be taken into account when diagnosing an ulcer.
Complications and consequences
Ulcers themselves are a complication of diabetes, but skin wounds can also become complicated - especially when secondary infections occur.
The consequences of ulcers in diabetes include the following complications:
- erysipelas - erysipelas - is a microbial skin infection that is accompanied by severe intoxication (streptococcal tissue damage);
- secondary inflammatory process in the lymph nodes, lymphatic vessels – indicates the spread of infection;
- sepsis (general intoxication against the background of the development of gangrene).
The severity of complications depends on the course of the underlying pathology, the duration and depth of the trophic disorder, and the type of trophic disorder. Many patients have to amputate part of the limb, or the entire limb - this happens when the disease process is advanced.
As a result of self-medication or improper treatment of ulcers in diabetes, other problems often arise:
- skin diseases such as eczema or dermatitis;
- damage to a vessel with subsequent bleeding;
- development of anaerobic infection, tetanus;
- joint damage;
- Myiasis is a parasitic disease.
Ulcers in diabetes require serious attention. Any patient should be aware that ignoring the doctor's recommendations can lead to disastrous consequences, disability and even death.
Diagnostics of diabetic ulcers
First of all, the doctor pays attention to the patient's complaints. If, against the background of diabetes, a person periodically experiences numbness in the legs, increased fatigue, swelling, hyperpigmentation, then certain conclusions can already be made regarding the diagnosis.
An external examination of the patient is also mandatory. In addition to the characteristic features of the ulcer itself, deformation of the foot, ankle, neuroosteoarthropathy can be detected. The quality of temperature, tactile, proprioceptive, pain, vibration sensitivity is determined using tests. Tendon reflexes are checked.
During the examination, attention is also paid to the skin color, swelling, and the presence of joint pathology. Particular attention is paid to the size and location of the ulcer, the nature of the discharge, the clarity of the edges, and the condition of healthy skin.
The following tests are mandatory:
- general analysis and blood biochemistry (indicate the presence of inflammation, allow to assess the quality of the blood clotting function);
- general urine analysis (indicates changes in renal function);
- Blood glucose level test.
Instrumental diagnostics includes radiocontrast arteriography, Doppler examination of arterial circulation, and computer capillaroscopy.
Often the diagnostic program includes rheolymphovasography, thermal imaging, and impedancemetry.
Differential diagnosis
Differential diagnostics are carried out with collagenoses, blood diseases, professional intoxications. The following diseases are subject to separate differentiation:
- obliterating atherosclerosis;
- phagedenic ulcer;
- congestive ulcers (a consequence of decompensation of the cardiovascular system);
- tuberculous ulcers, syphilitic ulcers, leprosy ulcers, radiation ulcers.
Rarely, patients are found to have so-called artificial ulcers, or artificial ones. The patient inflicts them on himself, for the purpose of simulation - as a rule, such ulcers indicate mental instability of the patient.
Who to contact?
Treatment of diabetic ulcers
Local treatment of trophic ulcers in diabetes includes systematic cleaning of the ulcer, treatment of the skin near the wound, regular dressings. The possibility of using ointments is agreed with the attending physician. Read more about the methods of treating ulcers in diabetes in this article.
Prevention
The main condition for preventing ulcers is following the recommendations of the attending physician. Such recommendations are necessarily voiced to all patients suffering from diabetes.
Ulcers can occur in any diabetic if he/she does not pay due attention to constant control of blood sugar levels. Therefore, prevention, first of all, consists of normalizing sugar levels and conducting maintenance therapy for diabetes.
Other equally important tips for preventing ulcers:
- It is necessary to maintain careful foot hygiene, cut your nails promptly and correctly, and prevent the development of fungal infections.
- It is important to clean, dry and air your shoes as often as possible – this is an important condition for healthy feet.
- When choosing shoes and socks, you should pay special attention to their quality and size to avoid the appearance of abrasions, blisters, and calluses on your feet.
- It is necessary, if possible, to avoid overheating and excessive cooling of the legs, and also not to overexert them.
- Regularly - for example, every evening, it is advisable to inspect the feet, toes, ankles. Particular attention should be paid to the presence of external damage, punctures, splinters. With diabetes, even such minor injuries can cause the formation of ulcers.
Forecast
The further outcome of the disease depends on the extent to which the underlying pathology - diabetes mellitus - will worsen, as well as on how seriously the patient will take the doctor's recommendations. If the patient is diagnosed with an isolated neuropathic type of ulcer, provided that timely and adequate therapy is carried out, the prognosis can be considered relatively favorable.
If diabetes is severe, with increasing vascular disorders, then in such a situation it is impossible to talk about an optimistic prognosis.
Ulcers in diabetes are difficult to treat. But: the sooner you pay attention to the problem, the sooner the therapy is prescribed - the more likely it is that the patient's condition will normalize.


 [
[