Medical expert of the article
New publications
Rheumatoid arthritis treatment and leg pain relief
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Today, the goal of treating rheumatoid arthritis, which causes severe leg pain, is to reduce joint inflammation and pain. Another goal is to maximize joint function and prevent joint deterioration and deformity. The sooner a person begins treating arthritis, the more success they will have. Aggressive pain management can improve joint function, stop joint damage, and reduce leg pain. How can this be done?
The challenge of optimal arthritis treatment
Optimal treatment of the joints of the legs from this disease includes a combination of medications, rest, exercises to strengthen the muscles, joints and ligaments, their protection, and information about this disease for the patient. Treatment depends on the general health, age of the patients and their physical activity. Treatment is most successful if the patient and doctor cooperate with each other.
At least two classes of drugs are used in the treatment of rheumatoid arthritis: first-line drugs that act quickly, and second-line drugs that act slowly. They are better known as pain-modifying antirheumatic drugs.
The so-called first-line drugs are cortisone and aspirin (corticosteroids), which doctors use to reduce inflammation and pain in the legs. The so-called second-line drugs are designed to promote remission of arthritis and can prevent aggressive destruction of joints.
The extent of joint destruction in the legs in rheumatoid arthritis varies depending on the overall condition of the affected individuals. Those who suffer from less destructive forms of the disease can manage leg pain. With early treatment, leg function improves and the risk of disability, as well as joint destruction in the legs, is minimized. But this is provided that the person has previously been treated with second-line drugs (pain-modifying antirheumatic drugs).
Most people require more aggressive second-line drugs, such as methotrexate, and also need anti-inflammatory drugs in combination. Sometimes these second-line drugs are used in combination. In some cases, they counteract severe deformity of the joints of the legs, and then surgery may be necessary.
"First Line" Drugs for Rheumatoid Arthritis
Acetyl salicylate (aspirin), naproxen (Paracetamol), etodolac (Lodine) and ibuprofen are examples of nonsteroidal anti-inflammatory drugs (NSAIDs). They are drugs that can reduce tissue inflammation, pain and swelling in the legs in rheumatoid arthritis. Aspirin in doses higher than those people take to treat headaches and fevers are effective anti-inflammatory drugs for treating leg joints in rheumatoid arthritis.
Aspirin has been used to treat and improve joint health since ancient Egyptian times. Newer NSAIDs are as effective as aspirin at reducing inflammation and pain, and require much lower daily doses. Patients' responses to different NSAID drugs vary. Thus, it is not unusual for a physician to try several NSAID drugs to identify the most effective agents with the fewest side effects.
Coping with drug side effects
The most common side effects of aspirin and other NSAIDs can include gastrointestinal upset, abdominal pain, ulcer flare-ups, and even gastrointestinal bleeding. To reduce gastrointestinal side effects, NSAIDs are usually taken with food.
Additional medications are often recommended to protect the stomach from ulcers. These oral medications include antacids, sucralfate (Carafate), inhibitors (Prevacid, etc.), imisoprostol (Cytotec). Newer agents - selective NSAIDs - may include inhibitors, such as celecoxib (Celebrex), which fight inflammation, but with less risk of irritation of the stomach wall and risk of bleeding.
Corticosteroid drugs
Corticosteroids can be taken orally or injected directly into the tissues and joints. They are more powerful than NSAIDs in reducing inflammation and in restoring joint mobility and function in the legs. Corticosteroids are useful for short periods during severe flare-ups of disease activity or when the body does not respond to NSAIDs. However, corticosteroids can have significant side effects, especially when given in high doses over a long period.
These side effects of arthritis include weight gain, facial swelling, thinning of the skin and bones, bruising even with minor injuries, cataracts, risk of infection, muscle atrophy in the legs, and destruction of large joints such as the hips. Corticosteroids (not all!) may also increase the risk of infection. These side effects can be partially avoided by gradually reducing the dose of corticosteroids.
Abruptly stopping corticosteroids for rheumatoid arthritis may result in flare-ups or other symptoms – so abruptly stopping corticosteroids is not recommended. Thinning of bones due to osteoporosis can be prevented by taking calcium and vitamin D supplements.
