New publications
Pigmented nevus: intradermal, borderline, complex.
Last reviewed: 04.07.2025

All iLive content is medically reviewed or fact checked to ensure as much factual accuracy as possible.
We have strict sourcing guidelines and only link to reputable media sites, academic research institutions and, whenever possible, medically peer reviewed studies. Note that the numbers in parentheses ([1], [2], etc.) are clickable links to these studies.
If you feel that any of our content is inaccurate, out-of-date, or otherwise questionable, please select it and press Ctrl + Enter.
A skin formation such as a pigment nevus consists of a cluster of melanocytes of varying degrees of differentiation, which are located in different skin layers. In common parlance, a nevus is often called a birthmark, which is not entirely correct, since in many cases the neoplasm is not congenital, but acquired. Pigment elements have a complex histological characteristic and are diverse in their clinical manifestations. [ 1 ]
Epidemiology
On average, there are about 20 pigmented nevi per population unit in the world. Such formations are more common among representatives of the white race, and less common among people with dark skin. The total number of nevus elements may increase with age.
In infants of the first year of life, pigment spots are found only in 5-10% of cases. If a newborn child has a large neoplasm, then in the future, the risk of malignancy of the process increases. [ 2 ]
In adolescents aged 12-15 years, dermal nevus spots are more common, which are detected in 90% of cases.
People aged 25-30 years have, on average, 20-40 pigment spots on their body.
Causes Pigmented nevus: intradermal, borderline, complex.
It is generally accepted that the tendency to form pigmented lesions is inherited. Up to 1 in 10 cases of melanoma may be associated with inherited defective genes [ 3 ] However, in addition to the genetic factor, there are other reasons:
- radiation effects;
- regular exposure to ultraviolet radiation;
- taking hormonal drugs (including contraceptives);
- severe hormonal changes (puberty, pregnancy, menopause, etc.);
- regular consumption of products containing harmful synthetic components;
- the presence of bad habits that negatively affect the liver;
- various intoxications;
- immunodeficiency states or prolonged use of drugs that suppress the immune defense.
Risk factors
The risk groups for the appearance of a pigment spot or protrusion include:
- persons whose professional activities involve long-term exposure to ultraviolet rays, as well as regular stays in tropical and subtropical regions of the planet;
- people who regularly come into contact with various chemical substances, ionizing radiation and electromagnetic radiation;
- people of light phenotype;
- patients with immunodeficiency states;
- people whose relatives have a large number of pigment spots on their bodies;
- people who have been taking hormonal drugs for a long time;
- people who frequently injure their skin;
- women during pregnancy and breastfeeding;
- patients with endocrine pathologies.
Pathogenesis
The name "nevus" in translation from Latin means "spot", "defect". Directly pigmented nevus is a benign pigmented growth on the skin, which appears as a result of the accumulation of nevus cells. Such cells differ from other melanocytes in that they lack processes, do not share melanin with nearby pigment cells and have a slow metabolism.
During embryogenesis, melanocytes originate from the neural crest, after which they are transported to the area of their final localization point: the skin, organs of vision, etc. Pigment cells are localized in the basal epidermal layer, near the zone of unification with the dermal layer. From these structures, pigment nevus cells develop.
New, acquired pigment nevi are formed naturally, starting from the age of six months. The processes of formation of nevus growths are directly influenced by hereditary predisposition, excessive ultraviolet radiation, etc. [ 4 ]
Symptoms Pigmented nevus: intradermal, borderline, complex.
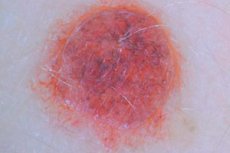
In most cases, a pigmented nevus looks like a flat or slightly raised spot. The color range is different: from different shades of black and brown to grayish-blue. The contours are clear and even, the surface is smooth. The average size fluctuates within 5 mm. However, larger specimens are also common - up to 10 mm and more. There are also known cases of giant nevi, which occupy large areas of skin. In some patients, nevus formations can be covered with papillomatous and warty growths. Sometimes hair grows through the spot.
