Medical expert of the article
New publications
Muscle strength study
Last reviewed: 07.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
Muscle strength is a quantitative measure expressing the ability of a muscle to contract while resisting an external force, including gravity. Clinical examination of muscle strength primarily reveals its decrease. A preliminary, approximate assessment of muscle strength begins with determining whether the subject can perform active movements in all joints and whether these movements are performed in full.
Having detected limitations, the doctor performs passive movements in the corresponding joints to exclude local lesions of the musculoskeletal system (muscle and joint contractures). Limitation of passive movements in a joint caused by bone and joint pathology does not exclude that the patient may have reduced muscle strength. At the same time, the absence or limitation of active voluntary movements with a full range of passive movements in an awake and cooperating patient indicates that the cause of the disorder is most likely a pathology of the nervous system, neuromuscular junctions or muscles.
The term " paralysis " (plegia) denotes a complete absence of active movements caused by a disruption of the innervation of the corresponding muscles, and the term "paresis" denotes a decrease in muscle strength. Paralysis of the muscles of one limb is called monoplegia, paralysis of the lower facial muscles, arm and leg on the same side of the body is called hemiplegia; paralysis of the muscles of both legs is called paraplegia, paralysis of the muscles of all four limbs is called tetraplegia.
Paralysis/paresis may result from damage to either the central (upper) or peripheral (lower) motor neuron. Accordingly, there are two types of paralysis: peripheral (flaccid) paralysis occurs as a result of damage to the peripheral motor neuron; central (spastic) paralysis occurs as a result of damage to the central motor neuron.
Damage to the central motor neuron (for example, in cerebral stroke ) affects the muscles of the limbs to varying degrees. In the arm, the abductors and extensors are predominantly affected, and in the leg, the flexors. Damage to the pyramidal system at the level of the internal capsule (where the axons of the Betz pyramidal cells are located very compactly) is characterized by the formation of the pathological Wernicke-Mann posture: the patient's arm is bent and brought to the body, and the leg is straightened and, when walking, is abducted to the side so that the foot moves along an arc ("the arm asks, the leg squints").
In peripheral motor neuron pathology, each level of damage (involving the anterior horns of the spinal cord, the spinal nerve root, the plexus, or the peripheral nerve) has a characteristic type of muscle weakness distribution (myotome, neurotome). Muscle weakness is not only neurogenic: it also occurs in primary muscle damage (myopathy) and in pathology of the neuromuscular synapse ( myasthenia ). Joint damage can be accompanied by significant limitation of movement in it due to pain, therefore, in case of pain syndrome, one should be careful in judging muscle weakness and the presence of neurological pathology.
Muscle strength assessment
To assess muscle strength, the patient is asked to perform a movement that requires contraction of a specific muscle(s), fix the pose, and hold the muscle in the position of maximum contraction, while the examiner tries to overcome the subject's resistance and stretch the muscle. Thus, when examining muscle strength in clinical practice, the principle of "tension and overcoming" is most often used: the doctor resists the patient's straining the muscle being examined and determines the degree of effort required for this. Different muscles or muscle groups are examined in turn, comparing the right and left sides (this makes it easier to detect minor muscle weakness).
It is important to follow certain rules of examination. Thus, when assessing the strength of the shoulder abductor muscles, the doctor should stand in front of the patient and resist the movement with only one hand (but not lean over the seated patient, putting pressure on the patient's hand with the entire weight of the body). Similarly, when assessing the strength of the finger flexors, the doctor uses only his finger, equivalent to the one being tested, but does not apply the strength of the entire hand or arm as a whole. It is also necessary to make adjustments for the child or old age of the patient. Muscle strength is usually assessed in points, most often on a 6-point system.
Criteria for assessing muscle strength using a 6-point system
Score |
Muscle strength |
0 |
There is no muscle contraction. |
1 |
Visible or palpable contraction of muscle fibers, but without locomotor effect |
2 |
Active movements are possible only when the force of gravity is eliminated (the limb is placed on a support) |
3 |
Active movements in full range under the action of gravity, moderate decrease in strength under external resistance |
4 |
Active movements in full range under the action of gravity and other external resistance, but they are weaker than on the healthy side |
5 |
Normal muscle strength |
When examining the neurological status, it is necessary to determine the strength of the following muscle groups.
- Flexors of the neck: m. sternodeidomastoideus (n. accessories, C 2 -C 3 - nn. cervicales).
- Neck extensors: mm. profundi colli (C 2 -C 4 - nn. cervicales).
