Medical expert of the article
New publications
Respiratory bronchus
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
As the caliber of the bronchi decreases, their walls become thinner, the height and number of rows of epithelial cells decrease. Non-cartilaginous (or membranous) bronchioles have a diameter of 1-3 mm, there are no goblet cells in the epithelium, their role is performed by Clara cells, and the submucosal layer without a clear boundary passes into the adventitia. Membranous bronchioles pass into terminal ones with a diameter of about 0.7 mm, their epithelium is single-row. Respiratory bronchioles with a diameter of 0.6 mm branch off from the terminal bronchioles. Respiratory bronchioles are connected to the alveoli through pores. Terminal bronchioles are air-conducting, respiratory ones participate in air conduction and gas exchange.
The total cross-sectional area of the terminal respiratory tract is many times greater than the cross-sectional area of the trachea and large bronchi (53-186 cm2 versus 7-14 cm2 ), but the bronchioles account for only 20% of the airflow resistance. Due to the low resistance of the terminal respiratory tract, early bronchiole damage may be asymptomatic, not accompanied by changes in functional tests, and be an incidental finding on high-resolution computed tomography.
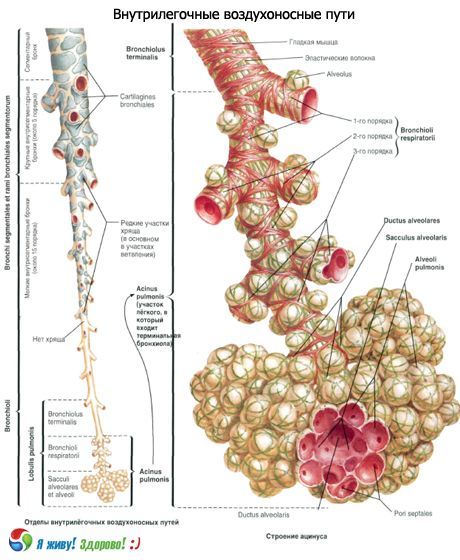
According to the International Histological Classification, the set of branches of the terminal bronchiole is called the primary pulmonary lobule, or acinus. This is the most numerous structure of the lung, in which gas exchange occurs. Each lung has 150,000 acini. The acinus of an adult is 7-8 mm in diameter and has one or more respiratory bronchioles. The secondary pulmonary lobule is the smallest unit of the lung, limited by septa of connective tissue. Secondary pulmonary lobules consist of 3 to 24 acini. The central part contains a pulmonary bronchiole and an artery. They are called the lobular nucleus or "centrilobular structure". Secondary pulmonary lobules are separated by interlobular septa containing veins and lymphatic vessels, arterial and bronchiolar branches in the lobular nucleus. The secondary pulmonary lobule is usually polygonal in shape with the length of each of the constituent sides being 1–2.5 cm.
The connective tissue framework of the lobule consists of interlobular septa, intralobular, centrilobular, peribronchovascular, and subpleural interstitium.
The terminal bronchiole is divided into 14-16 first-order respiratory bronchioles, each of which is in turn dichotomously divided into second-order respiratory bronchioles, which are dichotomously divided into third-order respiratory bronchioles. Each third-order respiratory bronchiole is subdivided into alveolar ducts (100 μm in diameter). Each alveolar duct ends in two alveolar sacs.
The alveolar passages and sacs have protrusions (bubbles) in their walls - alveoli. There are approximately 20 alveoli per alveolar passage. The total number of alveoli reaches 600-700 million with a total area of about 40 m2 during exhalation and 120 m2 during inhalation.
In the epithelium of the respiratory bronchioles, the number of ciliated cells progressively decreases and the number of non-ciliated cuboidal cells and Clara cells increases. The alveolar ducts are lined with squamous epithelium.
