Medical expert of the article
New publications
Steatocystoma
Last reviewed: 29.06.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Steatocystoma (synonym: sebocystoma) is a benign, non-void neoplasm filled with fatty secretion. It is rare, and rashes can be solitary, simple - steatocystoma simplex - or multiple. Multiple steatocystoma is a rare genetic disorder. [1] It is characterized by multiple dermal cysts of varying sizes that are present in areas where the pilosebaceous unit is well developed, predominantly in the armpits, trunk, and extremities. [2] In women, steatocystoma is more commonly seen in the inguinal region, and in men it usually has a diamond-shaped distribution on the trunk. Rarely found on the scalp and face, lesions range from normochromic to yellow, are mobile, slow-growing, and mostly contain fluid.
Steatocystoma appears in adolescence or early adulthood. In most cases, the disease is of the autosomal dominant type, but it can also occur sporadically. [3], [4]
Causes of the steatocystomas
Since this dermatologic pathology is quite rare, the causes of its occurrence are not precisely studied and are still hypothetical. Familial cases of the disease in several generations are known, it is assumed that it is inherited by autosomal dominant type. At the same time, the medical literature describes many more single (sporadic) cases of steatocystoma, and many patients had concomitant congenital or acquired keratoses and other systemic diseases.
The presumed cause of single or multiple steatocysts is androgenic (progesterone) stimulation of the sebaceous gland, which occurs during hormonal changes during adolescence. This hypothesis is based on the fact that the onset of the disease in the vast majority of cases is recorded in adolescents or young adults in post-puberty. The influence of unfavorable ecology, trauma, infection, immune system dysfunction is not excluded.
There are no statistics on the incidence of the disease. Some authors claim that steatocytomatosis is more common in young male people, others that gender is irrelevant. The age of manifestation of skin rashes predominantly varies from 12 to 25 years, they remain on the body throughout life. There are also isolated cases of early manifestation in infancy and late manifestation in old age.
The familial form may be associated with a mutation in keratin 17, a type 1 keratin found in sebaceous glands and hair follicles.The same mutation is found in congenital pachyonychia type 2, with which steatocystoma may be associated, a dominant autosomal disorder that manifests with nail dystrophy, palmar and plantar keratoderma, oral leukoplakia, follicular keratosis, and epidermal inclusion cysts.In addition, steatocystoma may present with hypertrophic squamous lichen planus, acrokeratosis verruciformis, natal dentition, and other manifestations.
Within the same family, phenotypic variations exist, as in the case of our patient, and subtypes may overlap. The same mutation in the keratin 17 gene may manifest in steatocystoma or pachyonychia type 2 alone or in combination. More than 11 different mutations have been described; however, the resulting phenotype is independent of the type of mutation. It is possible that these manifestations are spectra of the same disease.
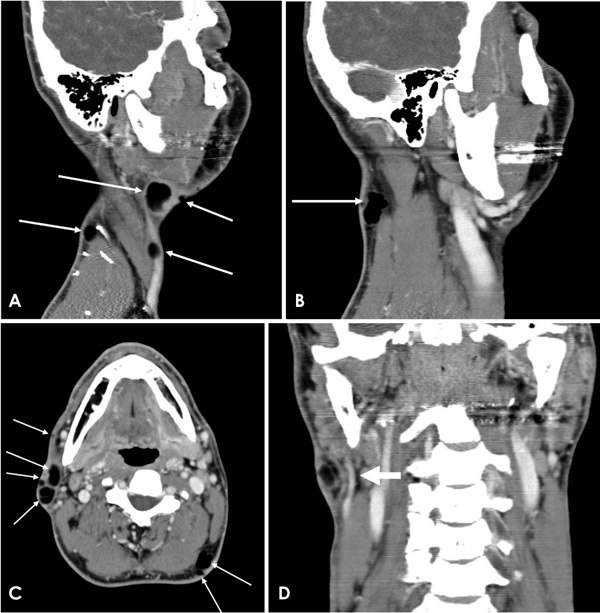
In addition to purulent steatocystoma, there are other reports of rare variants of steatocystoma such as facial, acral, vulvar, and simple steatocystoma (single lesion).
Risk factors
Steatocystoma has been observed by some investigators to be associated with the following congenital pathologies with a similar type of inheritance:
- Jackson-Lawler type pachyonychia - congenital polykeratosis with severe nail lesions;
- Coilonychia;
- Hereditary collagenosis - Ehlers-Danlos syndrome;
- Congenital cardiomyopathic lentiginosis (Leopard syndrome);
- Arteriohepatic dysplasia;
- Trichoblastoma;
- Basal cell nevus syndrome;
- Familial cases of syringoma;
- Keratoacanthoma;
- Acrokeratosis verruciformis;
- Gardner's syndrome;
- Polycystic kidney disease;
- Bilateral preauricular sinus.
The risk of steatocystoma is higher in patients with dermatitis of presumed autoimmune nature - suppurative hidradenitis suppurativa and red flat lice, collagenoses - rheumatoid arthritis, hypothyroidism; people with insufficient sweating and white spots on the nails (leukonychia).
Pathogenesis
The familial form of the disease is associated with a gene mutation at the 17q12-q21 locus. The KRT17 gene, which encodes a protein of keratin-containing intracellular filamentous intermediate structures of sebaceous glands, hair follicles, and nail bed, is altered. The mutation leads to impaired keratinization in the upper parts of hair follicles, resulting in deformation of sebaceous gland ducts and formation of cystic formations.
Many sporadic cases of steatocystomatosis are also known, so other etiopathogenetic factors other than inheritance are hypothesized. Other hypotheses consider the pathology as:
- Hamartoma of the sebaceous-hair apparatus;
- A type of dermoid cyst;
- Retention seborrheic cysts;
- Nevoid formations of underdeveloped hair follicles with attached sebaceous glands.