- Shrugging the shoulders: m. trapezius (n. accessories, C 2 -C 4 - nn. cervicales).
- Shoulder abduction: m. deltoideus (C 5 -C 6 - n. axillaris).
- Flexion of the supinated arm at the elbow joint: m. biceps brachii (C 5 -C 6 - n. musculocutaneus).
- Extension of the arm at the elbow joint: m. triceps brachii (C 6 -C 8 - n. radialis).
- Extension in the wrist joint: mm. extensores carpi radialis longus et brevis (C 5 -C 6 - n. radialis), m. extensor carpi ulnaris (C 7 -C 8 - n. radialis).
- Opposition of the thumb: m. opponens pollicis (C 8 -T 1 - n. medianus).
- Abduction of the little finger: m. abductor digiti minimi (C 8 -T 1 - n. ulnaris).
- Extension of the proximal phalanges of the II-V fingers: m. extensor digitorum communis, m. extensor digiti minimi, m. extensor indicis (C 7 -C 8 - n. profundus n. radialis).

- Flexion of the thigh at the hip joint: m. iliopsoas (L 1 -L 3 - n.femoralis).
- Extension of the leg at the knee joint: m. quadriceps femoris (L 2 -L 4 - n. femoris).
- Flexion of the leg at the knee joint: m. biceps femoris, m. semitendinosus, m. semimembranosus (L 1 -S 2 - n. ischiadicus).
- Extension (dorsiflexion) of the foot at the ankle joint: m. tibialis anterior (L 4 -L 5 - n. peroneus profundus).
- Plantar flexion of the foot at the ankle joint: m. triceps surae (S 1 -S 2 - n. tibialis).

The above muscle groups are assessed using the following tests.
- Neck flexion is a test to determine the strength of the sternocleidomastoid and scalene muscles. The patient is asked to tilt (but not extend) the head to the side and turn the face to the side opposite to the tilt of the head. The doctor counteracts this movement.
- Neck extension is a test that allows us to determine the strength of the extensors of the head and neck (the vertical portion of the trapezius muscle, the splenius muscles of the head and neck, the muscles that lift the scapulae, the semispinalis muscles of the head and neck).
The patient is asked to tilt his head back, resisting this movement.
Shrug test is a test used to determine the strength of the trapezius muscle. The patient is asked to "shrug" against the doctor's resistance.
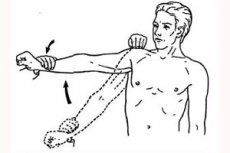
Shoulder abduction is a test to determine the strength of the deltoid muscle. At the doctor's request, the patient abducts the shoulder horizontally; it is recommended that the arm be bent at the elbow. Resist the movement by trying to lower the arm. It should be taken into account that the ability of the deltoid muscle to hold the shoulder in an abducted position is impaired not only when this muscle is weak, but also when the functions of the trapezius, anterior serratus and other muscles that stabilize the shoulder girdle are impaired.
The supinated elbow flexion test is a test designed to determine the strength of the biceps brachii. The biceps brachii is involved in flexion and simultaneous supination of the forearm. To test the function of the biceps brachii, the physician asks the subject to supinate the wrist and bend the arm at the elbow, resisting this movement.
The elbow extension test is a test used to determine the strength of the triceps brachii muscle. The examiner stands behind or to the side of the patient, asks the patient to extend the arm at the elbow, and resists this movement.
- Wrist extension is a test that helps determine the strength of the radial and ulnar extensors of the wrist. The patient extends and adducts the wrist with straight fingers, and the doctor prevents this movement.
- Opposition of the thumb is a test to determine the strength of the muscle that opposes the thumb. The subject is asked to firmly press the distal phalanx of the thumb to the base of the proximal phalanx of the little finger of the same hand and resist an attempt to straighten the main phalanx of the thumb. A test with a strip of thick paper is also used: they are asked to squeeze it between the 1st and 5th fingers and the pressing force is tested.
- Little finger abduction is a test to determine the strength of the muscle that abducts the little finger. The doctor tries to bring the patient's abducted little finger to the other fingers against its resistance.
- Extension of the main phalanges of the II-V fingers is a test used to determine the strength of the general extensor of the fingers, the extensor of the little finger, and the extensor of the index finger. The patient extends the main phalanges of the II-V fingers when the middle and nail fingers are bent; the doctor overcomes the resistance of these fingers and immobilizes the patient's wrist joint with the other hand.