 [ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
[ 5 ], [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ]
Second line drugs
"Second-line" or slow-release medications for rheumatoid arthritis (pain-modifying antirheumatic drugs) "First-line" drugs (NSAIDs and corticosteroids) can reduce joint inflammation and pain, but they cannot necessarily prevent joint destruction and changes - deformity.
Rheumatoid arthritis requires medications other than the NSAIDs and corticosteroids recommended by your doctor to stop the active damage to bone, cartilage and surrounding soft tissue. The medications needed to effectively treat this disease and the leg pain associated with it come in many forms. These are the aforementioned "second-line" or "slow-release" medications that may take months or weeks to work effectively in a complex treatment. They are used for quite a long period of time, even years, and in varying doses.
The most effective drugs can promote remission, thereby slowing down the progressive destruction of joints and their deformation. Sometimes all the second-line drugs are used together, and this is a good combination therapy for arthritic joints of the legs. As in the first line, the doctor can try different second-line drugs, then the treatment is optimal.
Peculiarities
Recent studies have shown that patients who respond to slow-release medications to control rheumatoid arthritis may actually reduce the small but real risk of developing lymphoma (cancer of the lymph nodes) that sometimes plagues patients with rheumatoid arthritis.
Hydroxychloroquine (Plaquenil) is used to treat malaria. It has been used to treat rheumatoid arthritis for quite some time. Possible side effects of this drug include muscle weakness in the legs and arms, stomach upset, skin rashes, and changes in the joint structure of the legs.
Changes in vision are rare, people taking this drug should see an ophthalmologist for monitoring.
Sulfasalazine (Azulfidine)
It is an oral medication that is traditionally used to treat mild to moderate inflammatory bowel conditions, such as ulcerative colitis and Crohn's disease colitis. Sulfasalazine is also used to relieve symptoms of rheumatoid arthritis, but it must be combined with anti-inflammatory drugs. Sulfasalazine is generally well tolerated. However, side effects include rash and upset stomach.
Since Sulfasalazine is made up of sulfur compounds and salicylic acid, it should be avoided by people with allergies to sulfur-containing drugs. Methotrexate is very popular among doctors as a second-line drug because it is effective and has few side effects. It also has the advantage of flexible dosage (they can be adjusted depending on the needs of the person). Methotrexate is an immunosuppressant drug. It can affect the bone marrow and liver, and rarely causes cirrhosis of the liver. All people taking methotrexate need regular blood tests to monitor their blood and liver function.
 [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
[ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ]
Gold Salts for Treating Arthritis and Leg Pain
Gold salts have been used to treat the symptoms of rheumatoid arthritis for many decades in the last century. Sodium aurothiomalate (water-soluble) and aurothioglucose, a gold suspension, are given by injection every week for several months and up to several years. Auranofin, an oral drug for the treatment of rheumatoid arthritis and pain in the legs, was introduced in 1980. It is much better tolerated than previous drugs, but acts on the body a little more slowly.
Side effects of gold preparations (oral and taken orally) include skin rashes, mouth ulcers, kidney damage with protein in the urine, and possible bone marrow damage if anemia and low white blood cell counts are present. People treated with gold salts should have regular blood monitoring and urine tests. Oral gold may cause diarrhea. These gold remedies have fallen out of favor with arthritis patients due to the availability of more effective treatments.
Immunosuppressive drugs
D-penicillamine may be useful in some cases of progressive types of rheumatoid arthritis. Its side effects are similar to those experienced by patients with gold medications. These side effects include chills, fever, mouth sores, skin rashes, metallic taste in the mouth, kidney and bone marrow problems, stomach upset, and joint pain, particularly in the legs. People taking this drug need to have their urine and blood tests monitored. D-penicillamine may rarely cause symptoms of other autoimmune diseases, and it is not often recommended for rheumatoid arthritis.
Immunosuppressive drugs are powerful drugs that suppress the immune system. Immunosuppressive drugs are used successfully to relieve the symptoms of rheumatoid arthritis, particularly leg pain. They include methotrexate, as well as azathioprine (Imuran), cyclophosphamide (Cytoxan), as well as cyclosporine (Sandimmune) and chlorambucil (Leukeran). Because of their serious side effects, immunosuppressive drugs (other than methotrexate) are generally recommended for those who have very aggressive disease or rheumatoid arthritis with serious complications, such as vasculitis - inflammation of the blood vessels.