Start the pathogenesis of pathology hormonal surges, immune failures, trauma and transferred infections.
Symptoms of the steatocystomas
The first signs are the appearance on the skin of one or many painless on palpation hemispherical moderately elastic mobile cystic nodules. At the beginning they are translucent, whitish or bluish, with time they acquire a yellowish color. The diameter of hemispheres varies from two to five millimeters. Sometimes the size of the neoplasm can be larger - the maximum known is 3 cm.
Rashes are located on areas of the body with a high density of sebaceous-hair structures - in the groin, armpits, in men, in addition, on the chest, scrotum, penis, the outer surface of the hands and feet. At the same time on the scalp and face they are practically absent.
Puncture of a steatocystoma produces a translucent oily content or a thicker creamy yellowish substance in which fine hairs may be found.
According to the nature of the spread, the following forms of the disease are distinguished:
- Generalized - diffuse spread, involving the face, neck, back, chest and abdomen, less often - the extremities, in these cases, dystrophic changes in teeth and nails, hair loss, excessive keratinization of the skin of the palms and soles, sweating disorders;
- Localized - multiple steatocystomas of any one area of the body;
- Solitary or simple - a single neoplasm of any localization.
There is also a purulent subtype of steatocystoma (steatocystoma suppurativa), which is characterized by spontaneous rupture of cysts with the subsequent development of inflammation, ending with scarring.
Multiple rashes are usually arranged in groups, less often scattered.

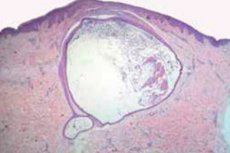
Morphologically, the neoplasm is a cyst, the shell of which is lined in several layers with squamous epithelium without a granular layer. In its cavity can be found downy hairs, and on the outer side - lobules of sebaceous glands.
According to electron microscopy, there are signs of nevoid neoplasm connected to the outer layer of skin by a thin duct, which consists of undifferentiated epithelial cells.
Complications and consequences
A steatocystoma is a chronic benign tumor that is more of a cosmetic defect. Although it is a benign condition and most lesions are asymptomatic, there is an inflammatory variant. In this case, there is spontaneous rupture of the cyst, suppuration and foul smelling discharge, especially with secondary colonization by bacteria. [5] Abscesses may also occur. These resemble the lesions of conglobate acne or suppurative hidradenitis. The lesions may progress to scarring, causing the patient great discomfort.
Malignization is unlikely, but there is evidence that it is possible.
Diagnostics of the steatocystomas
Steatocystoma is diagnosed on the basis of the patient's complaints, family history, clinical picture of pathologic changes in the skin and the results of histologic examination of the neoplasm.
Assess the general condition of the patient. Take general clinical tests of urine and blood, biochemistry - they are usually within normal limits. The doctor may prescribe specific tests and consultations of related specialists in case of suspected systemic pathologies - rheumatoid arthritis, hypo- or hyperthyroidism.
Instrumental diagnosis is performed - microscopy of the tumor contents and examination of its structure. According to the results of morphologic examination, a cyst with an arbitrarily shaped cavity, the shell of which consists of two layers, should be detected under the unchanged skin surface. The inner layer is lined with squamous epithelium cells covered with cuticle containing eosinophils, the granular layer is not defined. The outer layer is connective tissue. Segments of sebaceous glands are visible in the shell, opening into the hair follicle. The cysts are connected to the epidermal layer by short strands consisting of undifferentiated keratocytes. Culture analysis of the contents of the cystic cavity (in the absence of inflammation) shows no growth of pathogenic bacterial flora.
The clinical features of steatocystoma may resemble a number of diseases: downy cysts, myxoid cysts, miliums, conglobate acne, hidradenitis, and pseudofolliculitis, delaying diagnosis and proper monitoring.Purulent steatocystoma should be distinguished from severe nodular cystic acne, conglobate acne, infected fibroadenoma, and pyoderma.
Differential diagnosis
Differential diagnosis causes certain difficulties, especially when it is necessary to distinguish sebocystoma from eruptive cysts of downy hair, especially since in some cases both neoplasms occur simultaneously. They are differentiated by morphologic features. The cavity of an eruptive velous cyst is covered with squamous epithelium (like the cavity of a sebocystoma), but a granular layer is present, and many downy hairs are found.
In addition, differentiation is made with the following entities:
- Epidermal cysts and dermoids;
- Keratin-containing cysts (miliums);
- Lipomas (commonly referred to as fatty tumors);
- Sebaceous gland adenoma symmetric (Pringle-Burneyville disease);
- Syringoma;
- Gardner's syndrome;
- Calcinosis of the skin;
- Apocrine sweating;
- Conglobate acne;
- Cystic acne.
Treatment of the steatocystomas
Treatment is varied and usually unsatisfactory due to the difficulty in accessing such disseminated lesions.
Steatocystomas are removed mainly for cosmetic purposes. The following methods are used:
- Surgical excision;
- Needle aspiration;
- Radiowave knife removal;
- Electrocoagulation;
- Cryodestruction;
- Laser destruction.
The best cosmetic effect is given by radio wave and laser treatment.
In purulent steatocystomas systemic therapy with isotretinoin, tetracycline with opening and drainage of the cystic cavity is used. Intrathecal administration of triamcenolone acetonide is prescribed.
Inflamed lesions can be treated with corticosteroid injections or drainage. Mixed results have been reported using oral isotretinoin for the treatment of steatocystoma. Isotretinoin does not usually eliminate the condition, but it does reduce the size of purulent lesions. This therapeutic response probably reflects the anti-inflammatory effect of retinoids.
It has been reported in the literature that no relapses have been noted after systemic therapy.