The borderline type of nevus looks like a nodule and has a dry, smooth surface without hair. The outlines are even, less often - wavy. The most common sizes are 2-4 mm. It is not very prone to enlargement and color change, but is often multiple. The most common localization: soles, palms, genitals.
The blue type of nevus rises above the skin surface, can be hemispherical, with clear outlines and without hair. Common localization: face, arms, legs, gluteal area.
The risk of malignant transformation increases sharply if clinical signs of increased activity of the pigment spot appear.
The first signs of possible malignancy
You need to be careful not to miss the early signs of possible malignant degeneration of a pigment spot:
- acceleration of neoplasm growth;
- its compaction;
- the appearance of asymmetry in any part of the growth;
- the appearance of itching, tingling, tension, pain;
- change in pigmentation (in any direction);
- the appearance of redness around the border of the pigment;
- disappearance of hair from the nevus surface;
- the appearance of cracks and bulges;
- bleeding.
If any of the above symptoms or their combinations are observed, it is imperative to consult a doctor for adequate preventive and therapeutic measures. [ 5 ]
Pigmented nevus in a child
In newborn babies, these neoplasms are found relatively rarely, or are isolated. Upon reaching adolescence, such growths or spots are found in almost every child, and by the age of 25-30, their number can reach several dozen.
Most congenital pigment elements found in a newborn baby are small and single, representing a defect in the development of melanocytes. With age, the congenital spot usually increases in size without causing discomfort. The degeneration of the process can be suspected when signs of disproportionate development of the neoplasm or atypical changes appear.
Based on external characteristics, children's nevus elements are divided into small (up to 1.5 mm), medium (up to 2 cm), large (more than 2 cm) and giant.
Acquired pigmented nevi begin their development in early childhood. At first, a pigmented "point" of approximately 1-2 mm in diameter appears. Over time, it thickens, and a stalk may form. The predominant localization of the spot is the upper part of the body, head and neck. With the onset of puberty, the pigmented nevus often increases in size, darkens slightly. New elements are often added. In most cases, normal benign neoplasms do not increase in size to more than 0.5 cm in diameter, retain a uniform structure and color uniformity, contours, relief and symmetry.
In general, pigment spots change very slowly, over many months or even years, so they need to be monitored.
Stages
In its development, a pigmented nevus goes through several stages, ending with the processes of involution and fibrosis.
- Borderline pigmented nevus is characterized by the location of nevus structures at the border of epidermal and dermal tissue above the basement membrane.
- Complex pigmented nevus includes histological manifestations of both intraepidermal and borderline formation. Nevus structures gradually extend into the papillary dermal layer. Cell accumulations are also found in the dermis and epidermal layer.
- Intraepidermal pigmented nevus is characterized by the localization of nevus structures only in the dermis. This is the final stage of development of this neoplasm. During deepening into the dermis, the structures lose their ability to synthesize melanin. As a result, the growth loses pigmentation. This is why intraepidermal nevus is depigmented in most cases.
Forms
- Congenital pigmented nevus is of the following types:
- A spotted nevus, which has the appearance of a light brown spot 10-150 mm in diameter, contains dark brown spots or papular formations on its background.
- Pigmented melanocytic nevus – is found in 1% of infants, with giant pigmented nevus being registered in 1 out of 500 thousand newborns. In some cases, the neoplasm appears only a few weeks after the child is born. The preservation or loss of the skin pattern is noted: when the pattern is lost, this means that the cellular structures have penetrated the reticular layer of the dermis, forming a deep congenital melanocytic element. [ 6 ]
- Linear nevus is a congenital ectodermal anomaly characterized by the appearance of pigmented papules localized on the Blaschko lines.
- Acquired pigmented nevus can manifest itself in the following varieties:
- Blue nevus - has the appearance of a papule or nodule of a blue-dark color. Histology demonstrates focal melanocytic intradermal proliferation. In turn, there are three types of blue nevi: common, cellular and mixed pigmented nevus.