An exception is a drug such as methotrexate, which is often associated with complex side effects and its content must be checked in the blood. Methotrexate is preferred as a second-line drug for a quality result.
Immunosuppressant drugs
Immunosuppressant drugs can suppress bone marrow function and cause anemia, as well as low white blood cell counts, and this condition is also associated with low platelet counts. Low white blood cell counts can increase the risk of infections in the body, while low platelet counts can increase the risk of bleeding.
The drug Methotrexate can sometimes cause cirrhosis of the liver, as described above, and cause allergic reactions in the lungs. Cyclosporine can cause kidney damage and high blood pressure. Because of the potentially serious side effects, immunosuppressive drugs are used in low doses, usually in combination with effective anti-inflammatory drugs.
New Treatments for Rheumatoid Arthritis
New "second-line" drugs for reducing the symptoms of rheumatoid arthritis may include leflunomide (Arava) and tocilizumab. Each of these drugs may increase the risk of infections and the development of infections, information that should be conveyed to patients when taking these new second-line drugs. Leflunomide is available to relieve symptoms of leg pain and stop the progression of arthritis.
This is similar to blocking the body's action on a very important enzyme that plays a role in activating the immune system. Arava may cause hair loss, kidney disease, liver disease, diarrhea, and/or rash in some people. This drug should not be taken immediately during or before pregnancy due to possible birth defects, and should be avoided by women planning to become pregnant.
Medicines that represent a new approach to the treatment of rheumatoid arthritis are products of modern science - biotechnology. They are referred to in the literature as biological agents or powerful biological response modifiers. Compared with traditional arthritis drugs, powerful biological drugs act on the body much faster and can have a strong effect at the stage of progressive joint damage. In general, the methods of action of biological agents are more targeted, more defined with the degree of impact than traditional arthritis drugs.
Biological drugs
Etanercept, infliximab, adalimumab are biological drugs that are able to intercept protein agents in inflamed joints (tumor necrosis factor), which contributes to the occurrence of joint inflammation in the developed rheumatoid arthritis. These TNF blockers are able to intercept the protein before affecting the natural receptor, which is able to "turn on" the inflammation process. This effectively blocks inflammation provocateurs from inflammatory cells.
Symptoms – pain, swelling and other symptoms that indicate unhealthy legs can be quickly reduced in people who use these drugs. Etanercept is injected subcutaneously 1-2 times a week. Infliximab is an injection that is given directly into a vein (the drug is injected intravenously).
Adalimumab is administered subcutaneously once every two weeks or once every week. Golimumab is administered subcutaneously every month. Certolizumab pegol is administered with a needle under the skin every 2-4 weeks. Each of these medications is currently being evaluated by doctors only in practice so that doctors can determine what role these drugs can play in the treatment of patients at different stages and in different forms of rheumatoid arthritis. Research in recent years has shown that biological response modifiers and prevent progressive joint destruction in rheumatoid arthritis.
 [ 16 ]
[ 16 ]
Biological response modifiers
They are currently recommended for use after second-line drugs have failed. Biological response modifiers (TNF inhibitors) are expensive. They are often used in combination with methotrexate and other DMARDs. It should also be noted that TNF blocking biologics are increasingly being used in combination with methotrexate.
These medications should be avoided by people with significant heart congestion, heart failure, or demyelinating diseases (such as multiple sclerosis ) because they may worsen the person's condition. Anakinra (Kineret) is another biologic drug that is used for the ongoing treatment of moderate to severe forms of rheumatoid arthritis.
Anakinra works by binding to a protein on cells (proinflammatory cytokines). Anakinra is injected under the skin daily. Anakinra can be used alone or with other DMARDs. Anakinra does not work as quickly as other biologics.
Rituximab
Rituximab (Rituxan) is a type of antibody that was first used to treat lymphoma, a cancer of the lymph nodes. Rituximab may be effective in treating autoimmune diseases such as rheumatoid arthritis because it depletes B cells, which are important in killing inflammatory cells and in producing abnormal antibodies. Rituximab helps treat moderate to active rheumatoid arthritis in patients who have failed TNF-blocking biologics.
