Medical expert of the article
New publications
Role of changes in subchondral bone in the pathogenesis of osteoarthritis
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
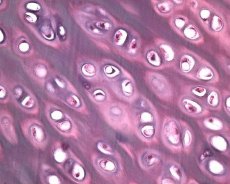
Along with the degeneration of articular cartilage, the underlying bone tissue is also involved in the pathological process in osteoarthrosis. It is assumed that thickening of the subchondral plate contributes to the progression of osteoarthrosis. As osteoarthrosis progresses, articular cartilage, which is subject to mechanical and chemical stress, slowly erodes due to an imbalance in the processes of cartilage catabolism and reparation. In particular, mechanical stress in relation to the joints “bearing” the body weight contributes to the formation of a large number of microfractures in the subchondral plate and cartilage. As the articular cartilage erodes, sclerosis of the subchondral bone progresses, the rigidity of bone tissue increases, which in turn contributes to further disruption of the structure of the articular cartilage. However, the question of the primary or secondary nature of subchondral bone changes in osteoarthrosis remains unresolved.
Until recently, radiographically detectable changes in the spongy substance of the subchondral bone, such as sclerosis or cyst formation, were considered secondary in patients with osteoarthrosis. However, the results of clinical and experimental studies indicate a possible initiating role of the subchondral bone in the pathogenesis of osteoarthrosis. One of the possible mechanisms is a sharp increase in the stiffness gradient of the subchondral bone due to the fact that the integrity of the underlying cartilage tissue depends on the mechanical properties of its bone "bed". Studies in primates have shown that changes in the subchondral bone can precede changes in the articular cartilage. The evidence for and against this hypothesis that has emerged as a result of studies in animal models of osteoarthrosis and clinical studies has only intensified the debate. Thickening of the trabeculae in the subchondral bone is not always accompanied by an increase in bone mineralization, or rather, an increase in the volume of osteoid. This sign of abnormal mineralization indicates that the disturbance of regulation of bone remodeling is an integral part of osteoarthritis and also supports the concept of a bone cell defect in osteoarthritis. J. Dequeker's group (1989) consider the latter to be a "generalized metabolic bone disease".
Bone tissue is constantly renewed. This dynamic process, called bone remodeling, is a complex sequence of resorption and mineralization. Osteoclasts resorb bone tissue, and osteoblasts secrete proteins that form the main organic component for mineralization. Bone formation and resorption do not occur randomly throughout the skeleton; it is a programmed process that occurs in different areas of the skeleton, called bone remodeling units. Early in the cycle, osteoclasts appear on the inactive surface; within 2 weeks, they form a tunnel in the cortical bone or a lacuna on the surface of trabecular bone. The frequency of activation of new bone remodeling units determines the degree of bone renewal. In a healthy young person, the processes of bone formation and resorption are balanced, and normal bone mass is maintained. In the hormonal regulation of bone tissue resorption, at least PTH and PGE2 , not only osteoclasts but also osteoblasts participate, since under the influence of these hormones, factors stimulating bone resorption by osteoclasts are released. Currently, more than 12 local and systemic regulators of bone tissue growth are known that affect its remodeling, in particular PTH, 1,25(OH) 2D3 ,calcitonin, growth hormone, glucocorticoids, thyroid hormones, insulin, IGF (1 and 2), estrogens, PGE2 , androgens.
Bone cells release a number of proteins and cytokines that perform endocrine regulation and signal transduction. Proteins produced by osteoblasts include bone matrix proteins such as collagen, osteopontin, osteocalcin, bone sialoproteins. In addition, these cells release proteases in both active and latent forms that participate in the process of bone tissue remodeling - MMPs, components of the plasminogen activator (PA)/plasmin system. Cytokines released by osteoblasts can act both through autocrine mechanisms and paracrine pathways on local cells (other osteoblasts, osteoclasts).
It is not yet known whether these signals are regulated by mechanical stress or other chemical signals induced by mechanical stress. However, it is known that repeated mechanical stress causes local proliferation of bone cells and/or proteins. In vivo, mechanical loading can activate osteoblasts, increase the level of cyclic nucleotides, prostaglandin production, and cause morphological changes associated with bone remodeling. In vitro, mechanical stress causes proliferation of osteoblast cultures, expression of mRNA of bone proteins involved in osteoid formation and mineralization, release of local growth factors such as IGF-1 and IGF-2, and adhesion molecules. Transmission of the mechanical stress signal can be carried out through mechanosensitive ion channels.
There is indirect evidence of osteoblast dysfunction in osteoarthrosis. G. Gevers and J. Dequeker (1987) demonstrated an increase in serum osteocalcin levels in women with hand osteoarthrosis, as well as in cortical bone explants, indicating that bone pathology may be part of osteoarthrosis. Autopsy revealed not only thickening of the subchondral bone, but also abnormally low mineralization of the femoral head. In guinea pigs with surgically induced osteoarthrosis, computed tomography revealed significant thickening of the bone fraction in the subchondral zone. An imbalance between collagen and non-collagen (osteocalcin, etc.) proteins can lead to an increase in bone volume, but does not affect its mineral density. According to M. Shimizu et al. (1993), the progression of degenerative changes in articular cartilage is associated with more intensive remodeling of the subchondral bone and an increase in its rigidity, which also indicates a defect in bone tissue cells in osteoarthrosis. According to the hypothesis proposed by B. Lee and M. Aspden (1997), the proliferation of defective bone cells can lead to an increase in bone tissue rigidity, but does not cause an increase in its mineral density.