- Nevus of Setton (also known as halo nevus) is a melanocytic formation surrounded by a hypopigmented halo. The main factors causing the growth are regular trauma and excessive insolation. Spontaneous depigmentation is possible.
- Myerson's nevus has an eczematous rim around the circumference of the neoplasm.
- Ophthalmomaxillary nevus – characterized by impaired pigmentation in the area innervated by the ophthalmic and maxillary nerves. The growth contains melanin-rich melanocytes that have processes and are localized in the upper zone of the dermis.
- Dysplastic pigmented nevus consists of proliferating atypical melanocytes and is a spot or plaque growth of irregular configuration, with unclear outlines of a brownish or dark shade.
There are a number of pigmented neoplasms that can be both congenital and acquired. One example is a papillomatous intradermal pigmented nevus, which has much in common with a common papilloma. This is a benign element, often brownish, brownish or pastel in color, it can begin to develop at almost any age, from the neonatal period to old age. Papillary pigmented nevus is often large in size, most often found in the head or back of the neck.
Intradermal, intradermal pigmented nevus is the most common type of pigmented neoplasm. It is formed in the deep dermal layers, rises above the skin surface, has a dome-shaped configuration, and is sometimes covered with hair. Most often, its base is wide, but there are also elements on a stalk. The neoplasm is benign, but with frequent damage it can transform into a malignant tumor.
Unilateral pigmented nevus – congenital or acquired – is localized along the Blaschko lines, which correspond to the directions of migration and proliferation of mutant cellular structures during embryonic development. Other names for unilateral neoplasms: linear, segmental, Blaschkoid, Blaschkolinear.
In addition to the above classification, there are single (single) and multiple pigmented nevi, as well as various growths depending on their location:
- Pigmented nevi of the face are often located in the forehead or cheeks, less often on the temples and lips. Such neoplasms should be removed especially carefully, since the skin on the face is quite sensitive and thin. A pigmented nevus on the lip must be removed, which is associated with frequent trauma to the element and a high risk of malignancy.
- Pigmented nevus of the eye of the choroid is almost always localized on the back surface of the fundus, so it cannot be seen with the naked eye. The neoplasm can be examined using an ophthalmological examination, or if it is located in the equator area of the eye. The pathological element looks like a slightly protruding growth of a grayish shade, with clear outlines and dimensions of about 5 mm.
- Pigmented nevus of the conjunctiva appears inside or outside the mucous transparent membrane of the eye. The most common localization is the corner of the upper part of the eyelid or the corneal edge. The neoplasm is usually flat, with clear edges and dimensions of about 3-4 mm. Pigmented nevus of the iris, like conjunctiva, is well examined with a slit lamp.
Complications and consequences
According to experts, pigmented nevus can degenerate into melanoma under the influence of various risk factors, among which traumatic damage to the growth dominates. Although in some cases, melanoma can develop without previous trauma.
The actual frequency of malignancy of neoplasms has not been precisely established to date. Experts note that not every case of nevus growth ends in the development of a malignant process. For this reason, benign spots are classified as optional pre-malignant skin formations that do not necessarily degenerate, but have certain risks. Such types of nevus growths as complex, borderline, giant, blue and intradermal have a special tendency to malignancy.
Multiple pigmented nevi are considered a risk factor for the development of melanoma.
It is now well established that giant congenital nevi and malignant melanoma are associated, although the magnitude of the risk of malignant transformation is still the subject of considerable debate. Widely divergent figures range from 1.8% to 45%. A recent review [ 7 ] estimated that the incidence of melanoma in nevi larger than 2% of the total body surface area during the first 15 years of life is 8.52%.
Diagnostics Pigmented nevus: intradermal, borderline, complex.
Most often, diagnosis of nevus formations consists of examination of the body surface by a dermatologist. The specialist will pay attention to the shape, structural homogeneity, color range, location, hair growth, after which he will make a diagnosis and describe further actions.
In some cases, the diagnosis is controversial or ambiguous, so the doctor has to resort to additional diagnostic methods. A micropreparation and its cytological examination are rarely used, since the neoplasm is injured during the collection of biomaterial, which increases the risk of malignant degeneration. Such a study can be used if there are cracks, oozing, wounds and ulcers in the area of the pigment spot.