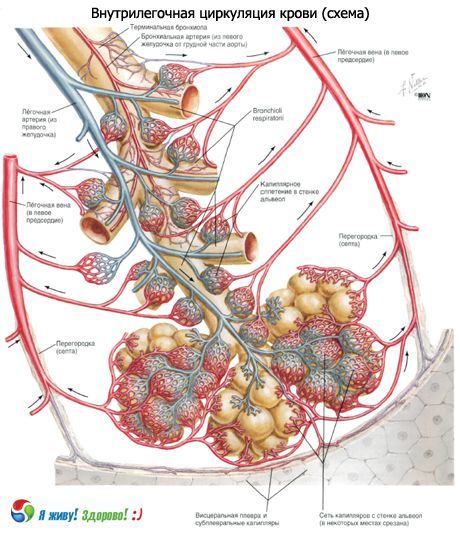
Electron microscopic studies have made a significant contribution to the modern understanding of the alveolus structure. The walls are common to two adjacent alveoli over a large area. The alveolar epithelium covers the wall on both sides. Between the two layers of the epithelial lining there is an interstitium in which the septal space and a network of blood capillaries are distinguished. The septal space contains bundles of thin collagen fibers, reticulin and elastic fibers, a few fibroblasts and free cells (histiocytes, lymphocytes, neutrophilic leukocytes). Both the epithelium and the endothelium of the capillaries lie on a basal membrane 0.05-0.1 μm thick. In some places, the subepithelial and subendothelial membranes are separated by the septal space, in other places they touch, forming a single alveolar-capillary membrane. Thus, the alveolar epithelium, alveolar-capillary membrane and endothelial cell layer are components of the air-blood barrier through which gas exchange occurs.
The alveolar epithelium is heterogeneous; three types of cells are distinguished in it. Alveolocytes (pneumocytes) of type I cover most of the surface of the alveoli. Gas exchange occurs through them.
Alveolocytes (pneumocytes) type II, or large alveolocytes, are round and protrude into the lumen of the alveoli. Microvilli are present on their surface. The cytoplasm contains numerous mitochondria, a well-developed granular endoplasmic reticulum, and other organelles, the most characteristic of which are membrane-bound osmiophilic lamellar bodies. They consist of an electron-dense layered substance containing phospholipids, as well as protein and carbohydrate components. Like secretory granules, lamellar bodies are released from the cell, forming a thin (about 0.05 μm) film of surfactant, which reduces surface tension, preventing the collapse of the alveoli.
Type III alveolocytes, described under the name of brush cells, are distinguished by the presence of short microvilli on the apical surface, numerous vesicles in the cytoplasm and bundles of microfibrils. They are believed to perform fluid absorption and surfactant concentration or chemoreception. Romanova L.K. (1984) suggested their neurosecretory function.
In the lumen of the alveoli, there are normally a few macrophages that absorb dust and other particles. At present, the origin of alveolar macrophages from blood monocytes and tissue histiocytes can be considered established.
Contraction of smooth muscles leads to a decrease in the base of the alveoli, a change in the configuration of the bubbles - they lengthen. It is these changes, and not ruptures of the partitions, that underlie swelling and emphysema.
The configuration of the alveoli is determined by the elasticity of their walls, stretched by the increase in the volume of the chest, and by the active contraction of the smooth muscles of the bronchiole. Therefore, with the same volume of breathing, different stretching of the alveoli in different segments is possible. The third factor determining the configuration and stability of the alveoli is the force of surface tension formed at the boundary of two environments: the air filling the alveolus and the liquid film lining its inner surface and protecting the epithelium from drying out.
To counteract the surface tension force (T), which tends to compress the alveoli, a certain pressure (P) is necessary. The value of P is inversely proportional to the radius of curvature of the surface, which follows from the Laplace equation: P = T / R. It follows that the smaller the radius of curvature of the surface, the higher the pressure is necessary to maintain a given volume of alveoli (at constant T). However, calculations have shown that it should be many times greater than the intra-alveolar pressure that exists in reality. During exhalation, for example, the alveoli should collapse, which does not happen, since the stability of the alveoli at low volumes is ensured by a surface-active substance - surfactant, which reduces the surface tension of the film when the area of the alveoli decreases. This is the so-called antiatelectatic factor, discovered in 1955 by Pattle and consisting of a complex of substances of protein-carbohydrate-lipid nature, which includes a lot of lecithin and other phospholipids. Surfactant is produced in the respiratory section by alveolar cells, which, together with the cells of the surface epithelium, line the alveoli from the inside. Alveolar cells are rich in organelles, their protoplasm contains large mitochondria, therefore they are distinguished by high activity of oxidative enzymes, they also contain non-specific esterase, alkaline phosphatase, lipase. Of greatest interest are the inclusions constantly found in these cells, determined by electron microscopy. These are osmiophilic bodies of oval shape, 2-10 μm in diameter, of a layered structure, limited by a single membrane.