C. I. Westacott et al. (1997) hypothesized that abnormal osteoblasts directly affect cartilage metabolism. Cultivating osteoblasts from patients with osteoarthritis with chondrocytes from people who did not have joint diseases, the authors observed a significant change in the release of glycosaminoglycans by normal cartilage tissue in vitro, but the level of cytokine release remained unchanged. G. Hilal et al. (1998) showed that the culture of osteoblasts from subchondral bone of patients with osteoarthritis in vitro has an altered metabolism - the activity of the AP/plasmin system and the level of IGF-1 in these cells are increased. The observation of C. I. Westacott et al. (1997) can be explained by an increase in the activity of proteases in subchondral bone cells.
It remains unknown whether changes in the subchondral bone initiate osteoarthritis or contribute to its progression. DK Dedrick et al. (1993) demonstrated that in dogs with surgically induced osteoarthritis, thickening of the subchondral bone is not a necessary condition for the development of osteoarthrosis-like changes in the articular cartilage, but contributes to the progression of degenerative processes in the cartilage. The results of the study by A. Sa'ied et al. (1997) contradict the data of the previous study. Using 50 MHz echography to assess the initial morphological changes and their progression in articular cartilage and bone in experimental osteoarthritis induced by injections of monoiodoacetic acid into the stifle joint of rats, the authors demonstrated a simultaneous process of changes in bone and cartilage during the first three days after injection.
Osteoblasts secrete growth factors and cytokines involved in local bone remodeling, which may promote remodeling of proper cartilage in “weight-bearing” joints after their penetration through microcracks in the calcified layer of articular cartilage. Moreover, bone cell secretory products are found in synovial fluid. The most likely products secreted by abnormal osteoblasts that can initiate the process of local cartilage remodeling are TGF-b and bone morphometric proteins (BMPs). Both members of the TGF family are secreted by both chondrocytes and osteoblasts, and both are capable of modifying both bone and cartilage remodeling. J. Martel Pelletier et al. (1997) observed an increase in the level of TGF-β in subchondral bone explants of patients with osteoarthrosis compared to healthy individuals, which indicates a probable role of this growth factor in the pathogenesis of osteoarthrosis. IGFs are also produced by osteoblasts. In a culture of osteoblast-like cells obtained from patients with osteoarthrosis, an increase in the level of IGFs was found, which alter cartilage metabolism.
TGF-b, IGF, BMP and cytokines produced by osteoblasts in the subchondral bone may influence the production of collagenase and other proteolytic enzymes in cartilage, which in turn may promote remodeling/degradation of the cartilage matrix. It remains unclear whether osteoblasts in OA produce less macrophage colony-stimulating factor (M-CSF - a stimulator of bone resorption) than normal cells. The results of studies by AG Uitterlinden et al. (1997) showed that vitamin D receptors, which are expressed by osteoblasts and regulate the expression of a number of factors synthesized by these cells, may play a certain role in the formation of osteophytes, which partially explains the role of osteoblasts in the pathogenesis of this disease.
Taking into account the results of the above studies, G. Hilal et al. (1998), J. Martel-Pelletier et al. (1997) proposed the following working hypothesis of the relationship between subchondral bone remodeling and proper articular cartilage in osteoarthrosis. At an early or advanced stage of OA pathogenesis, the process of bone tissue remodeling in the subchondral bone intensifies. At the same time, repeated loading leads to local microfractures and/or the appearance of an imbalance in the IGF/IGF-binding protein (IGFBP) system due to an abnormal response of subchondral bone osteoblasts, which contributes to its sclerosis. The latter in turn can contribute to the appearance of microfractures of proper cartilage and damage to its matrix.
Under normal conditions, this damage is repaired by local synthesis and release of IGF-1 and IGF-binding protein, which stimulate the formation of articular cartilage ECM. At the same time, the GF-system promotes the growth of subchondral bone cells and the formation of bone matrix. The anabolic activity of the IGF-system is increased in the subchondral bone of patients with osteoarthrosis, while local activation of the AP/plasmin system (a local regulator of the IGF-system) in articular cartilage causes its local changes. In osteoblasts in osteoarthrosis, IGF-1 disrupts the regulation of AP by plasmin by the positive feedback type, therefore, it can restrain remodeling in bone tissue, which ultimately leads to subchondral sclerosis. Thus, in bone and cartilage tissue, local induction of IGF-1 and proteases leads, on the one hand, to cartilage damage, on the other hand, to subchondral bone thickening, the latter in turn contributing to further cartilage damage. The imbalance between cartilage damage associated with subchondral sclerosis and its reparative capabilities leads to progressive changes in the cartilage ECM and to the development of osteoarthrosis. According to the authors, this hypothesis also explains the slow progression of the disease.

