Medical expert of the article
New publications
Surgical treatment of external hemorrhoids
Last reviewed: 08.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Hemorrhoids are a disease that brings a lot of unpleasant moments and discomfort, especially to those who have to sit for a long time. This is pain, itching, a feeling of heaviness, burning in the anus. The urge to empty the bowels is perceived with a shudder, because it is often accompanied by bleeding, severe pain. Symptoms depend on the severity of the pathology, on whether it is internal or external. At the initial stages, conservative treatment is used. [ 1 ] If this does not lead to success, hemorrhoids continue to progress, internal nodes constantly fall out during defecation, work capacity decreases, then they resort to surgical treatment. [ 2 ]
Surgical treatment of external hemorrhoids
Hemorrhoids are provoked by circulatory disorders in the lower parts of the intestine. Hemorrhoidal nodes increase in size and, against the background of increasing degenerative processes in the sphincter, fall out of the anus. Dense painful seals are found around it, inflammatory complications are possible, causing fever, increased temperature.
The need to remove external hemorrhoids arises at stages 3-4 of the disease, when drug therapy has proven ineffective.
The third stage corresponds to a condition when the nodes fall out even from slight physical exertion and are put back in manually. At the fourth and last stage, this happens constantly, the nodes cannot be returned to the anal canal, heavy bleeding leads to anemia. [ 3 ]
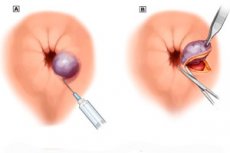
There are various methods of hemorrhoidectomy, for example, Milligan-Morgan, Whitehan and others. The operation is performed under general anesthesia, the nodes are excised with a scalpel in a certain way, the wounds are sutured with absorbable threads. Although surgical treatment often entails complications leading to anal sphincter insufficiency, the formation of canal strictures, a long period of rehabilitation, but in difficult cases this approach is still relevant. Along with it, minimally invasive techniques are used that do not require general anesthesia. [ 4 ]
Removal of external hemorrhoids under local anesthesia
A number of operations to remove external hemorrhoids without a scalpel are performed under local anesthesia. Depending on the stage of the disease, this may be:
- infrared photocoagulation (exposure of the node to high temperature, after which it dies);
- sclerotherapy (a sclerosing agent injected into the node causes its atrophy);
- transanal dearterialization of hemorrhoidal arteries under Doppler control (ultrasound reduces the blood flow to the hemorrhoidal node, after which it dries up);
- electrocoagulation (using alternating current supplied to electrodes between which the base of the node is clamped, tissue denaturation occurs). [ 5 ]
Ligation for external hemorrhoids
The ligation procedure involves putting a latex ring on the hemorrhoidal node using a ligator. At this stage, 2 types are used:
- vacuum, when a vacuum is used to suck a unit into a special cylinder and a ring is dropped onto its surface;
- mechanical - the same procedure, but carried out manually with special tweezers.
The technique is used at stages 2 and 3 of hemorrhoids. No more than 2 nodes are removed per session. Prevention of possible complications is carried out using antibiotics. [ 6 ]
Laser treatment of external hemorrhoids
Another operation performed under local anesthesia is laser coagulation, which is relatively painless and less traumatic than hemorrhoidectomy. Its essence is that a beam focused on the external hemorrhoidal node cuts it off and after healing there are no scars left. [ 7 ]
The advantages of this procedure are that it does not require hospitalization, has a short postoperative period, and has a low risk of relapse.