Surfactant system of the lungs
The surfactant system of the lungs performs several important functions. Surface-active substances of the lungs reduce surface tension and the work required for ventilation of the lungs, stabilize the alveoli and prevent their atelectasis. In this case, surface tension increases during inspiration and decreases during expiration, reaching a value close to zero at the end of expiration. Surfactant stabilizes the alveoli by immediately decreasing surface tension when the volume of the alveoli decreases and increasing surface tension when the volume of the alveoli increases during inspiration.
Surfactant also creates conditions for the existence of alveoli of various sizes. If there were no surfactant, small alveoli would collapse and pass air to larger ones. The surface of the smallest airways is also covered with surfactant, which ensures their patency.
For the functioning of the distal part of the lung, the patency of the bronchoalveolar junction is most important, where the lymphatic vessels and lymphoid accumulations are located and the respiratory bronchioles begin. The surfactant covering the surface of the respiratory bronchioles comes here from the alveoli or is formed locally. Substitution of surfactant in the bronchioles with the secretion of goblet cells leads to narrowing of the small airways, an increase in their resistance and even complete closure.
Clearance of the contents of the smallest airways, where the transport of the contents is not associated with the ciliated apparatus, is largely ensured by surfactant. In the zone of functioning of the ciliated epithelium, the dense (gel) and liquid (sol) layers of bronchial secretion exist due to the presence of surfactant.
The surfactant system of the lung is involved in the absorption of oxygen and the regulation of its transport through the air-blood barrier, as well as in maintaining the optimal level of filtration pressure in the pulmonary microcirculation system.
Destruction of the surfactant film by Tween causes atelectasis. Inhalation of aerosols of lecithin compounds, on the contrary, gives a good therapeutic effect, for example, in case of respiratory failure in newborns, in whom the film can be destroyed by bile acids during aspiration of amniotic fluid.
Hypoventilation of the lung leads to the disappearance of the surfactant film, and the restoration of ventilation in the collapsed lung is not accompanied by complete restoration of the surfactant film in all alveoli.
The surface-active properties of surfactant also change in chronic hypoxia. In pulmonary hypertension, a decrease in the amount of surfactant is noted. As experimental studies have shown, impaired bronchial patency, venous congestion in the pulmonary circulation, and a decrease in the respiratory surface of the lungs contribute to a decrease in the activity of the surfactant system of the lungs.
An increase in the concentration of oxygen in the inhaled air leads to the appearance in the alveolar lumens of a large number of membrane formations of mature surfactant and osmiophilic bodies, which indicates the destruction of surfactant on the surface of the alveoli. Tobacco smoke has a negative effect on the surfactant system of the lungs. A decrease in the surface activity of surfactant is caused by quartz, asbestos dust and other harmful impurities in the inhaled air.
According to several authors, surfactant also prevents transudation and edema and has a bactericidal effect.
The inflammatory process in the lungs leads to changes in the surface-active properties of the surfactant, and the degree of these changes depends on the activity of the inflammation. Malignant neoplasms have an even stronger negative effect on the surfactant system of the lungs. With them, the surface-active properties of the surfactant decrease significantly more often, especially in the atelectasis zone.
There is reliable data on the disruption of the surface activity of surfactant during prolonged (4-6 hours) fluorothane anesthesia. Operations using artificial blood circulation machines are often accompanied by significant disruptions in the surfactant system of the lungs. Congenital defects of the surfactant system of the lungs are also known.
Surfactant can be detected morphologically by fluorescent microscopy due to primary fluorescence in the form of a very thin layer (0.1 to 1 µm) lining the alveoli. It is not visible in an optical microscope, and is also destroyed when preparations are treated with alcohol.
There is an opinion that all chronic respiratory diseases are associated with a qualitative or quantitative deficiency of the surfactant system of the respiratory organs.


 [
[