Preliminary studies have shown that rituximab has been used to be useful in treating severe forms of rheumatoid arthritis that are complicated by severe inflammation of the blood vessels (aka vasculitis) and cryoglobulinemia. Rituximab is given as an intravenous infusion in two divided doses over a two-week period about every six months.
Abatacept
Abatacept (Orencia) is a potent biologic drug that blocks active T cells. Abatacept is used to treat arthritis in adults who are not treated with traditional DMARDs. Abatacept is given as an intravenous infusion over a month.
Tocilizumab
Tocilizumab (Actemra) was recently approved for the treatment of adult patients with moderate to severely active rheumatoid arthritis (RA). Tocilizumab is the first approved biologic drug that can block interleukin-6 (IL-6), which is a chemical agent of inflammation in the acute form of rheumatoid arthritis.
Tocilizumab is a drug given intravenously for a month. Biologics are often used in combination with traditional drugs in the treatment of rheumatoid arthritis, they are generally not used with other biologics because the risk of serious infections is unacceptable.
Prosorba preparation
Prosorba is used to reduce or relieve symptoms of moderate to severe rheumatoid arthritis pain in adults with long-standing rheumatoid arthritis who have failed to recover from or who are intolerant to antirheumatic pain-modifying drugs (DMARDs). The exact role of this treatment is poorly understood by physicians today and it is not commonly used today.
Rheumatoid Arthritis, Pregnancy and Leg Pain
Rheumatoid arthritis often resolves or reduces symptoms as pregnancy progresses. As pregnancy progresses, rheumatoid arthritis joint inflammation and leg pain tend to decrease and be minimal during pregnancy. Unfortunately, this reduction in pregnancy joint inflammation and leg pain is not sustained after delivery.
Medicines commonly used to treat severe inflammation of the joints of the legs, such as nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen (Motrin, Advil), naproxen (Aleve), and others, should not be used during pregnancy. Medicines used to stop the progression of rheumatoid arthritis, such as methotrexate and cyclosporine (Neoral, Sandimmune), should not be used during pregnancy and should be stopped well before conception because of the potential risk to the fetus. Biologic medications for leg pain due to rheumatoid arthritis should not be used during pregnancy.
For rheumatoid arthritis that is active during pregnancy, steroid medications such as prednisone and prednisolone are often used to relieve leg pain to calm the joint inflammation. These medications do not have any negative effects on the fetus.
Diet and other arthritis treatments to relieve leg pain
Doctors say there is no special diet to treat the symptoms of rheumatoid arthritis. A century ago, such diets were advertised as avoiding foods such as tomatoes that aggravate the symptoms of rheumatoid arthritis. This is no longer accepted as true. Fish oil has been advertised as helpful in some short-term studies of rheumatoid arthritis.
The benefits of medications for relieving the symptoms of rheumatoid arthritis remain unproven. Symptomatic pain relief can often be achieved with oral acetaminophen (Tylenol) - a topical preparation that is rubbed into the skin. Antibiotics, particularly tetracycline, minocycline (Minocin), have been tried for relieving the symptoms of rheumatoid arthritis in recent clinical trials. Early results have shown mild to moderate improvement in arthritis symptoms.
Minocycline appears to inhibit the development of important enzymes that mediate tissue destruction, called metalloproteinases.
Diseases of the legs, other than tissues affected by rheumatoid inflammation, are considered on an individual basis.
 [ 19 ], [ 20 ], [ 21 ], [ 22 ]
[ 19 ], [ 20 ], [ 21 ], [ 22 ]
Exercises for joint mobility in the legs with arthritis
Regular exercise, done correctly, is essential to maintain joint mobility and strengthen the muscles around the painful joints of the legs in arthritis. In these circumstances, a swimming pool is especially useful because it allows you to perform exercises with minimal stress on the joints. Professional therapists can offer support in physical exercise to restore the joints of the legs.