Hip flexion is a test to determine the strength of the iliac, large and small lumbar muscles. The patient is asked to bend the hip (bring it to the stomach) while sitting and, at the same time, by resisting this movement, the lower third of the thigh is affected. The strength of hip flexion can also be tested with the patient lying on his back. To do this, he is asked to raise his straight leg and hold it in this position, overcoming the downward pressure of the doctor's palm, resting on the patient's mid-thigh. A decrease in the strength of this muscle is considered an early symptom of damage to the pyramidal system. Leg extension at the knee joint is a test to determine the strength of the quadriceps femoris. The test is conducted with the patient lying on his back, the leg bent at the hip and knee joints. He is asked to straighten his leg, raising his shin. At the same time, a hand is placed under the patient's knee, holding his thigh in a semi-bent position, with the other hand pressure is applied to the shin downwards, preventing its extension. To test the strength of this muscle, the patient, sitting on a chair, is asked to straighten his leg at the knee joint. With one hand, this movement is resisted, with the other - the contracting muscle is palpated.
- Knee flexion is a test necessary to determine the strength of the muscles of the back of the thigh (ischiocrural muscles). The study is conducted with the patient lying on his back, the leg bent at the hip and knee joints, the foot firmly in contact with the couch. They try to straighten the patient's leg, having previously given him the task not to lift his foot off the couch.
- Ankle extension (dorsiflexion) is a test that helps determine the strength of the anterior tibialis muscle. The patient, lying on his back with his legs straight, is asked to pull his feet towards him, slightly adducting the inner edges of the feet, while the doctor resists this movement.
- Ankle plantar flexion is a test used to determine the strength of the triceps surae and plantaris muscles. The patient, lying on his back with his legs straight, plantar flexes his feet against the resistance of the examiner's palms, which apply pressure on the feet in the opposite direction.
More detailed methods for studying the strength of individual muscles of the trunk and limbs are described in manuals on topical diagnostics.
The above methods of assessing muscle strength should be supplemented with some simple functional tests, which are intended to check the function of the entire limb rather than to measure the strength of individual muscles. These tests are important for detecting minor muscle weakness that is difficult for the physician to notice when focusing on individual muscles.
- To detect weakness in the muscles of the shoulder, forearm and hand, the patient is asked to squeeze three or four fingers of the hand as hard as possible and try to release their fingers during the squeeze. The test is performed simultaneously on the right and left hand to compare their strength. It should be taken into account that the strength of the squeeze largely depends on the integrity of the forearm muscles, so if the small muscles of the hand are weak, the handshake can remain quite strong. The strength of the squeeze of the hand can be accurately measured using a dynamometer. The squeeze test of the hand can detect not only weakness of the hand muscles, but also the phenomenon of myotonia of action, observed in such hereditary neuromuscular diseases as dystrophic and congenital myotonia. After strongly squeezing his hand into a fist or strongly squeezing someone else's hand, a patient with the phenomenon of myotonia of action cannot quickly unclench his hand.
- To detect weakness in the proximal parts of the legs, the subject should stand up from a squatting position without using their hands. In children, it is necessary to observe how they rise from a sitting position on the floor. For example, in Duchenne muscular dystrophy, the child resorts to auxiliary techniques when standing up ("climbing up oneself").
- To identify weakness in the distal parts of the legs, the patient is asked to stand up and walk on his heels and toes.
- Central (pyramidal) paresis of the arms can be detected by asking the patient to hold his arms straight with the palmar surfaces almost touching slightly above the horizontal level with his eyes closed (Barré test for the upper limbs). The arm on the side of the paresis begins to drop, while the hand bends at the wrist and rotates inward ("pronator drift"). These postural disorders are considered very sensitive signs of central paresis, allowing it to be detected even when direct examination of muscle strength does not reveal any disturbances.
- In patients with suspected myasthenia, it is important to establish whether weakness in the muscles of the head, trunk, and limbs increases with exertion. To do this, they stretch their arms out in front of them and look at the ceiling. Normally, a person can stay in this position for at least 5 minutes. Other tests that provoke muscle fatigue are also used (squats, loudly counting to 50, repeatedly opening and closing the eyes). Myasthenic fatigue can be most objectively detected using a dynamometer: the force of squeezing the hand into a fist is measured, then the patient quickly performs 50 intense clenching of both hands into a fist, after which dynamometry of the hands is again performed. Normally, the force of squeezing the hands remains almost the same before and after such a series of clenching of the hands into a fist. In myasthenia, after physical strain of the hand muscles, the force of squeezing the dynamometer decreases by more than 5 kg.


 [
[