A safer method is considered to be fluorescence microscopy, reflective confocal microscopy [ 8 ], spectroscopy [ 9 ] and computer diagnostics, which involves obtaining an image of the spot with its subsequent characterization.
Laboratory tests are prescribed to determine the probability of the growth transforming into a malignant tumor. To do this, the patient gives blood for tumor markers - specific antigen proteins that are formed and released into the blood in the presence of a tumor process.
Instrumental diagnostics is most often represented by a histological examination, which helps to determine the type of pigmented nevus, the stage of its development, and the probability of malignancy. A macropreparation is obtained during the removal of the neoplasm and is immediately sent for diagnostics, where it is pre-processed and microscopically examined.
Based on the results of the histological examination, the specialist determines the type of the pathological element, in accordance with the cellular morphology. The thickness of the growth is measured in micrometers by measuring the longest diameter from the top of the element to the lowest (deepest) tumor cell.
Pathological anatomy of the biomaterial is important for differentiation of pigmented nevus and determination of further treatment tactics (if necessary). During the description, the following factors should be taken into account:
- histological affiliation;
- thickness of the neoplasm;
- presence of ulcers;
- marginal resection fields.
When melanoma is detected, the doctor prepares a pathological report and creates an individual further treatment plan.
Differential diagnosis
Pigmented nevus must be distinguished from many types of neoplasms on the skin, which can be either completely safe or life-threatening for the patient.
Thus, it is necessary to take into account the probability of development of the following skin elements:
- Benign (atheromas, lymphangiomas, papillomas, hemangiomas, lipomas, moles and nevi, fibromas and neurofibromas).
- Malignant (basaliomas, sarcomas, melanomas, liposarcomas).
- Precancerous or borderline skin elements (xeroderma pigmentosum, senile keratosis, cutaneous horn).
Nevus elements are often called by other terms - for example, moles, nevoid formations, birthmarks, etc. A mole or pigmented nevus are considered equivalent concepts when it comes to a congenital neoplasm.
Who to contact?
Treatment Pigmented nevus: intradermal, borderline, complex.
The treatment tactics for pigmented nevi are selected individually, but in most cases it is a radical removal of the neoplasm without the use of any kind of traumatic methods (for example, chemical burning). The most common methods of removal are considered to be the following:
- Surgery is a reliable method that does not require expensive equipment and can be used for any nevus variations. However, surgical treatment also has some disadvantages: for example, quite noticeable scars may remain after the operation. Most often, this method is used if it is necessary to remove a large pigmented nevus or a suspicious neoplasm with signs of malignancy.
- Laser removal of pigmented nevi is recommended for small formations located on any part of the body, including the face. The procedure is painless, the problem disappears almost without a trace, but the method is not recommended for large nevi. [ 10 ]
- The cryodestruction method can be used to remove small superficial spots. Cryodestruction involves exposure to liquid nitrogen: when exposed to a temperature of -196°C, the cells freeze, the growth is destroyed, a crust forms, which subsequently falls off. The procedure is slightly painful, and there are practically no scars.
- The electrocoagulation method is the opposite of cryodestruction and involves exposure to high temperatures. The coagulator loop is heated to a certain temperature and the tissue is cauterized, separating healthy tissue from the pathological focus. The advantages of this method include the elimination of bleeding, but the procedure is somewhat painful, so local anesthesia is required.
- The radiosurgery method involves the use of high-frequency radio waves. The removal of pigment spots occurs in a contactless manner, and the procedure itself is painless and safe.
The doctor decides which method of removal will be used in each specific situation, taking into account the size, type, and probability of malignancy of the pathological element.
After the procedure to remove the neoplasm, the doctor prescribes restorative treatment. The following external medications are used:
- A weak solution of potassium permanganate. To prepare the solution, take 100 ml of clean boiled water, add a few crystals of potassium permanganate, mix thoroughly until completely dissolved. The product is used for gentle treatment of the wound 2 times a day. A weak solution (2-5%) does not cause additional tissue irritation, but has the necessary antibacterial, drying and deodorizing effect.