For example, joint mobility exercises for the feet and toes can be helpful in reducing inflammation and maintaining alignment of misaligned joints. Devices such as canes and crutches can help with daily living. Alternating heat and cold on the feet are conditions that can help relieve symptoms before and after exercise.
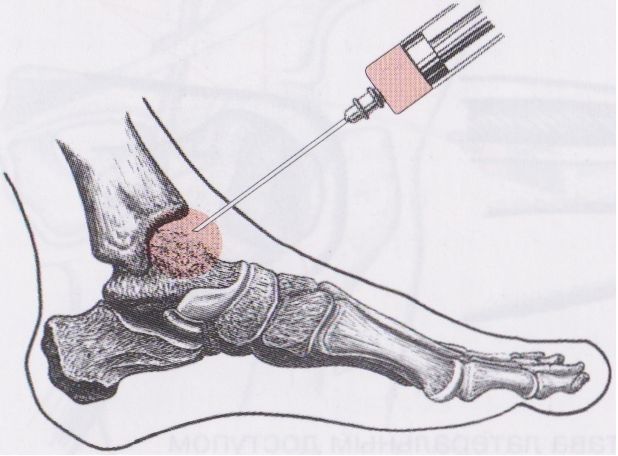
Surgery may be recommended to restore mobility to the joints of the legs or to repair damaged joints in the legs. Doctors who specialize in surgery for painful joints are orthopedic surgeons. Surgeries range from arthroscopy to partial and total leg joint replacement.
 [ 23 ], [ 24 ], [ 25 ], [ 26 ]
[ 23 ], [ 24 ], [ 25 ], [ 26 ]
Arthroscopy
Arthroscopy is a surgical technique in which a doctor inserts a tube-like instrument into a joint to view and remove deformed tissue.
Total joint arthroscopy is a surgical procedure in which a damaged joint is replaced with artificial materials. For example, small joints in the hands or feet may be replaced with plastic.
Large joints such as hips or knees can be replaced with metal parts.
Psychological support
Joint exercises, while minimizing emotional stress, can help improve the overall health of people with rheumatoid arthritis. Support and special psychological groups provide people with rheumatoid arthritis with time to discuss their problems with others and learn more about their disease.
What is the prognosis for people with rheumatoid arthritis?
With early, aggressive treatment, the outlook for those affected by rheumatoid arthritis can be very good. The medical profession's attitude toward the control of the disease has changed dramatically since the turn of the century. Doctors now strive to eliminate any signs of disease activity, preventing flare-ups and attacks. The disease can be controlled, and the combined efforts of doctor and patient can lead to good results.
Patients have a less favorable prognosis when they have joint deformities in the legs or arms, disability, persistent uncontrolled joint inflammation, and/or rheumatoid disease affecting other organs in the body. In general, rheumatoid arthritis tends to be potentially more destructive to the leg joints when rheumatoid factor or citrulline antibodies are present in the blood.
Can Rheumatoid Arthritis and Leg Pain Be Prevented?
There are currently no specific measures to prevent rheumatoid arthritis. Because smoking, exposure to inflammatory and chronic periodontal diseases increase the risk of developing rheumatoid arthritis, these activities should be avoided.
What research is being done for people with rheumatoid arthritis?
Scientists around the world are exploring many promising new approaches to relieve rheumatoid arthritis symptoms and leg pain. These areas include treatments that block the action of specific inflammatory factors such as tumor necrosis factor (TNFalpha), B cell and T cell functions, and interleukin-1 (IL-1), as described above. Many other drugs are being developed to target specific critical white blood cells involved in rheumatoid inflammation. In addition, new drugs with novel mechanisms of action differ from traditional drugs.
Other methods of targeting diseased joints will more accurately identify which patients are at risk for developing an aggressive disease such as rheumatoid arthritis. A recent antibody study found that the presence of citrulline antibodies in the blood is associated with a predisposition to more destructive forms of rheumatoid arthritis.
Genetic research may bring many new opportunities for early diagnosis and precise treatment of leg tissues in the near future. There are studies underway that use gene analysis to determine which patients are at higher risk and have a more aggressive course of the disease. All this is happening because of the improvement of technology. We are on the verge of huge improvements in how to manage rheumatoid arthritis.