- Levomekol ointment is an anti-inflammatory and antibacterial drug that is prescribed for external application daily for 4 days. If an allergic reaction develops after the first day of using the ointment, then further use of the drug should be discontinued.
- Propolis tincture is a natural preparation that promotes wound healing. It is applied locally in the form of applications or washes, twice a day for 5-6 days. In standard dosages, the tincture is non-toxic and well tolerated by patients.
- An alcohol solution of brilliant green is a well-known antiseptic and disinfectant that should be applied to the edges of the wound surface twice a day. A slight burning sensation may occur during treatment, which quickly passes. Allergic reactions are rare.
If all the doctor's recommendations are followed, the wound after the pigment spot is removed will heal quickly, leaving a small scar or depigmented area that will smooth out over time.
Prevention
A benign pigmented nevus does not pose a health hazard. The only risk is that the pathological neoplasm has a tendency to malignant degeneration. To prevent this from happening, it is necessary to monitor the condition of the pigment spot, observe its changes, and avoid injury. Doctors provide the following recommendations on this matter:
- Before going for a walk in sunny weather, you should use sunscreen or cover exposed areas of the body with clothing;
- You should not overuse tanning, including solariums;
- It is not advisable to use aggressive cosmetic procedures on the skin that can damage and injure tissue;
- If even the slightest suspicion of the formation of a malignant element appears, you should immediately consult a doctor.
If pigment nevi are already present, then you don’t need to worry too much, but you shouldn’t let the situation slide either. It’s enough to periodically visit a dermatologist or oncologist to monitor the formation. If the doctor deems it necessary, he will prescribe surgical or alternative removal of the problematic growth.
Despite the controversy, many clinicians agree that prophylactic removal of all giant and large hairy nevi is indicated.[ 11 ]
Forecast
Absolutely all pigment spots and dots on the skin require constant monitoring. Particular caution and attention should be shown in relation to neoplasms located on traumatic parts of the body, as well as to previously damaged, regularly growing and intensively changing nevus elements.
With timely removal of a suspicious or poorly located pigmented nevus, the prognosis is completely favorable.
If the patient refuses radical treatment of the formation, or its removal is not possible due to the complexity of its anatomical location, then it is necessary to strictly follow the doctor's recommendations: exclude possible damage to the pathological growth, protect it from sunlight, and regularly visit an oncologist-dermatologist.
When a pigmented growth becomes malignant, the prognosis depends on its size and location, the degree of spread to the lymphatic system, and the presence and number of metastases. The earlier the malignant tumor is detected, the more favorable the prognosis. The survival rate at an early stage of detection is 90-95%. The five-year survival rate for plantar melanoma is 82% for lesions up to 1.49 mm in size and 0% for lesions larger than 3.5 mm. [ 12 ]
Most nevus forms do not pose a danger to human health and life if they are not damaged, rubbed, irritated, and protected from ultraviolet radiation.
Pigmented nevus and the army
In the vast majority of cases, if a conscript has nevus neoplasms, he is not exempted from military service. However, sometimes a young man can still be exempted from conscription and assigned the category of "limited fitness" or "unfit for service". This is possible:
- if we are talking about a large benign growth that is “unfortunately” located on the body and is likely to interfere with wearing a military uniform and equipment, provided that it is impossible to remove it (there are contraindications confirmed by a doctor);
- if the malignancy of the neoplasm is confirmed.
- In order to find out whether they will take you into the army with a nevus growth, a young man should:
- visit a therapist, dermatologist and oncologist for consultation;
- collect the necessary certificates confirming the presence of a pathological formation;
- provide a medical card with a confirmed diagnosis and a doctor's report.
Pigmented nevus often requires increased attention to it and regular monitoring of the condition. Therefore, there is every chance to prove the need for systematic medical observation and the impossibility of military service - again, provided that there are contraindications to the removal of the pathological element.
